mieducation
Medical Use of Contact Lenses: A Review from BCLA CLEAR
In the eighth in a series of articles summarising the key findings of the BCLA CLEAR publication, a major review of the published evidence relating to all aspects of contact lens practice, Drs Karen G. Carrasquillo and Kellen Riccobono offer an overview of the section relating to the medical uses of contact lenses.
The BCLA CLEARmedical use of contact lenses publication provides a brief introduction to the types of contact lenses used in a medical setting and also defines certain relevant terminology.1 The report proposes the following definition for a medical contact lens: ‘a contact lens that is worn for the primary purpose of treating an underlying disease state or complicated refractive status.’
WRITERS Dr Karen G. Carrasquillo and Dr Kellen Riccobono
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Be aware of the indications for each use of medical contact lens (CL),
2. Recognise the subgroup of patients that benefit from medical CLs for visual rehabilitation,
3. Realise the mechanism of action for a variety of medical CLs,
4. Understand considerations when fitting medical CLs, and
5. Recognise the importance of patient education and review.
There are two subcategories of medical contact lenses:
1. Therapeutic contact lenses (also known as bandage contact lenses).
Defined as ‘lenses that are used for the treatment of ocular discomfort or to support the cornea during healing after surgery or when the cornea is being treated for an underlying disease state or to protect the cornea from the environment or mechanical interaction with the lids’.
2. Rehabilitative contact lenses.
Defined as ‘lenses that are prescribed for conditions that prevent a patient from achieving adequate visual function with spectacles because of high, irregular, or asymmetric refractive error. Partially or completely occlusive lenses that improve function or cosmesis after trauma, surgery, or stroke also fall into this category’.
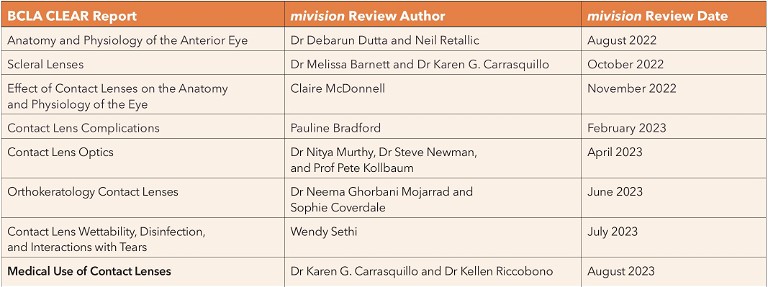
Table 1 summarises the indications for each use of medical contact lens, which will be discussed in more detail in the following sections.
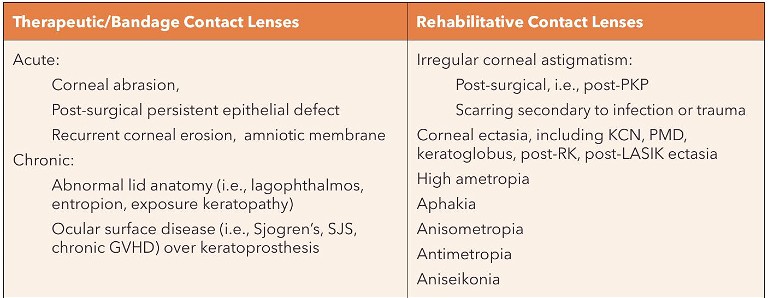
Table 1. Indications for the use of medical contact lenses. RK = radial keratotomy; LASIK = laser assisted in situ keratomileusis; PKP = penetrating keratoplasty; SJS = Stevens-Johnson Syndrome; GVHD = graft versus host disease; KCN = keratoconus; PMD = pellucid marginal degeneration.
BANDAGE LENSES IN AN ACUTE SETTING
As listed in Table 1, therapeutic contact lenses play a vital role in the management of acute ocular surface disease and/or corneal epitheliopathy.
Post-surgical The report discusses in detail the variety of surgeries that use therapeutic contact lenses to improve healing and provide improved comfort to the patient after the procedure. Evidence is cited of the safe and effective use of bandage contact lenses after the following procedures:
• Photorefractive keratectomy (PRK),
• Laser epithelial keratomileusis (LASEK),
• Phototherapeutic keratectomy (PTK),
• Epithelial-off corneal crosslinking (CXL),
• Ethylenediamine-tetraacetic acid (EDTA) treatment for band keratopathy,
• Phacoemulsification,
• Ptosis repair, and
• Bleb leaks, perforations, and penetrating wounds.
On the other hand, a summary of only equivocal evidence is cited for the use of therapeutic contact lenses after penetrating keratoplasty and pterygium repair.
Post-epitheliopathy Therapeutic lenses assist in the healing of acute epithelial damage by providing protection from external environmental factors as well as the mechanical interaction of the lids (Figure 1). By doing so, these lenses provide an environment in which the corneal tissue can heal without excessive desiccation and/or shearing forces from blinking, both of which can deter healing. This indication is relevant in certain clinical situations, including after persistent epithelial defects, recurrent corneal erosions, corneal abrasions, and over tissue adhesives after corneal perforations or over amniotic membranes.
Bandage Contact lenses
• Post cornea, lens extraction, or eyelid surgery to improve healing and comfort.
• For protection of those with corneal epithelial damage from corneal abrasions, epithelial defects, or recurrent corneal erosions.
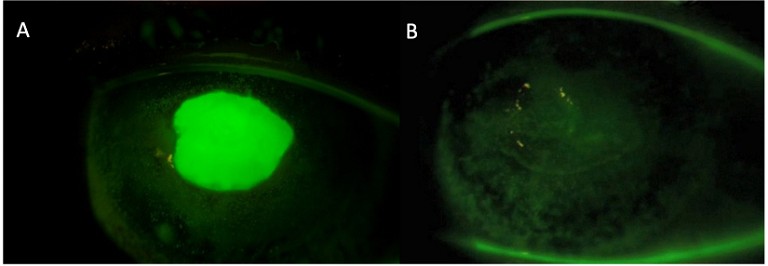
Figure 1. (A) Persistent epithelial defect secondary to neurotrophic keratopathy from herpes simplex virus and (B) healed after scleral lens wear. Image courtesy of Karen G Carrasquillo.
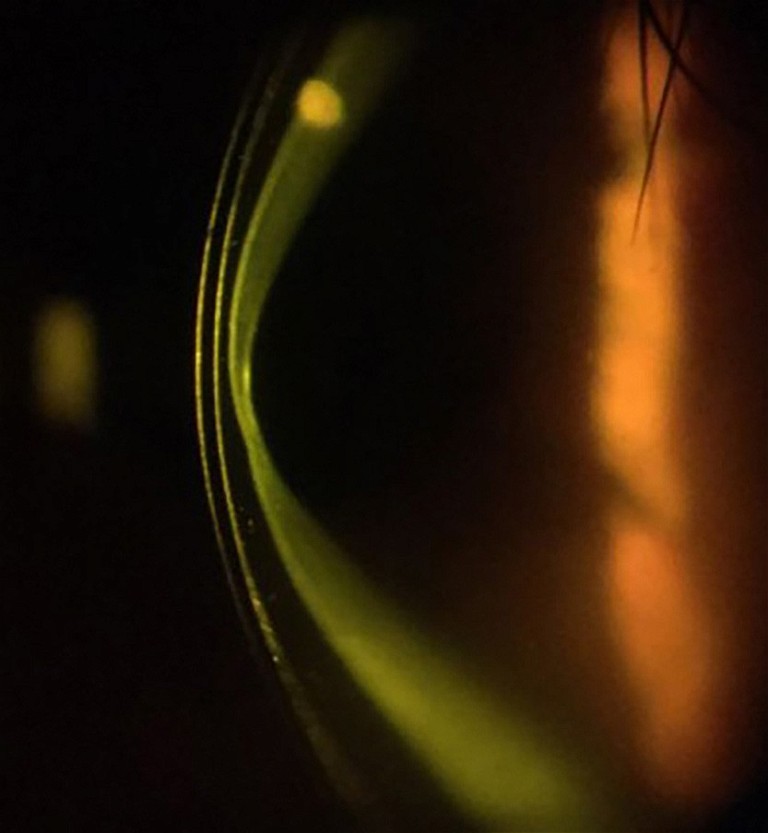
Figure 2. Secondary ectasia in Stevens-Johnson Syndrome. Image courtesy of Karen G Carrasquillo.
Refractive Error
In cases of high ametropia, antimetropia, anisometropia, aniseikonia, aphakia:
• Contact lenses provide improved vision and better contrast sensitivity over spectacles.
• Soft or rigid contact lenses can be used to best correct vision and to avoid amblyopia in paediatric patients.
• Contact lenses are sometimes used overnight in paediatric patients, though there is a risk of microbial keratitis.
• Contact lenses are especially important in unilateral conditions, where aniseikonia may be pronounced.
• Occlusive contact lenses can be used for unilateral aphakia when diplopia is present.
• Contact lenses improve binocular resolution and stereoacuity over spectacles.
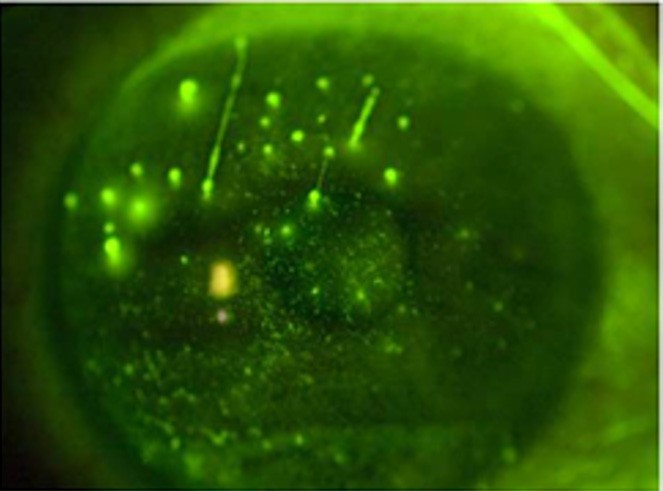
Figure 3. Filamentary keratitis in graft vs host disease. Image courtesy of BostonSight.
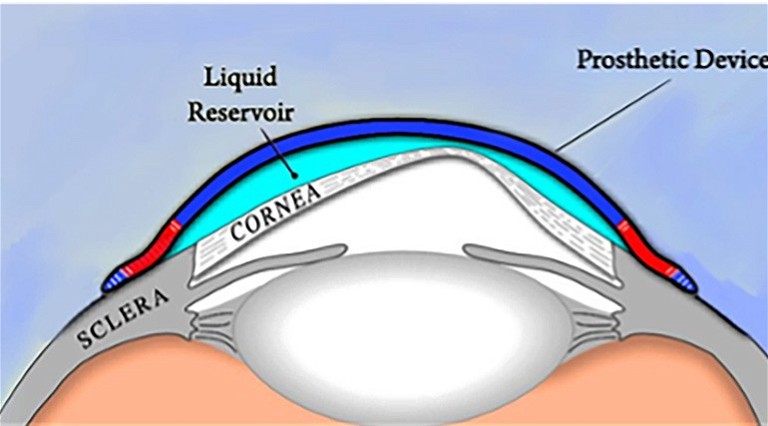
Figure 4. Schematic of scleral lens over irregular cornea. Image courtesy of BostonSight.
CONTACT LENSES FOR CHRONIC DISEASE
Based on the substantial evidence and literature, several chronic conditions are managed with contact lenses for medical use. These are outlined in Table 2.
CONTACT LENSES FOR VISUAL REHABILITATION
In some ocular pathologies, conventional corrective methods, such as glasses or conventional contact lenses, fail to provide the patient with functional vision. In these cases, medically necessary contact lenses can be vital for visual rehabilitation to provide the best visual function and quality of life (QoL).
A variety of contact lens types may be used depending on the condition, the severity of the disease, and the ability to reach a physiologically compatible and stable fitting lens. The categories of medically necessary contact lenses include rigid corneal lenses (RCL), specialty soft, hybrid (a lens with an RCL centre and a soft skirt), piggyback (an RCL fitted on top of a soft contact lens), and scleral lenses.
A large subgroup of patients that benefit from contact lenses for visual rehabilitation are those with corneal ectasias and/or irregular corneal astigmatism. These patients can suffer from poor visual acuity and function due to the irregular shape of the cornea. Rigid lenses, such as RCL or scleral lenses (Figure 4), can provide patients with improved vision by masking the underlying irregular cornea and providing a new and regular refractive front surface for the optical system.
Table 2. Chronic ocular surface disease conditions that may benefit from medical contact lenses.
(Click to view larger image)
Patients with high refractive error benefit from contact lenses due to the large prismatic effect and minification or magnification that can occur in glasses for these patients. Similarly, in anisometropic, antimetropic, and aphakic patients, contact lenses help reduce prismatic effects and aniseikonia.
TINTED OPAQUE OR PROSTHETIC LENSES
Cosmetic tinted lenses are designed to beautify the appearance of a healthy eye, and frequently used to enlarge the pupil or change the iris colour.
Therapeutic tinted lenses are used to treat an ocular disease or defect, and can be prescribed for glare, photophobia, to enhance colour vision, and for occlusion therapy in amblyopia.
Prosthetic tinted lenses improve cosmesis for an otherwise cosmetically abnormal eye. They are typically used in congenital abnormalities, disfiguring disease, and penetrating trauma.
Medical contact lenses are not only used for refractive error and visual clarity, but also for visual comfort. This is particularly important in the case of photophobia and glare after trauma or in the setting of ocular disease such as ocular albinism. Photophobia and glare can affect visual function and quality of life significantly, even if the patient has ‘normal’ visual acuity levels. Therapeutic contact lenses have been shown to improve photophobia and quality of life in both adults and children. In some cases, the contact lens is not only reducing photophobia but also improving cosmesis, particularly in cases of disfiguring disease or trauma. Figure 5 is an example of a patient who was successfully fitted in therapeutic tinted soft contact lenses to reduce photophobia after a fixed, surgical peaked pupil in the right eye.
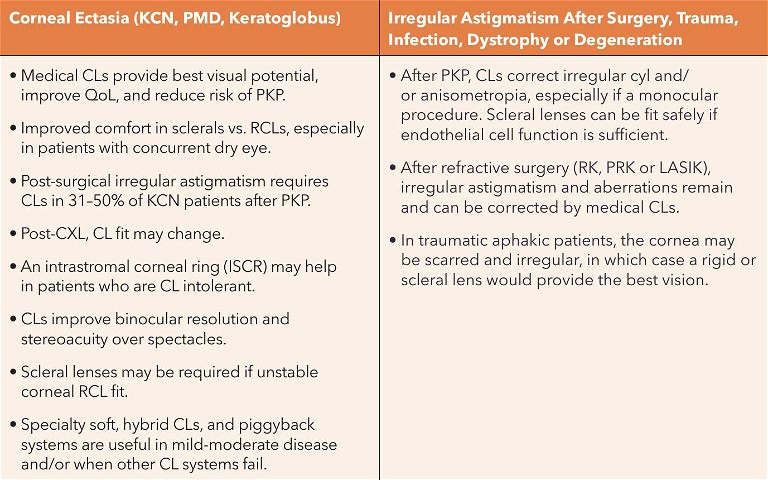
Table 3. Contact lenses for visual rehabilitation.

A

B
Figure 5. (A) A patient with an irregular pupil following retinal detachment repair surgery in the right eye. Note the peaked, surgical fixed pupil in the right eye on baseline. (B). A well colour-matched soft tinted lens was fitted in the right eye with an artificial pupil of the same size to match the left eye for best cosmesis and for best control of the patient’s symptoms of glare. Images courtesy of Kellen Riccobono.
Tinted or Prosthetic Lenses:
• Are useful for cosmetic reasons to give a more natural eye look for those with abnormalities or to simply beautify the appearance,
• Provide relief from symptoms such as glare, and photophobia,
• Can be used as part of a management strategy for amblyopia or colour vision enhancement.
Examples of conditions in which tinted lenses can be used:
• Retinitis pigmentosa,
• Cone dystrophies,
• Albinism,
• Traumatic aniridia,
• Peripheral iridotomy,
• Colour blindness,
• Disfiguring disease, and
• Amblyopia occlusive treatment for penalisation of the better seeing eye or in cases of intractable diplopia.
FOR OCULOMOTOR DYSFUNCTION
Evidence related to the benefits of contact lenses in nystagmus is scarce and equivocal. Most reports are retrospective studies and there is contradicting evidence in the ability of contact lenses to dampen ocular oscillation in nystagmus and improve visual acuity. The one prospective, randomised clinical trial studying the effects of both soft contact lenses and RCLs showed there was no benefit in visual acuity or dampening of ocular oscillation.
As it pertains to lid ptosis, at the time of the report’s publication, there was little evidence supporting the role that scleral lenses had in managing several types of lid ptosis, including ocular myopathy, complicated ptosis due to long term RCL wear, phthisis bulbi, and myopathy from Kearns-Sayre syndrome. There have been no long-term reports on the benefits and/or impact of scleral lenses in this setting. However, in one case report, Phillis et al. reported on the long-term impact (eight years) of using scleral lenses as a lid crutch to provide lid support in a paediatric case of a paralytic lid ptosis. They increased the sagittal depth and the lens diameter to raise the upper lid, distributed the weight of the tall lens over a larger surface area, and avoided complications of compression and suction.2 The scleral lens provided adequate visual improvement and lid support, and there were no complications of neovascularisation or oedema secondary to the high sagittal depth of the lens. Moreover, the cornea showed signs of clearing in corneal opacities over time, likely from the protection the scleral lens provides against chronic exposure.
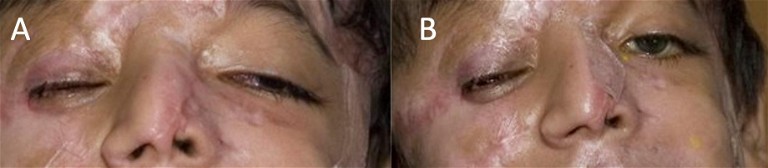
Figure 6. (A) Paralytic lid ptosis of the left eye. (B) Paralytic lid properly supported by a scleral lens used as a lid-crutch. Image courtesy of Karen G Carrasquillo.
WITH PROPHYLACTIC ANTIBIOTICS
Often medical contact lenses are used to treat anterior segment and corneal pathologies, such as corneal abrasions or persistent epithelial defects, where the risk of infection exists due to the nature of an open wound. In this case, it is standard for practitioners to treat with concurrent prophylactic topical antibiotics, typically those of a preservative free formulation, especially when using these drops in the fluid bowl of a scleral lens. While this practice is common, at the time of this report, there were no well controlled human studies to determine the true efficacy. There have been reports of soft lenses pre-soaked in gentamicin being able to provide an inhibitory concentration of gentamicin in the tear film for three days and when a combination was used for delivery into the anterior chamber. There is much to be explored, however prophylactic use of antibiotics – typically over a soft contact lens on the eye or inside the scleral lens reservoir before application on eye – is often used to reduce the risk of microbial keratitis along with close monitoring.
DURING THERAPY WITH OTHER AGENTS
Table 4 summarises the reports describing the concurrent use of topical therapeutic agents with contact lenses.
COMPLICATIONS OF MEDICAL USE
In cases of ocular surface disease, the compromised nature of the ocular surface or the severity of the disease may render these corneas more vulnerable or prone to complications during contact lens wear, including infection. As a consequence, more regular review may be advised.
However, the typical complications and risk factors are largely the same as for those who wear contact lenses for refractive purposes. Overnight lens wear increases the risk of infection further and the use of antibiotic prophylaxis may be prescribed. This is especially the case if corticosteroids are being taken for concomitant inflammatory disease, for example.
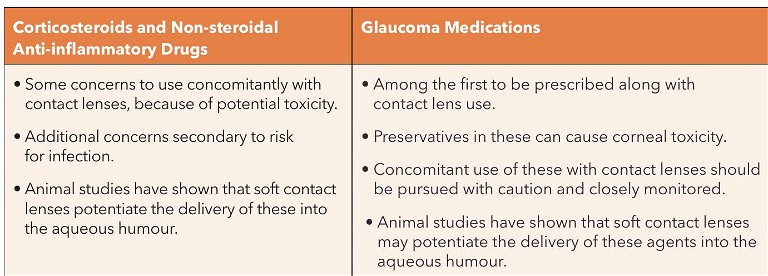
Table 4. Examples of concurrent use of topical therapeutic agents with contact lenses.
Complications with Contact Lenses for Medical Use
• Similar complications to those who wear contact lenses for purposes not related to medical reasons.
• Potentially more vulnerable to complications or may be associated with the underlying pathology.
Complications may, in some instances, be precipitated by the underlying disease. For example, corneal melt and perforation has been reported in patients with graft versus host disease wearing bandage soft contact lenses. However, this complication is likely due to the immune-mediated disease rather than to therapeutic lens wear.
PATIENT INSTRUCTIONS AND EDUCATION
Contact lens wearers should be educated on all aspects of lens care and handling, regarding application and removal aspects. Family members may also be trained to provide support. Wearing needs may vary depending on the reason for contact lens use and personal motivation.
Preserved multipurpose solutions that come with traditional gas permeable lens products can cause hypersensitivity reactions when medical contact lenses are being used to manage ocular surface diseases. Therefore preservative-free solutions may be preferred for disinfection, i.e., a hydrogen peroxide-based cleanser.
Compliance is another important aspect in the use of medical contact lenses to minimise and/or avoid complications. Education is important and regular reviews essential to maximise success and reduce risk.
When it comes to patient experience, evidence for the use of contact lenses for medical use is overwhelmingly positive. Numerous studies on scleral lenses report on improvement in quality of life, including activities of daily living, and visual function, amongst others. The same applies to soft contact lenses when used as bandage lenses, although not as overwhelmingly as scleral lenses.
In conclusion, there are many ways that contact lenses can be used in a medical setting to treat the ocular surface or provide the best possible visual potential.
To earn your CPD hours from this article visit mieducation.com/medical-use-of-contact-lenses-areview-from-bcla-clear.
This article is based on an original article published in the United Kingdom in Optician. The full report and supplementary information can be accessed at: doi.org/10.1016/j.clae.2021.02.002.
Wearing Schedules
• Most patients requiring medical contact lenses often wear them every waking hour.
• Various retrospective studies report the average scleral lens wear time to be around 12 hours.
• Overnight wear of therapeutic soft contact lenses (silicone hydrogels) or scleral lenses may be warranted at times. In each scenario, careful monitoring is required.
Five Clinical Pearls
1. Medical contact lenses for visual rehabilitation in the case of corneal disease can provide a significant improvement in visual acuity, visual function, and quality of life.
2. Contact lenses can be used as a bandage to the ocular surface to treat epithelial erosions, abrasions, or persistent defects to improve healing and patient comfort.
3. Tinted contact lenses can be beneficial – not only in the management of photophobia or glare but also in the improvement of cosmetic appearance after trauma and/or surgery.
4. Proper management and monitoring for adverse events, such as microbial keratitis with medical contact lenses, is vital.
5. Soft lenses may potentiate the delivery of topical therapeutics to the ocular surface and the aqueous humour.

Dr Karen G Carrasquillo FAAO FSLS FBCLA is Senior Vice President of Clinical and Professional Affairs at BostonSight. She is also an adjunct clinical professor both at the New England College of Optometry, and at the school of optometry, at the Massachusetts College of Pharmacy and Health Sciences. She is a Global Ambassador of the BCLA.

Kellen Riccobono OD FAAO completed a fellowship at the University of Houston College of Optometry in cornea and contact lenses. She is a Fellow of the American Academy of Optometry. She has worked at the BostonSight clinic as a PROSE provider as well as the New England College of Optometry as an assistant clinical professor. She currently works at an ophthalmology practice in San Marcos, Texas.

The Podcast of BCLA CLEAR – Medical use of contact lenses can be found by scanning the QR code or visit: podcasts. apple.com/cz/podcast/ bcla-clear-episode-6 medical-use-of-contactlenses/id1524673927?i= 1000549957771.
Original paper: Jacobs, D.S., Carrasquillo, K.G., Cottrell P.D., Fernández- Velázquez F.J., Gil-Cazorla R., Jalbert, I., Pucker, A.D., Riccobono, K., Robertson, D.M., Szczotka- Flynn, L., Speedwell, L., Stapleton, F., BCLA CLEAR – Medical use of contact lenses. Cont Lens Anterior Eye. 2021 Apr;44(2):289-329.
Acknowledgement and recognition to Deborah S. Jacobs, Paul D. Cottrell, Fernando J. Fernández-Velázques, Raquel Gil-Cazorla, Isabelle Jalbert, Andrew D. Pucker, Danielle M. Robertson, Loretta Szczotka-Flynn, Lynne Speedwell, and Fiona Stapleton who were the paper’s authors, and to the educational grants from Alcon and CooperVision.
The editors for this series are Neil Retallic and Dr Debarun Dutta.
References
1. Jacobs, D.S., Carrasquillo, K.G., Cottrell, P.D., et al. BCLA CLEAR – Medical use of contact lenses. Contact Lens and Anterior Eye 2021;44:289–329. doi.org/10.1016/J.CLAE.2021.02.002.
2. Phillis, K., Brocks, D., Carrasquillo, K.G., Case Report: Use of Prosthetic Replacement of the Ocular Surface Ecosystem Treatment of Traumatic Lid Ptosis in a Pediatric Patient. Optom Vis Sci 2020;97:1029–33. doi.org/10.1097/OPX.0000000000001612.