The MYOPIA ISSUE
mitechnology
Evolving Technologies
Spectacle Lenses for Myopia Control
Faced with a rapidly increasing prevalence of myopia across the world, and forecasts of half of the global population being myopic by 2050,1 soft contact lens companies rapidly adopted vision correction solutions demonstrated by research labs to simultaneously slow progression of myopia. Fast forward a decade and we are seeing spectacle lens solutions offering similar myopia control efficacy becoming increasingly available in clinical practice. Dr Paul Gifford explores the options.
WRITER Dr Paul Gifford
Contact lenses are a natural choice for myopia control research studies because they offer the simple advantage of tracking eye movements. Designing a distance power corrected central optic zone correction surrounded by plus addition powered zones creates a peripheral myopic defocus profile identified as being favourable to promote slowing of myopia progression.2 The contact lens moving with the eye ensures that the same optical profile is maintained in all gaze positions.
Spectacle lenses do not track with eye movements, a factor that is exploited for correcting presbyopia by using different parts of the spectacle lens to correct for different focussing distances. Early myopia research had shown that these presbyopia correcting spectacle lens designs provide a very small myopia control effect,3-5 which was attributed more so to them creating a partial defocus effect with the addition zone,6 rather than reducing accommodation demand. Peripheral defocus contact lens designs subsequently demonstrated greater myopia control efficacy,7,8 presumably benefiting from defocus being maintained across the whole periphery in all directions of gaze.
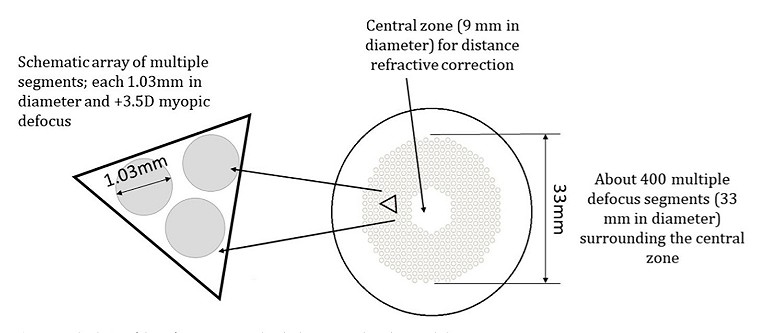
Figure 1. MiyoSmart spectacle lens design, from the open access paper.9
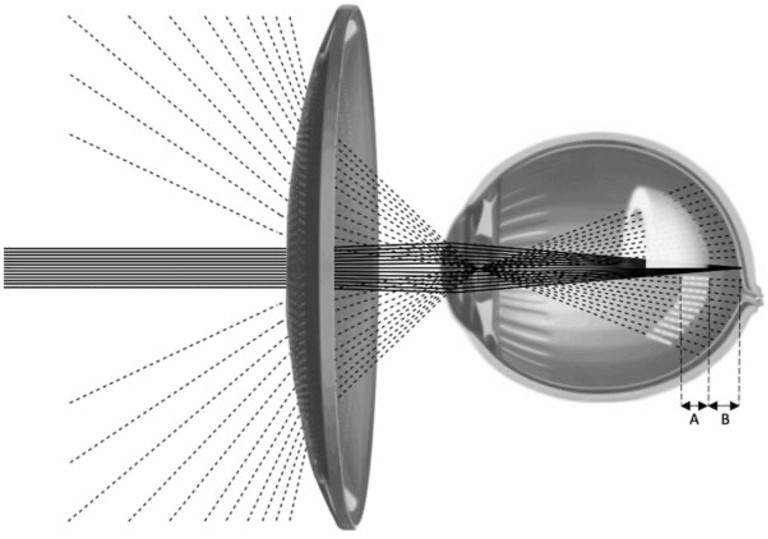
Figure 2. Stellest spectacle lens design, from the open access paper.10
Spectacle lenses are the traditional first consideration for vision correction in children, so it’s not surprising that research and development teams turned their attention to solving the difficult challenge of altering peripheral defocus in a spectacle lens while maintaining good foveal focus across all positions of gaze. This article investigates the incredible spectacle lens technologies that have been developed to overcome this problem: their design, principles of action, and comparative efficacy.
MYOPIA CONTROL SPECTACLE LENS DESIGNS
There are currently four spectacle lens designs that incorporate novel technologies for myopia control (Table 1). These are backed by peer reviewed, randomised controlled trials to demonstrate their efficacy and acceptability for children with myopia.
These designs are common in sharing a central single vision central optical zone surrounded by the adopted myopia control technology, and can be thought of as being like a single vision lens incorporating an overlaying ‘treatment zone’ for myopia control, with the following features.9-12
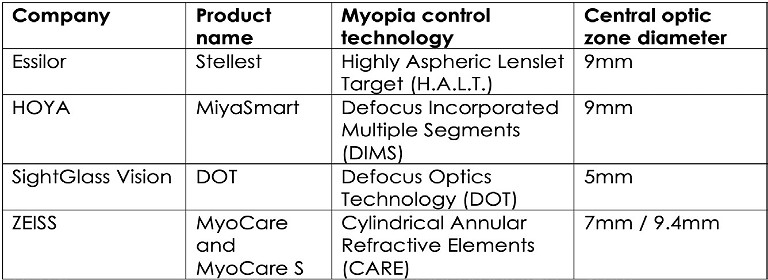
Table 1. Product names, myopia control technology, and optic zone diameters for novel technology myopia control specific designs.9-12
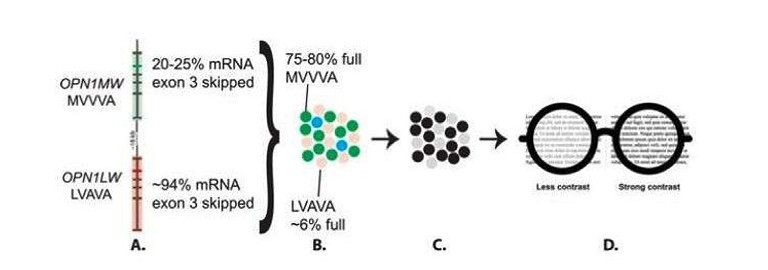
Figure 3. Foundational science leading to DOT lens design, from the open access paper.11
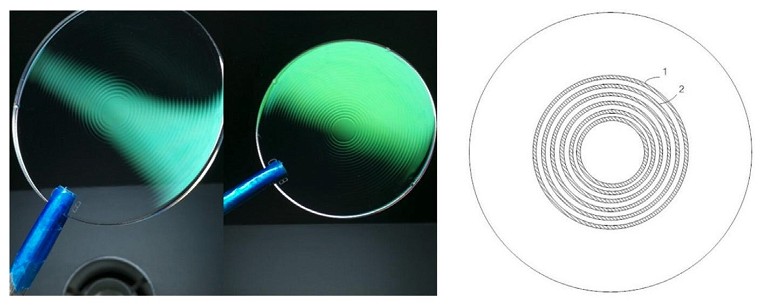
Figure 4. MyoCare lens design, from the open access paper.12
• The single vision carrier lens provides consistent refractive power across the entire lens to provide full correction at all gaze positions.
• All designs incorporate a central zone that does not include the myopia control component to allow best-corrected acuity and lens power verification.
• The overlaying myopia control technology surrounds the central zone:
– MiyoSmart and Stellest incorporate small diameter plus powered lenslets in a honeycomb or concentric ring array respectively.
– MyoCare incorporates rings of microcylinders.
– DOT incorporates a pattern of microdiffusers designed to alter contrast.
• In all designs, spaces between the lenslets, micro-cylinders or micro-diffusers allow consistent access to the single vision correction in all positions of gaze.
• MiyoSmart and Stellest lenslets have been shown to behave like a single vision lens and do not alter accommodation or binocular vision function.9,10 Early data for the DOT lens appears similar, with no data currently available for the MyoCare lens.
Further detail follows in the order of the first publication of the scientific data validating each design for myopia control in children.
HOYA MIYOSMART
The Defocus Incorporated Multiple Segments (DIMS) technology incorporated into MiyoSmart was designed by Hong Kong Polytechnic University. A single vision base provides refraction correction that incorporates a central 9mm diameter optical zone surrounded by a uniform pattern of 1.03mm diameter +3.50D powered lenslets out to a 33mm diameter (Figure 1).
The mechanism of action is described in the clinical trial for the DIMS technology incorporated into MiyoSmart: “This design simultaneously introduces myopic defocus and provides clear vision for the wearer at all viewing distances. There are multiple foci from myopic defocus at a plane in front of the retina, which would be received as blur images on the retina.”9
ESSILOR STELLEST
This lens features a single vision component providing full distance correction in all gaze positions and includes eleven concentric rings of 1.1mm diameter contiguous (touching) aspherical lenslets surrounding a 9mm clear zone. The geometry of aspherical lenslets has been calculated to generate a ‘volume of myopic defocus’ in front of the retina at any eccentricity, serving as a myopia control signal (Figure 2).
The mechanism of action is described in the clinical trial paper for the H.A.L.T. Technology incorporated into Stellest: “Instead of focusing light on two distinct surfaces, as in the case of competing defocus lenses, these aspherical lenses deviate rays of light continuously in a nonlinear manner that creates a threedimensional quantity of light in front of the retina.”10
SIGHTGLASS VISION DOT
Diffusion optics technology (DOT) lenses follow a different approach to the optical defocus theory for myopia control, and instead are based on research in people carrying genes linked to high myopia where cellular defects in cone photoreceptors were detected.
The researchers recognised that the photoreceptor defects caused adjacent photoreceptors to signal sharp contrast, which they attributed to being a contributing factor for myopia development. In the clinical trial paper, the authors stated that: “This observation suggests that abnormal contrast signalling between neighbouring full and empty cones may stimulate axial elongation.”11
Their suggestion is that urban living and spending more time indoors are high contrast environments that mimic the photoreceptor signalling created by the genetic mutation in hereditary high myopia. Children spending more time in these environments offer an explanation for the recent increase in myopia prevalence.
The DOT design incorporates thousands of micro-diffuser elements scattered across the single vision lens outside of a central clear 5mm zone (Figure 3). The microdiffusers are designed to reduce contrast without significantly affecting vision, thereby disrupting the high contrast environmentinduced photoreceptor signalling attributed to axial elongation and myopia progression.11
ZEISS MYOCARE
The MyoCare lens design was developed by the Wenzhou Medical University to target the optical defocus mechanism for myopia control. MyoCare has a common single vision refractive power that remains consistent across the lens and includes an array of annular mico-cylinders of +8.00D power spaced at 1.2mm intervals surrounding a 9.4mm clear zone (Figure 4).
The MyoCare design developers describe the design as: “When a flat light wave passes through the treatment zone of the lens, the resultant wave that emerges from the back surface of the lens has a consistent disturbance due to phase retardation from the micro-cylinders. These wave disturbances can be interpreted as higher-order aberrations which induce a blurred image on the peripheral retina.”12
TECHNOLOGY TRANSFER INTO CLINICAL PRACTICE
All these novel spectacle designs are common in using a single vision ‘carrier’ lens that provides distance vision correction in all gaze positions. The universally adopted clear central zone provides a primary gaze aligned area that is free from the myopia control components and allows the eye care practitioner to easily verify the single vision correction power of that spectacle lens. While the myopia control technology differs across the designs, they all incorporate spaces between the myopia control optical components that maintain access to the single vision correction in all gaze positions.

Table 2: Summary of efficacy outcomes for myopia control spectacle lenses, used with permission from the MyopiaProfile.com article, ‘The next generation -DIMS, H.A.L.T., DOT and CARE spectacle lenses for myopia control’. Note that the scientific terminology used for each lens design in its published paper is used here. DIMS = Hoya MiyoSmart, HAL = Essilor Stellest, DOT = SightGlass DOT lens, CARE = ZEISS MyoCare.
The optical power of the lenslet, microdiffuser or micro-cylinder components, is considerably different to traditional bifocal or progressive addition lens add power, because they do not provide a clear point of paraxial focus. Traditional bifocal or progressive lens adds form a clear point of focus that the eye can use instead of accommodating to achieve the same effect. Instead, the numerous myopia control optical components form myopic defocus patterns of varying effect, depending on design, that do not provide useful focus for the eye to use for distance or near vision. In this regard they cleverly enable the same defocus capability adopted in myopia control soft contact lens designs, which is maintained at all gaze positions across the lens without detrimentally affecting vision.
EFFICACY
Each of these four novel myopia control spectacle lens designs has been investigated in a randomised controlled trial (RCT), and outcomes reported for both refractive and axial length slowing of myopia progression. In evaluating the evidence of myopia control studies, it is crucial to look at RCT data to determine how well a treatment works compared to matched children wearing single vision correction. It is also crucial to look to axial length data for the most accurate and comparable evidence on myopia control efficacy, as axial length data is seen to be 10 times more sensitive than refraction in determining small changes in myopia.13
Table 2 provides a summary of the published data from the initial RCTs for these four lens designs. The MiyoSmart and Stellest RCTs were each published with two years of data, while the DOT lens and MyoCare RCTs have only reported one year data so far.9-12
It is important to note that Table 2 presents the absolute values for the refractive and axial length progression rates, for both the treatment and control (single vision = SV) groups in each study. These absolute values allow for evaluation of similarities, or otherwise, in the data. Another way that efficacy is typically described is with percentages, where the percentage reported is the overall ‘slowing’ effect that the lens design has had on the treatment group, compared to the measured myopia progression of the control group.
While a percentage efficacy is an important metric in understanding how well the treatment works in proportion to the control group, the percentage is relevant only to that study and cannot be directly compared to percentage outcomes from other studies. This is because the percentage is influenced by the duration of the study, the characteristics of the study population, and other factors.14
With a focus on the axial length treatment outcomes as the most accurate gauge of efficacy, these figures appear to show the following:
• The axial length progression of the control groups in each study appear broadly similar at 12 months, meaning that the study populations are broadly comparable.
• The axial length progression of the treatment groups at 12 months appears to show similarity of three lens designs, and a higher number (more progression) with one lens design. However, viewing data in this way does not allow for the conclusion that one or more designs are superior to others, as direct statistical comparison would be required.
WHICH SHOULD YOU PRESCRIBE?
Given that each of these lens designs has proven efficacy for slowing myopia progression, all are definitely a superior choice to a single vision correction for a child with progressing myopia. Prescribe the lens design which is available to you and best suits that child, and you will be prescribing an evidencebased myopia control solution. Variations in lens material availability and other features can also influence the prescribing choices of the individual eye care practitioner.
Whichever lens design you choose to prescribe, the most crucial factor in myopia control success is to encourage full-time wear.
In the Essilor Stellest study, the best results were obtained by children who wore their spectacles for at least 12 hours per day, seven days per week.10
LENS FITTING AND DISPENSING
The myopia control technology components of these lenses have been shown to have minimal impact on visual acuity and visual function, however optimum centration of the lens is crucial to ensure the best possible outcomes for the patient. The central optical zone of each lens design should be centred on primary gaze in natural head position, which means accurately measuring monocular pupil distance and height, just as for measuring centration of progressive addition spectacle lenses.
Research has shown that children typically adapt quickly and easily to wearing these novel lens technologies, within the first week or so.9,10 It is important to ensure a secure frame fit so that the child has a stable visual experience to permit easy adaptation. Educating parents and patients on the importance of regular frame adjustments can support understanding of these spectacle lenses as a treatment, not just as a vision correction.
THE FIRST OPTION FOR MYOPIA CONTROL?
These novel myopia control spectacle designs have broken the mold in achieving similar myopia control efficacy seen in the best soft contact lens designs and orthokeratology while maintaining good vision in all gaze positions. Since all children with myopia will need spectacles at some stage – even if wearing contact lenses part-time or full-time – it makes sense to consider myopia control spectacles as a first line treatment, especially for first correction or in younger children.
Dr Paul Gifford is a research scientist and the cofounder of My Kids Vision and Myopia Profile.
Dr Gifford’s expertise includes every facet of the optometry profession, from clinical practice to academia, research and industry. An Adjunct Senior Lecturer at UNSW and a consultant to the contact lens industry, he has won several prestigious research awards, published numerous scientific and educational papers, and lectured internationally.
References available at mivision.com.au