mitechnology
Corneal Biomechanics in Anterior Segment Disease & Refractive Surgery Screening
WRITER Dr Brendan Cronin
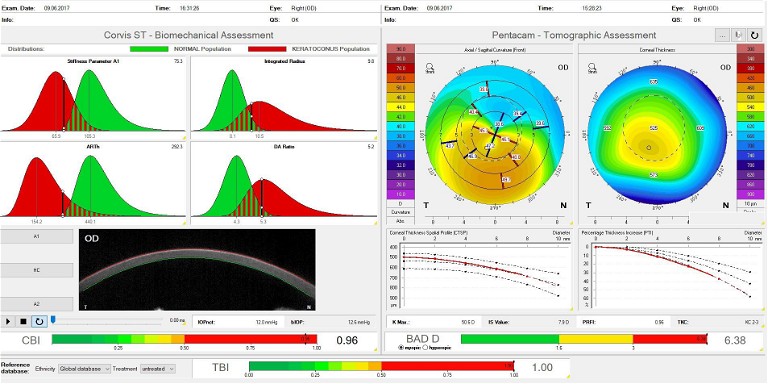
Figure 1. A report combining both topography and biomechanical indices for a patient with keratoconus.
The cornea’s role in maintaining visual acuity makes its structural integrity paramount in ocular health and disease management. Recent advancements in diagnostic technologies have propelled corneal biomechanics to the forefront of ophthalmic and optometric research and clinical practice. The Oculus Corvis ST has emerged as a pivotal tool in this realm, providing unprecedented insights into the dynamic mechanical behaviour of the cornea. This article aims to elucidate the role of corneal biomechanics, as assessed by the Oculus Corvis, in the diagnosis and management of anterior segment diseases, underscoring its significance in keratoconus, refractive surgery, and the burgeoning field of myopia management.
HOW THE CORVIS ST MEASURES BIOMECHANICS
Corneal biomechanics encompass the viscoelastic properties that dictate the cornea’s ability to withstand and respond to intraocular and external forces. Traditional assessment methods focussed predominantly on geometric, tomographic, and topographic metrics, often overlooking the cornea’s mechanical resilience and behaviour under stress.
Essentially, we have always assumed that if a cornea had a normal shape and thickness, then its biomechanics were normal. Similarly, if a cornea was thin or mildly ectatic, we have assumed that it was biomechanically normal. The introduction of the Oculus Corvis ST marked a paradigm shift in enabling clinicians to visualise and quantify the cornea’s dynamic response to a standardised air pulse.
The device’s high-speed Scheimpflug camera captures over 4,300 frames per second, detailing the cornea’s deformation and subsequent return to its original shape. This process yields critical data, including deformation amplitude, applanation lengths, and corneal velocities, painting a comprehensive picture of corneal biomechanical integrity. By integrating this information with traditional corneal measurements, eye care professionals can achieve a more holistic understanding of corneal health.
The combined biomechanic/tomographic assessment report provides one unified index with both detailed metrics on corneal shape and biomechanics, and a simple one number index of the corneal properties. This topographic biomechanical index (TBI) simplifies the delineation of normal from abnormal corneas for anterior segment conditions.
BIOMECHANICS IN DIAGNOSING AND MONITORING KERATOCONUS
Keratoconus, characterised by progressive corneal thinning and ectasia, exemplifies the clinical importance of biomechanical assessment. The disease’s insidious onset and variable progression necessitate sensitive and specific diagnostic markers. The biomechanical profiles generated by the Oculus Corvis ST have shown potential in identifying keratoconic corneas, even in the absence of overt topographic changes. This capability is particularly valuable in early-stage keratoconus, where conventional metrics may fail to detect subtle structural abnormalities.1
Moreover, the longitudinal monitoring of corneal biomechanics can offer invaluable insights into disease progression, aiding in the timely implementation of interventions such as corneal cross-linking. This procedure, aimed at enhancing corneal rigidity, underscores the therapeutic relevance of biomechanical understanding. By tracking biomechanical changes post-intervention, clinicians can gauge treatment efficacy and adjust management strategies accordingly.
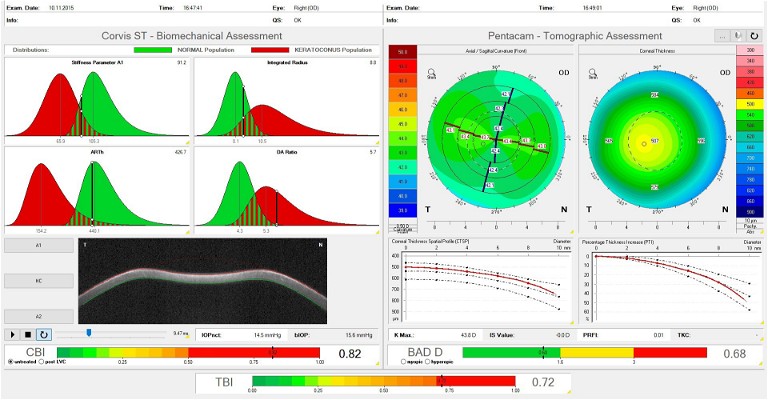
Figure 2. A combined report for a patient with normal topography but weak biomechanics.
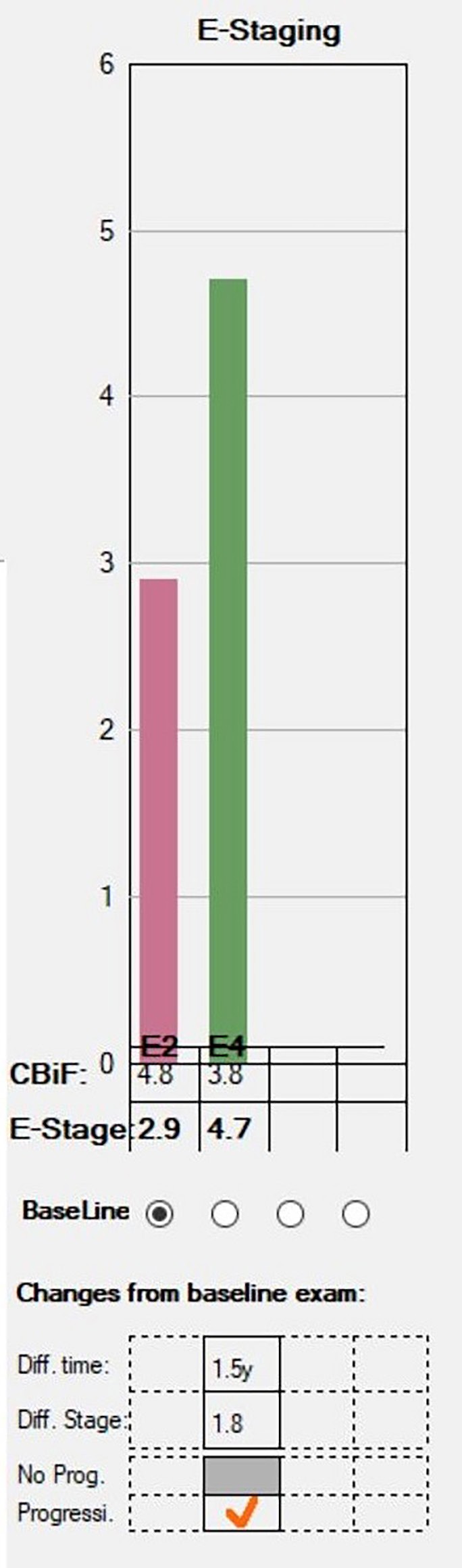
Figure 3. The Homburg Biomechanical E-Staging report showing statistically significant reduction in corneal rigidity in a patient with keratoconus.
The Homburg Biomechanical E-Staging report (Figure 3) on the Corvis allows the user to assess how the corneal biomechanics may weaken over time and therefore potentially accelerate progression. Again, this may assist in risk stratifying patients, particularly at their baseline presentation, into how likely they are to progress and how closely they need to be followed up.
BIOMECHANICS IN REFRACTIVE SURGERY
The success and safety of refractive surgery – such as LASIK, keratorefractive lenticule extraction (KLEx), and photorefractive keratectomy (PRK) – are inextricably linked to corneal biomechanical integrity. Preoperative biomechanical assessment can identify corneas at elevated risk of adverse outcomes, including post-LASIK ectasia, a complication characterised by progressive corneal steepening and thinning. The Corvis ST’s ability to discern subtle biomechanical vulnerabilities enables more informed patient selection and customised surgical planning, enhancing procedural safety and efficacy.2
Beyond individual risk assessment, biomechanical data can inform surgical technique adjustments, such as flap thickness and ablation depth, further personalising treatment to accommodate each patient’s unique corneal properties. This tailored approach optimises refractive outcomes while minimising the risk of biomechanically induced complications, embodying the principles of patient-centred care. The provided indices can also be used to detect subtle and sub-clinical post LASIK ectasia.3
For example, while a patient may fall below the range of what is typically considered safe for stromal thickness levels for laser eye surgery, their TBI may suggest that a PRK is well within safe biometric parameters. At an even more nuanced level, some software allows for a comparison of preand extrapolated post-laser biomechanics to determine an accurate risk profile of the development of post-LASIK ectasia.4
The role of biomechanics in keratorefractive lenticule extraction (KLEx) is even more fascinating. It demonstrates the wealth of new information we can glean from biomechanics and how we can use this to make procedures safer and more accurate. Biomechanics affect KLEx outcomes in three ways; ectasis risk as discussed above, the ease of lenticule extraction, and the accuracy of the refractive outcome.
As the technology for KLEx procedures accelerates, so will the number of surgeons performing the procedure and the number of patients having it. KLEx procedures, such as corneal lenticule extraction for advanced refractive correction (CLEAR), smooth incision lenticule keratomileusis (SILK ), SmartSight and small incision lenticule extraction (SMILE), all involve the dissection of a mid-stromal lenticule for refractive correction. Traditionally there have been two issues affecting this procedure; some lenticules are ‘sticky’ and difficult to remove, and the accuracy of refractive outcomes are slightly below those of LASIK. Both of these issues are significantly affected by biomechanics.
The risk of a difficult lenticule extraction can be predicted by biomechanics. The femtosecond laser settings for spot size, power, and overlap can then be adjusted to account for these differences, making the procedure easier for the surgeon and safer for the patient.5
Similarly, over or under corrections can be partially predicted by corneal biomechanics.
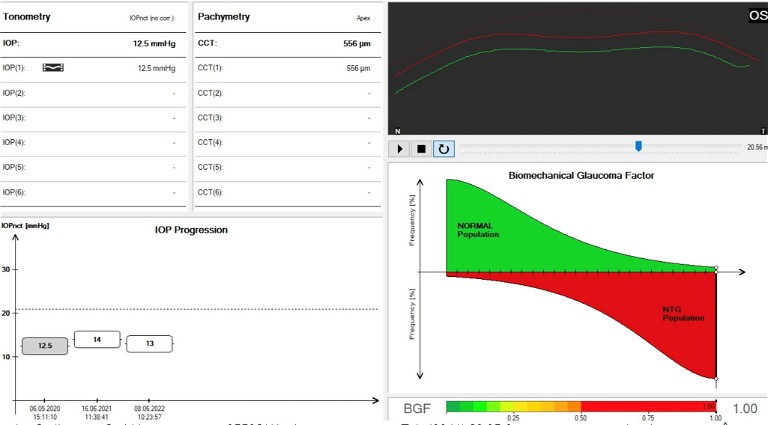
Figure 4. A glaucoma screening display showing a patient at very high risk of developing normal tension glaucoma. Note the normal IOP and normal central corneal thickness.
By incorporating biomechanics into their preoperative assessment regime, surgeons can adjust their nomograms to account for the predicted over or under correction associated with the specific properties of each patient’s cornea.6
THE FUTURE OF CORNEAL BIOMECHANICS
As we stand on the cusp of a new era in ophthalmology, the potential applications of corneal biomechanics continue to expand. The predictive value of biomechanical properties in assessing myopia progression risk represents a frontier in vision science. With myopia prevalence escalating globally, understanding the biomechanical underpinnings of its development and progression could revolutionise preventive strategies and therapeutic interventions.
Biomechanical metrics can correlate with myopia onset and axial elongation, offering a novel lens through which to view this widespread refractive error. Myopia control is a critical and expanding part of optometry practices. While Australia and New Zealand are arguably at the forefront of this rapidly evolving skill set, the ability to identify children who are at risk of both developing myopia and those who are more likely to progress would take myopia control to the next level of sophistication. Imagine being able to identify high risk patients and then being able to prevent the development of myopia before they even need refractive correction.7,8
While further studies are needed to unravel the complex interplay between biomechanical properties and why they correlate with myopic progression, understanding these may potentially pave the way for ground-breaking preventive measures.
BIOMECHANICS IN OTHER DISEASES
While this article has been focussed on the benefits of biomechanics in corneal diseases, the benefits of understanding biomechanics in glaucoma cannot be overstated. The Corvis ST provides information that can be critical in managing glaucoma. For example, corneal biomechanics can risk stratify patients who are at risk of developing normal tension glaucoma. Traditionally, normal tension glaucoma has been difficult to diagnose, however biomechanics can assist in predicting normal tension glaucoma risk with good sensitivity and specificity.9
Similarly, the biomechanically corrected intraocular pressure (bIOP) factors corneal strength properties into an IOP measurement that is independent of central corneal thickness.
This may provide information over and above that provided by traditional contact tonometry and facilitate better understanding of why some patients will progress despite what is considered to be adequate IOP lowering.10
The viscoelastic properties of the cornea also assist in determining patients who are at risk of structural and functional progression in people who are glaucoma suspects. Essentially, stiffer thinner corneas are at higher risk of visual field loss progression than thicker, softer corneas. A higher corneal stiffness is postulated to reflect a higher peripapillary scleral stiffness and therefore optic nerve head vulnerability. Much of the pivotal research in this area was done in Australia, highlighting how we are at the forefront of investigating and using the benefits of biomechanics to benefit patients.11
“As we stand on the cusp of a new era in ophthalmology, the potential applications of corneal biomechanics continue to expand”
CONCLUSION
The integration of corneal biomechanics into the fabric of ophthalmic practice marks a significant advancement in our approach to eye care. The Oculus Corvis ST stands at the vanguard of this movement, offering a window into the cornea’s dynamic resilience and susceptibility to disease. By harnessing the power of biomechanical assessment, clinicians can enhance diagnostic accuracy, tailor therapeutic interventions, better understand glaucoma progression, and potentially predict and prevent conditions such as myopia.
Dr Brendan Cronin is a corneal and refractive surgeon at the Queensland Eye Institute and Focus Vision. He performs all types of corneal transplant surgery, sutureless pterygium surgery, microincision cataract surgery, and LASIK.
References available at mivision.com.au