mitechnology
Allotex Allogenic Corneal Inlays
A New Frontier in Presbyopia Correction
WRITERS Dr Brendan Cronin and Dr David Gunn
There’s a new kid on the block for presbyopia management and it’s called Allotex. This allogenic corneal inlay is a biological, minimally invasive implant that restores near vision without sacrificing distance acuity or resorting to intraocular surgery. Drs Brendan Cronin and David Gunn believe this inlay is an attractive option for both patients and eye care providers seeking a balanced, low-risk presbyopia solution.
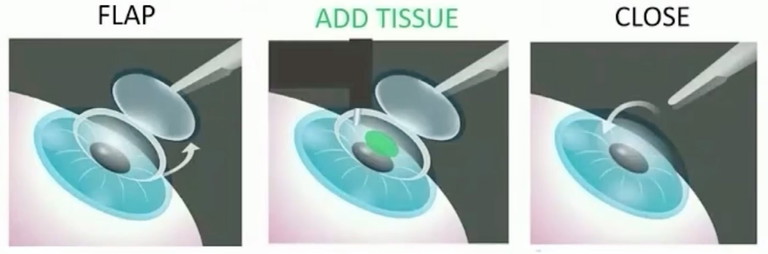
The Allotex surgical procedure.
Presbyopia affects nearly 1.8 billion people globally,1 reducing quality of life by impairing near vision in people over 45. For emmetropic presbyopes, or those with minor refractive errors, the challenge is unique: they enjoy good distance vision but find near tasks increasingly difficult. Traditional options like reading glasses, monovision LASIK (laserassisted in situ keratomileusis), multifocal contact lenses, and refractive lens exchange all have drawbacks. Glasses offer a solution but are not what a refractive patient is looking for. Monovision LASIK compromises binocular function. Multifocal IOLs require intraocular surgery and corneal laser options like PresbyLASIK may be irreversible.
A SAFE, PROVEN BIOLOGICAL APPROACH
Allotex builds on the proven safety and efficacy of allogenic corneal tissue used in procedures like CAIRS (corneal allogenic intrastromal ring segments) for keratoconus. CAIRS are ring-shaped allogenic implants that have demonstrated excellent outcomes in reshaping the cornea and improving visual acuity in keratoconus and other corneal ectasias. Compared to synthetic intrastromal rings, CAIRS show lower rates of inflammation, haze, and longterm complications due to their biologic compatibility.
This success supports the broader use of allogenic corneal implants in refractive surgery. Unlike synthetic inlays previously marketed for presbyopia, which were ultimately ceased due to complications,
Allotex inlays are made from decellularised, radiation-sterilised, donor corneal collagen. This material integrates well with host tissue, avoiding adverse immune reactions or metabolic disturbances and ensuring greater long-term stability and safety.
DESIGN AND PLACEMENT
The Allotex inlay is a transparent, 20 micron thick, ~2.5 mm diameter disc, shaped using an industrial excimer laser and optical coherence tomography (OCT) guidance. While the implant is 20 microns thick, it tapers to a sub one micron thickness at its edge. The disc is implanted under a femtosecond-created LASIK flap in the non-dominant eye. Its curvature and optical properties are designed to increase depth of focus by introducing specific higher-order spherical aberrations. This enhances near and intermediate vision while preserving distance acuity, functioning similarly to extended depth of focus intraocular lenses (EDOF IOLs) but without entering the eye. Allotex works with United States based tissue banks to utilise tissue that is only useful for lamellar transplantation, so that corneal transplant reserves are not depleted.
The surgical procedure involves creating a LASIK flap 120 microns thick. The flap is lifted, and the inlay is positioned directly over the pupil on the stromal bed. After positioning, the flap is repositioned, securing the inlay beneath the surface. There is no ablation of corneal tissue (unless a concomitant ablation is performed), and there is no change to the natural crystalline lens. The procedure is entirely additive and reversible.
BIOCOMPATIBILITY AND REVERSIBILITY
A major advantage of the Allotex inlay is its biological composition. Being made of human collagen, the inlay blends into the cornea without eliciting foreign body responses. Patients generally do not experience haze, thinning, or interface scarring; issues that plagued synthetic inlays.
In the rare event that a patient does not adapt to the visual result, the inlay can be removed. Removal is performed by lifting the LASIK flap and gently irrigating or peeling away the inlay.
WHO BENEFITS MOST?
Allotex inlays are particularly well suited to:
• Emmetropic presbyopes who wish to regain near vision without glasses,
• Patients with low levels of hyperopia or myopia not warranting lens surgery (-3.00D to +2.00D),
• Those intolerant of monovision corrections,
• Individuals wary of permanent or intraocular solutions, and
• Pseudophakic patients with monofocal lenses seeking an improvement in near vision.
This demographic has previously had limited satisfactory options. Allotex fills that niche by offering a solution that preserves distance vision, avoids intraocular risks, and can be removed if desired.
CLINICAL OUTCOMES: THREE-YEAR DATA
A prospective three-year study published in the Journal of Cataract and Refractive Surgery1 evaluated 25 patients (50 eyes) who underwent implantation of Allotex inlays in their non-dominant eyes. The study provides strong evidence of efficacy, safety, and stability.
Key Results
Near Visual Acuity (UNVA): Mean UNVA in treated eyes improved significantly to 0.10 logMAR (6/7.5 approx. J2), compared to 0.56 logMAR (approx. 6/21) in untreated eyes.
Distance Visual Acuity (UDVA): No significant difference between treated and untreated eyes. Mean UDVA was 0.07 logMAR vs. 0.03 logMAR, respectively (both approximately 6/6).
Corrected Distance Visual Acuity (CDVA): Minimal change in CDVA. Six out of 25 eyes lost one line of CDVA.
Depth of Focus: Treated eyes achieved 2.8D of depth of focus compared to 1.1D in untreated eyes.
Spectacle Independence: Of 25 patients, 22 patients reported complete freedom from reading glasses at three years.
Complications: There were no cases of corneal haze, rejection, or epithelial ingrowth. No inlays required explantation due to medical complications.
These results suggest the Allotex inlay significantly improves near vision and depth of focus without compromising distance vision and does so safely over a multi-year period.
COMPARISON TO OTHER PRESBYOPIA SOLUTIONS
Monovision LASIK adjusts one eye for near and one for distance. While effective for some, it can reduce stereopsis and cause adaptation difficulties. The Allotex inlay, by enhancing depth of focus in one eye without inducing significant myopia, preserves distance acuity and binocular function.
Refractive lens exchange (RLE) replaces the natural lens with a multifocal or EDOF IOL. This permanently removes accommodation and introduces risks associated with intraocular surgery. For emmetropic presbyopes without cataract, RLE may be unnecessarily invasive. Allotex offers a noninvasive alternative that retains the natural lens.
PresbyLASIK reshapes the cornea to create a multifocal surface. It is irreversible and may affect night vision and contrast. Allotex achieves a multifocal-like effect through spherical aberration without tissue ablation.
Pharmacological drops such as pilocarpine provide temporary pupil constriction to improve near vision. These offer limited duration, require ongoing application, and may cause brow ache or reduced night vision. Allotex offers a stable, long-term effect in a one-time procedure.
PATIENT EXPERIENCE AND VISUAL QUALITY
Patients report a high degree of satisfaction. The treated eye retains usable distance vision (~20/25), with improved intermediate and near acuity. Binocularly, most patients function with excellent vision at all ranges. Depth perception is maintained, and night vision disturbances are rare due to the inlay’s optical clarity and matched refractive index.
Adaptation time varies, but most patients adjust within weeks. Counselling and setting expectations are crucial as epithelial remodelling can take some months for the distance vision to stabilise. The reversible nature of the procedure provides peace of mind.
CLINICAL INTEGRATION AND WORKFLOW
For practices already performing LASIK, integrating Allotex requires minimal change. The femtosecond laser and flap creation process are familiar. The inlay is provided sterile and ready-to-use. Postoperative care mirrors LASIK: short-term antibiotics, anti-inflammatory drops, and dry eye management.
Patient selection is key. Ideal candidates are:
• Aged 45–65,
• Motivated for spectacle independence,
• Free of ocular surface disease or keratoconus, and
• With a stable refraction and healthy corneas.
Preoperative measurements should include topography, aberrometry, and pupil evaluation under different lighting and cycloplegic refraction. Dominance testing helps select the correct eye. Educating patients on the expected benefits and adaptation phase improves satisfaction.
SUMMARY
Allotex allogenic corneal inlays offer a new, biocompatible solution for presbyopia in emmetropic and mildly ametropic patients. Key benefits include:
• Significant improvement in near vision and depth of focus,
• Preservation of distance vision and stereopsis,
• Reversibility and minimal invasiveness, and
• Excellent biocompatibility and longterm safety.
These features make Allotex an attractive option for both patients and eye care providers seeking a balanced, low-risk presbyopia solution.

Dr Brendan Cronin and Dr David Gunn.
Dr Brendan Cronin MBBS (Hons) DipOphthSci B.Com LLB FRANZCO is an ophthalmologist and the Director of Education at the Queensland Eye Institute. He is also a Senior Lecturer at the University of Queensland.
He is a member of The Royal Australian and New Zealand College of Ophthalmologists and the European Society of Cataract and Refractive Surgery. He has a special interest in diseases of the cornea and anterior segment including, cataract surgery, corneal transplant surgery, pterygium surgery, keratoconus surgery, and laser refractive surgery.
Dr David Gunn MBBS (Hons I) BSc CertLRS FRANZCO FWCRS is a Brisbane-based ophthalmologist specialising in cornea, cataract, and refractive surgery. He has a research focus in laser eye surgery and advanced keratoconus treatments. He introduced CAIRS surgery to Australia in 2021 and has performed several Australian and world first procedures in the area of keratoconus. He practises at the Queensland Eye Institute and Focus Vision Clinic.
References
1. Fricke TR, Tahhan N, Naidoo KS, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: Systematic review, meta-analysis and modelling. Ophthalmology, 2018;125(10):1492-1499. doi: 10.1016/j.ophtha.2018.04.013.
2. Keskin Perk FFN, Taneri S, Kilic A, et al. Increasing depth of focus with allogeneic presbyopic inlays: 3-year results. J Cataract Refract Surg. 2023 Oct 1;49(10):1005-1010. doi: 10.1097/j.jcrs.0000000000001270. PMID: 37487178.