miophthalmology
BCLA CLEAR Presbyopia:
Management with Spectacles
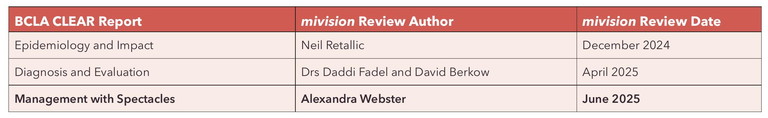
In the third article of a series encapsulating significant conclusions from the BCLA CLEAR Presbyopia publications, Alexandra Webster provides an overview of spectacle management options for presbyopia, along with a summary of the history, market data, future possibilities, and clinical considerations. The content is based on insights from the BCLA CLEAR publication, Presbyopia: Management with Contact Lenses and Spectacles.1
WRITER Alexandra Webster
LEARNING OBJECTIVES
On completion of this CPD activity, participants should:
1. Realise the many different solutions for presbyopia using spectacles,
2. Be able to use clinical findings, patient information, and task analysis to guide lens choice,
3. Realise the importance of patient communication to set expectations, and
4, Understand the importance of measurements and manufacturers’ guidelines when dispensing.
The correction of presbyopia by spectacles is an under-researched area of eye care practice. Although there is much anecdotal and textbook information available, few studies have explored clinical decision making or comparison of different options. Therefore, much of the information available is derived from theoretical optical knowledge and practical experience.
The demand for presbyopic visual solutions cannot be understated. With nearly two billion presbyopes wordwide currently,2 and an expectation that more people will be living and working longer with complex visual demands, the need for suitable, presbyopic solutions is paramount.
A BRIEF HISTORY
Presbyopia can be seen as the challenge that initiated the invention of spectacles, with curved glass initially used to provide magnification. Many centuries later, developments came with ‘multifocal’ spectacle lenses being designed to satisfy the need for ametropic presbyopes. Arguably the most famous was Benjamin Franklin who designed the first bifocal in around 1760 – the Franklin Split. Later, in 1827, the trifocal was patented by John Issac Hawkins. However, it was not until 1959 that the first progressive lens was commercially available, known as the Varilux lens and developed by Bernard Maitenaz. From that point on, progressive lens designs have advanced significantly, with free-form surfaces enabling superior lens solutions. Although available data is limited, it is estimated that by 2028 the overall market for spectacle lenses will be US$62.4 billion, with progressive lenses expected to account for about 60% of the world spectacle lens market.1
CLINICAL EXAMINATION CONSIDERATIONS
Clinical examination success comes from understanding individual patient needs in conjunction with analysis of their refractive requirements. The definition of presbyopia outlined in BCLA CLEAR Presbyopia: Definitions, supports this dual consideration:
“Presbyopia occurs when the physiologically normal age-related reduction in the eye’s focussing range reaches a point that, when optimally corrected for far vision, the clarity of vision at near is insufficient to satisfy an individual’s requirements.”3
A full patient history should be undertaken, including previous discussions on correction solutions, their success/failure, and why. It is also necessary to obtain information about the patient’s lifestyle and occupation, and to perform a task analysis; this is a recurring theme of the paper. The BCLA CLEAR Presbyopia: Evaluation and Diagnosis paper provides a detailed exploration of refractive requirements and approaches.4 There is a particular need to consider the patient’s amplitude of accommodation in conjunction with their ametropia, as this will influence their management requirement (Figure 1). The determined add will require further consideration during the dispensing process.
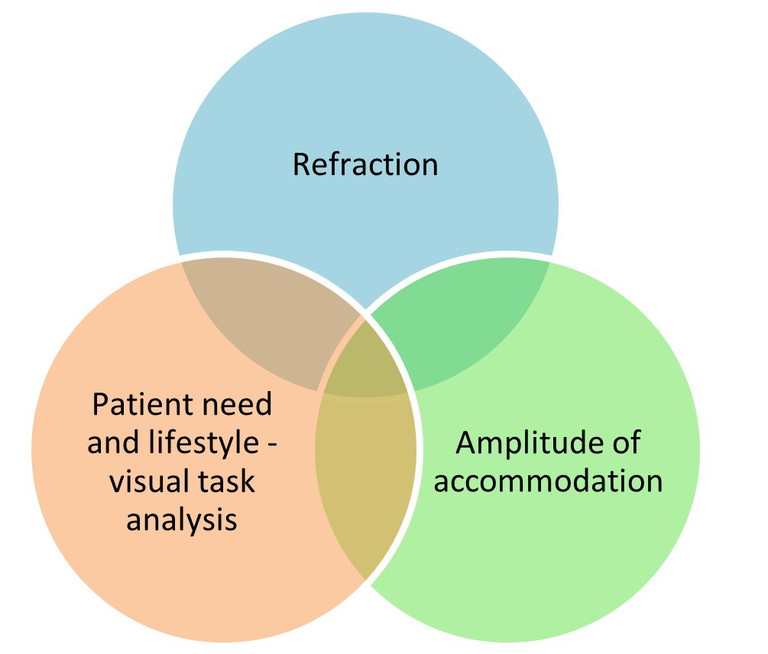
Figure 1. Requirements for managing the presbyope with spectacles.
SPECTACLE SOLUTIONS FOR PRESBYOPIA
Eye care practitioners can choose from a virtual apothecary of spectacle lens forms, designs, materials, tints, filters, and surface treatments to provide their presbyopic patients with the most suitable visual solution(s). On a basic level, presbyopic spectacle lenses can be placed into three categories: single vision, multifocal (bifocal/ trifocal), and progressive surface lenses. However, with modern lens surfacing techniques, the lines are somewhat blurred (excuse the pun), for example, a bifocal surface and a progressive surface can now exist in one lens design.
“Presbyopia can be seen as the challenge that initiated the invention of spectacles, with curved glass initially used to provide magnification”
SINGLE VISION SPECTACLES
This monofocal option is arguably the most versatile, with all lens materials, forms, tints, filters, and surface treatments available. Providing a comparatively large field of view, single vision (SV) lenses may be prescribed following a task analysis for a distance, near or occupational-specific correction. A UK sample of SV wearers has shown near spectacles to be the most utilised by presbyopes, but distance spectacles are worn for a greater proportion of time.5 SV spectacles can be an option for those wanting a near or occupational-specific correction over distance contact lenses (CL), for patients fitted with distance-only intraocular lenses, or for patients using multifocal or monovision CLs.
Communication issues are a known contributor to spectacle non-tolerance, which includes patients wearing SV near spectacles and expecting to be able to see in the distance. Practical application of the near addition, then asking the patient to view in the distance to experience the limitations of this correction option, may support a better patient understanding before dispensing. The need to remove SV spectacles or swap pairs for different tasks should be broached with the patient to assist their decision making. Keep in mind that subjective quality of vision scores has been shown to decrease as time spent wearing SV near correction increases, potentially contributing to the need to change or remove spectacles.5
Though SV ready-made reading spectacles are widely available, these should only be considered in an emergency or in countries where access to prescribed spectacles is limited. A UK-purchased, random sample of ready-made reading spectacles showed that 42% did not conform to international optical standards, particularly owing to induced horizontal and/or vertical prism.6
MULTIFOCAL SPECTACLES
Bifocals
Bifocal spectacles are available in a range of segment types (Figure 2), materials, tints, and filters. Two distinct focal distances can be viewed – often distance and near – but can be need-specific e.g. intermediate and near. Free-form technology now enables new bifocal surfaces to be manufactured, including blending between the segment and main lens portions to create non-visible segments and hybrid designs where a progressive blend is used to replace the bifocal segment top.
Dispensing considerations for bifocals include selection of the segment type and size, and positioning of the segment top. These should be tailored to the individual’s requirements. Segment top positioning is recommended at the lower edge of the iris or the top of the lower lid for small round segments and 2 mm below the top of the lower lid for straight-top segments (Figure 3). However, this may be modified for a number of reasons, including intended use, non-standard posture, or to match a previously satisfactory fit.
Image jump must be considered and covered in patient communication. This is when the wearer experiences a sudden movement or ‘jump’ of the object being viewed into their near field of view. It is a phenomenon associated with the near segment, so thought needs to be given to the segment type and power (Figure 4). E-line and cemented/bonded (modern Franklin Split) bifocals are considered ‘no-jump’ as they do not induce base-down prism, with the optical centre of the segment found on the dividing line. Image jump in bifocals may be a risk factor for falls in older patients with downwards viewing, for example when walking downstairs.7 Useful advice to patients is to tuck their chin when looking down, so the distance portion of the lens is accessed, for example when walking downstairs.7
Trifocals
Favoured more in the United States than Europe, trifocals have further limitations on availability than bifocal lenses but can be sourced in a number of materials and finishes. The trifocal provides three distinct areas of corrective power, commonly for distance, intermediate, and near viewing, though they can be modified for occupational need; both in power and segment placement. A range of different configurations of trifocal segment sizes, shapes, and positioning is available (Figure 5).
POWER VARIATION LENSES
These are spectacle lenses with ‘a smooth variation of focal power over part or all of its area, without discontinuity, designed to provide more than one focal power’. This definition, therefore, includes traditional or full progressive addition lenses (PALs), alongside occupational progressive lenses, degressive, and low addition lens designs.
Full Progressive Addition Lenses
As stated earlier, the progressive lens market boasts the lion’s share of presbyopic spectacle sales. Traditional or ‘full’ PALs provide a corridor of increasing power between a far and near zone, providing the wearer with the advantage of being able to see distance through to near vision in one pair of spectacles. This is achieved as a seamless, progressive surface, which creates oblique surface astigmatism in the lateral areas of the lens. Effectively, a corridor of vision is generated where, according to the Minkwitz rule, increasing astigmatism is produced perpendicular to the increasing lens power.8 The subjective effect of the resultant oblique astigmatism can be referred to as a ‘swim’ effect as the head is moved, as well as reducing peripheral field of view increasingly so as the wearer accesses the intermediate/near portions of the lens. The vertical placement of the distance correction in the upper portion of the lens gradually moving through the correction zones, combined with the peripheral vision limitations, means that the wearer needs to move their head to access clear vision depending on the task they are performing. For patients working on digital devices, this can result in neck and/or back strain.
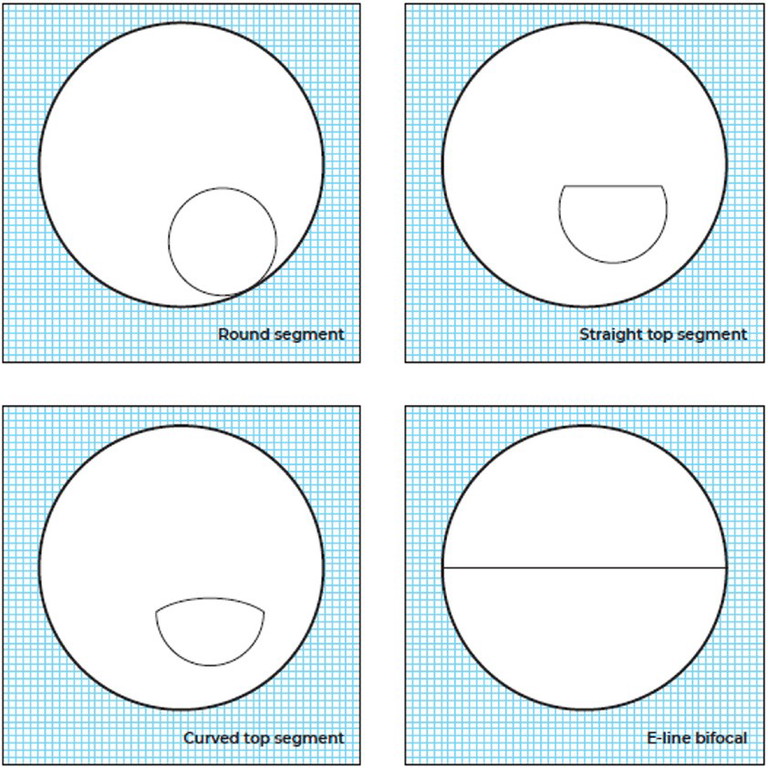
Figure 2. Bifocal segment types.
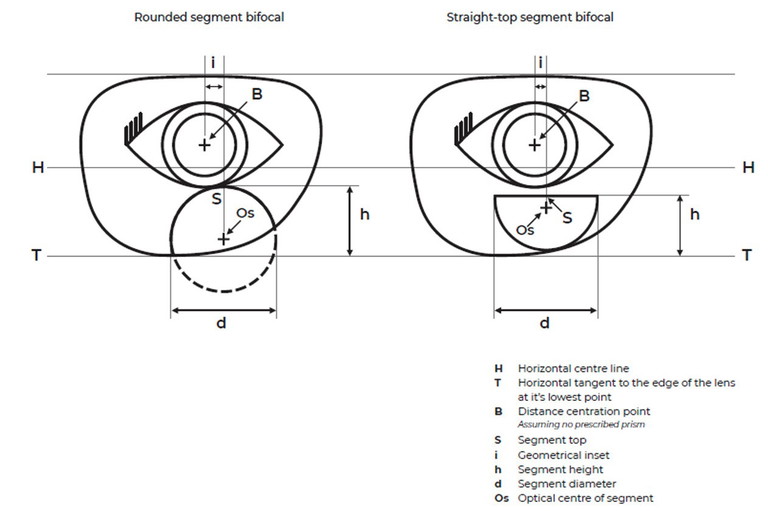
Figure 3. Bifocal fitting and measurements.
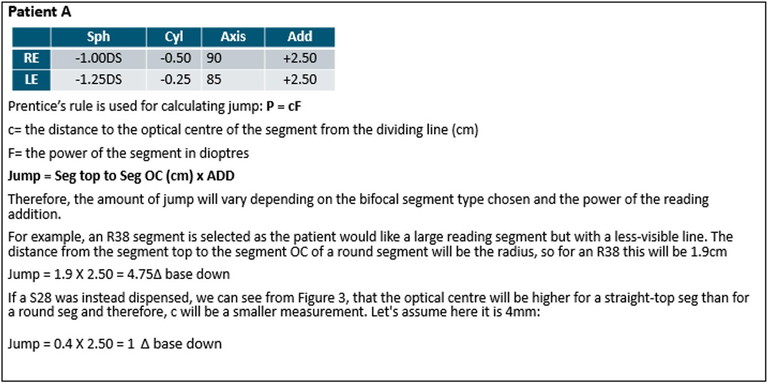
Figure 4. Jump calculation example.
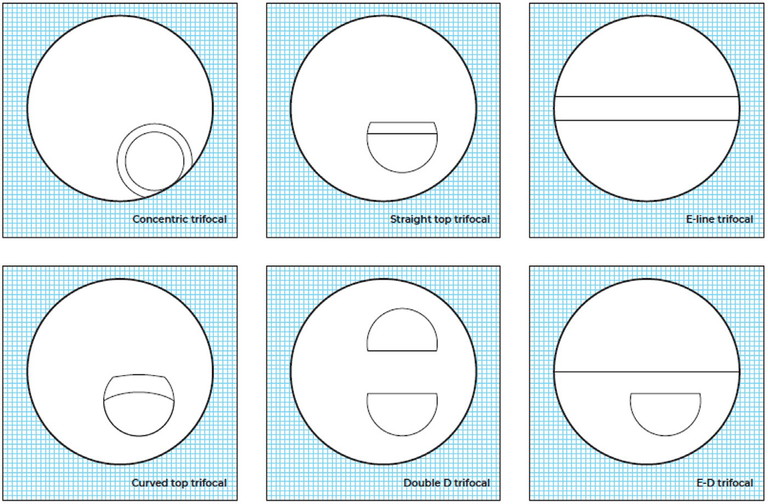
Figure 5. Trifocal segment types.
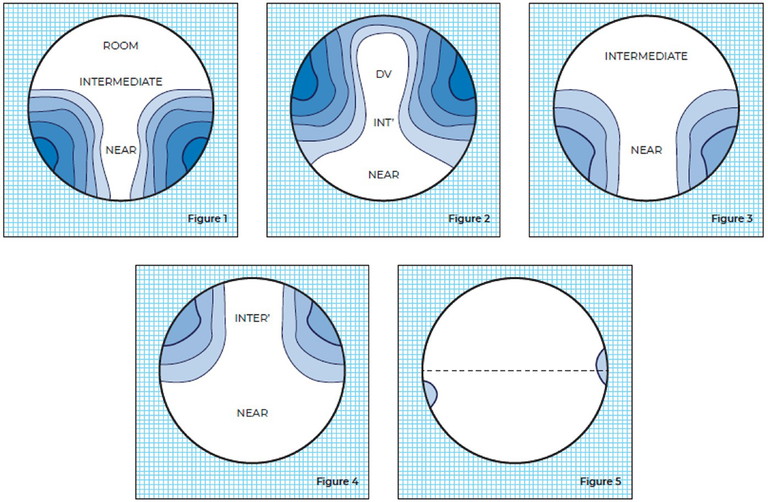
Figure 6. Examples of generic power variation lenses showing typical iso-astigmatism lines.
When ordering PALs, the chosen frame should be fully fitted before obtaining measurements. The lenses are ordered by specifying monocular pupillary distances and vertical heights of the pupil centres. Individualised designs require vertex distance, pantoscopic angle, and face-form angle. Lens manufacturers specify minimum fitting heights, which vary between designs. Independent research of improved wearer experience and patient preferences with modern PAL designs is still to be undertaken.
Occupational Progressive Lenses
An occupational lens can be considered to be any that has been selected to provide benefit for a specific situation or purpose. All occupational spectacle lens solutions will offer situational benefit, but equally require some compromise in reduced viewing distance or peripheral field of view. As touched on in previous sections, SV and multifocal lenses can be dispensed as occupation-specific spectacles. However, here we shall consider lenses that have a seamless progressive surface.
Returning to the Minkwitz rule, by reducing the power range across the progressive surface of the lens, we will also reduce the peripheral astigmatism. Therefore, a progressive occupational lens designed to correct for a reduced depth of focus will provide a wider field of view for the wearer. Figure 6 provides some examples of powervariation lenses that show how surface astigmatism is dependent on design.
Conceived for the office environment, occupational progressive lenses can be a solution for many other work, hobby, or lifestyle situations. Following a visual task analysis, a lens design can be selected that offers intermediate and near correction alongside a small distance-vision area for room-viewing at approximately 4 m. Other designs cater for those who have a closer visual demand, enabling viewing at 2 m or down to 1.2 m. Some designs specify a +0.50D addition to the distance correction and a -0.50 reduction from the near correction, providing a more middle-range focus progression. Most occupational progressive lenses are ordered in the same way as full progressive lenses, again being mindful of the manufacturer’s minimum fitting requirements.
Degressive Lenses
Compared to PALs, where two focal reference points are found (distance and near), a degressive lens only has a near reference point, with a reduction or ‘degression’ in power from near to intermediate. Therefore, degressive lenses are ordered using the near prescription, and a specified negative degression is applied, dependent on the design. Vertical centration may vary, depending on manufacturer requirements and intended use. Monocular vertical heights, that also take into account minimum fitting of usually 10 mm to the upper rim, are recommended.
As the power change across a degressive lens is less than in progressives, the result is a comparatively wider field of view. This lens type provides a focal range that can be selected to favour near or intermediate rather than distance viewing, along with a wider peripheral field than a full or occupational PAL, making it particularly suitable for patients with specific, extended close range needs.
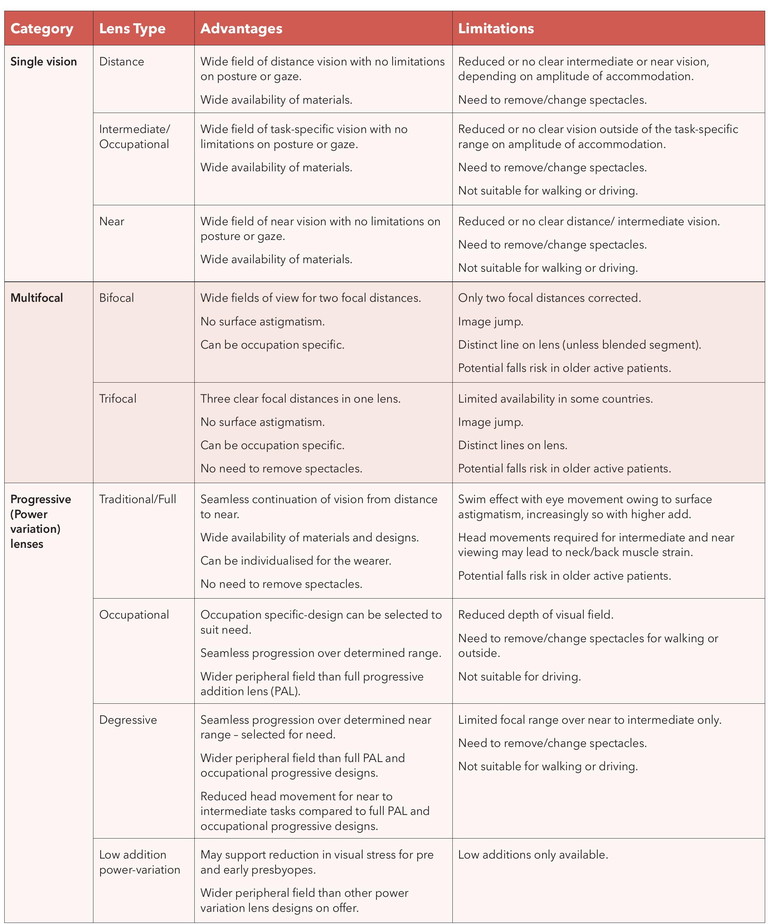
Table 1. Overview of advantages and limitations of presbyopic spectacle lens options.
Low-Add Power Variation Lenses
Often referred to as ‘boost’ or ‘anti-fatigue’ lenses in the UK, these designs employ a power-variation surface with a low addition ranging from 0.30D to 1.25D. Initially marketed to reduce visual fatigue caused by extended periods of accommodation while using digital devices, the lenses can be a visual solution for some pre and early presbyopes, with the low vertical power variation causing minimal subjective peripheral blur. Again, specifying monocular vertical fitting height is advised and the manufacturer-recommended minimum frame depth needs to be adhered to.
VISUAL TASK ANALYSIS WHEN DISPENSING
Given the impressive range of lens designs available, it may be difficult to know where to start when it comes to making spectacle recommendations for those with presbyopia.
Throughout the BCLA paper, there is reference to visual task analysis and its importance in selecting suitable solutions for the individual patient. However, there is limited research into visual task analysis available, and how to best match this to the patient’s individual requirements. The prevalence of digital eye strain is reported to be up to 90%, so the modern, digital working (and home) environment must be explored.
Suggested aspects of a visual task analysis for the presbyope include investigation of:
• Habitual gaze direction,
• Head tilt,
• Eye/head movements,
• Arrangement of the workstation (office and/ or home),
• Seating position,
• Luminance (including sources of glare),
• Use of different technologies (including tablets, laptops, smartphones),
• Duration of task, and
• Size of task.
When comparing presbyopic spectacle management options (Table 1), it is interesting to note that quality of vision scores for presbyopes has been found to be similar across SV distance, bifocal, or progressive correction wear.5 Studies have shown that following adaption, correctly fitted PALs are the preferred choice over other spectacle options and there is a subjective preference for modern free-form and individualised PALs, when compared to older designs. Suboptimal or lack of correction can significantly impact quality of life, vision, and task ability.9
CONCLUSION
The range of spectacle solutions for presbyopia is extensive, from single vision lenses to advanced progressive designs. To ensure successful spectacle dispensing for presbyopic patients (Figure 6), it is essential to thoroughly understand individual needs and conduct an accurate visual task analysis. With effective communication and by demonstrating the visual range that each lens option offers, we can help patients make wellinformed decisions about their eyewear.
Given the complexities of modern life, patients may benefit from choosing between various eyewear solutions, including both spectacles and contact lenses, depending on the tasks they face. However, there is a paucity of information available on the best practices for spectacle use and evidence-based management of presbyopia.
Top Tips for Practice
1. Maintain comprehensive knowledge of the features and benefits of lens products.
2. Conduct a full visual task analysis to understand the patient’s specific requirements.
3. Use clinical findings and patient information to guide spectacle lens recommendations.
4. Use demonstration tools to effectively communicate the trade-offs of each lens option.
5. Take accurate dispensing measurements and follow the manufacturer’s guidelines for dispensing.
Acknowledgement and recognition to the authors of the original paper: Philip Morgan, Nathan Efron, Eric Papas, Melissa Barnett, Nicole Carnt, Debarun Dutta, Andy Hepworth, Julie-Anne Little, Manbir Nagra, Heiko Pult, Helmer Schweizer, Bridgitte Shen Lee, Lakshman Subbaraman, Anna Sulley, Alicia Thompson, Alexandra Webster, MariaMarkoulli.
The paper is open access and available at BCLA CLEAR Presbyopia: Evaluation and diagnosis -Contact Lens and Anterior Eye (contactlensjournal. com) or via the QR code.
BCLA CLEAR Presbyopia was facilitated by the BCLA, with financial support by way of educational grants for collaboration, publication and dissemination provided by Alcon, Bausch and Lomb, CooperVision, EssilorLuxottica, and Johnson and Johnson Vision.

The editors for this article series are Neil Retallic and Dr Debarun Dutta.
To earn your CPD hours from this article, visit mieducation.com/bcla-clear-presbyopiamanagement-with-spectacles.

Alexandra Webster MSc PGDip FBDO CL FHEA FBCLA is a qualified dispensing optician and contact lens optician who has worked in both independent and corporate practices. She is Head of Continued Professional Development and a practical examiner in ophthalmic dispensing and contact lenses for the Association of British Dispensing Opticians (ABDO). Ms Webster has worked as a lecturer in ophthalmic dispensing and contact lenses at Bradford College and is an experienced author, presenter, and facilitator of CPD. She is currently undertaking a Professional Doctorate in Education with the Open University.
References
1. Morgan PB, Efron N, Dutta D, et al. BCLA CLEAR Presbyopia: Management with contact lenses and spectacles. Cont Lens Anterior Eye. 2024;47(4):102158. doi: 10.1016/j.clae.2024.102158.
2. Fricke TR, Tahhan N, Ho SM, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: Systematic review, meta-analysis, and modelling. Ophthalmology 2018;125(10):1492-9. doi: 10.1016/j.ophtha.2018.04.013.
3. Wolffsohn JS, Naroo SA, Markoulli M, et al. BCLA CLEAR presbyopia: Definitions. Cont Lens Anterior Eye. 2024;47(4):102155. doi: 10.1016/j.clae.2024.102155.
4. Wolffsohn JS, Berkow D, Haddad M, et al. BCLA CLEAR Presbyopia: Evaluation and diagnosis. Cont Lens Anterior Eye. 2024;47(4):102156. doi: 10.1016/j.clae.2024.102156.
5. Sivardeen A, McAlinden C, Wolffsohn JS. Presbyopic correction use and its impact on quality of vision symptoms. J Optom 2020;13(1):29-34. doi: 10.1016/j. optom.2018.12.004.
6. Elliott DB, Green A. Many ready-made reading spectacles fail the required standards. Optom Vis Sci. 2012;89(4):E446-51. doi: 10.1097/ OPX.0b013e318249d608.
7. Elliott DB. The Glenn A. Fry award lecture 2013: blurred vision, spectacle correction, and falls in older adults. Optom Vis Sci. 2014;91(6):593-601. doi: 10.1097/ opx.0000000000000268.
8. Sheedy JE, Campbell C, King-Smith E, Hayes JR. Progressive powered lenses: the Minkwitz theorem. Optom Vis Sci. 2005;82(10):916-22. doi: 10.1097/01. opx.0000181266.60785.c9.
9. Markoulli M, Fricke TR, Arvind A, et al. BCLA CLEAR presbyopia: Epidemiology and impact. Cont Lens Anterior Eye. 2024:102157. doi: 10.1016/j.clae.2024.102157.