mieducation
Individualised Solutions
Surgical Management of Presbyopia
The surgical management of presbyopia has become a hot topic and now, more so than ever, there are a number of different options that corneal and refractive specialists can add to their armamentarium to manage these patients. Optometrists are often the first point of contact for patients experiencing the effects of presbyopia. As such, understanding the various surgical treatment options available is crucial for providing informed recommendations and improving patient outcomes. In this article, Dr Erica Darian-Smith explores the most popular surgical interventions for laser refractive surgery, including monovision, Presbyond (ZEISS) optimising internal spherical aberrations, PresbyMax (Schwind Amaris) multifocal rings applied to the cornea, refractive lens exchange (RLE), and corneal inlays.
WRITER Dr Erica Darian-Smith
LEARNING OBJECTIVES
On completion of this CPD activity, participants should:
1. Be aware of the surgical options
for the correction of presbyopia,
2. Understand the benefits and drawbacks of each option,
3. Recognise the importance of customising the solution to the individual patient’s needs, and
4. Be aware of the important
role optometrists play in guiding
patient choice.
Presbyopia, or the loss of near vision is a real hassle, but an inevitable part of the ageing process, affecting almost every person over 40. It results from the gradual stiffening of the crystalline lens, which impairs its ability to change shape for near vision. Patients may struggle with multiple pairs of glasses or multifocal contacts, often complaining of compromise to their depth perception, contrast sensitivity, and overall quality of life.
Treating presbyopia is challenging as we are trying to attain perfection. The ideal procedure will be safe and deliver clear vision at distance, intermediate and near; good optical quality, with high contrast sensitivity and night vision preservation; binocularity; high patient tolerance; short adaptation time; simultaneous correction of refractive error; and, ideally, the ultimate panacea: reversibility.
Laser refractive surgery has long been an established option for correcting myopia, hyperopia, and astigmatism. In recent years, various laser techniques have been adapted to treat presbyopia. These procedures modify the cornea to change its shape and improve near vision.
MONOVISION
Monovision involves correcting the dominant eye for distance vision and the other nondominant eye for near vision. This allows patients to use their eyes for both near and distance vision without relying on glasses or contact lenses. While being a viable option, there are challenges with the inherent anisometropia that is created. These include: intermediate vision loss, reduced tolerance, reduction in distance vision, summation loss, and perhaps most importantly, stereoacuity loss. For some patients, monovision is an excellent option, particularly those who have natural monovision, or who have adapted with contact lenses or glasses.
LASER BLENDED VISION
Given that I offer Presbyond at my practice, I will focus on this procedure for the laser component of this discussion. This is a laser-assisted in situ keratomileusis (LASIK), flap-based procedure on the ZEISS refractive laser suite platform. I use the Visumax 800 femtosecond laser and the Mel90 excimer laser, which are the newest lasers in the ZEISS refractive suite. This procedure was devised by Professor Dan Reinstein, an eminent refractive surgeon based in London, United Kingdom. He states that laser blended vision is tolerated by almost all patients (97%) compared with traditional monovision techniques, which are tolerated by a lower proportion of 59–67% of patients.1,2 At our laser refractive clinic in Sydney, we strictly follow Prof Reinstein’s protocols.
Therefore, our patient selection for the procedure is thorough.
Standard criteria for LASIK:
• Normal tomography (no signs of forme fruste keratoconus),
• Stable refraction (reproducibility for a minimum of a year),
• Dry eye assessment (appropriate tear film and optimisation and treatment of dry eye before any laser intervention),
• No systemic comorbidities (mental health issues, autoimmune diseases, uncontrolled diabetes etc), and
• A healthy eye. Individual criteria for Presbyond:
• A clear lens, and
• They pass a cross-blur test (tolerate microanisometropia).
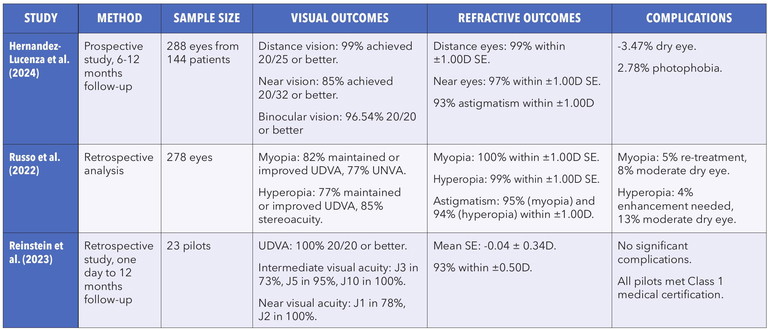
Table 1. Summary of main studies that have published results for laser blended vision.
The premise of laser blended vision is that an extended depth of focus and combined mini-anisometropia are used. To achieve this, the non-dominant eye is given a near aim (ranging from -1.5D to -0.75D, depending on the pre-existing accommodative amplitude and patient tolerance, which is measured in our preoperative cross-blur test), and the dominant eye is set for emmetropia. Blend zones exist between the two eyes (this is where the extended depth of focus effect is incorporated into the cornea). To achieve these ‘blend zones’ we use an individual measurement of the patient’s total spherical aberrations (internal and corneal), making this a highly personalised and customisable treatment. Ultimately, Presbyond laser blended vision is able to correct naturallyoccurring spherical aberrations of the eye, increasing depth of focus and combining this with a micro-anisometropia to generate near, intermediate, and distance correction across the two eyes. Like traditional LASIK, pupil size can be adjusted for by altering the optical zone of the treatment.
Presbyond research recently included the study of a group of commercial and military pilots requiring aeromedical certification who underwent the treatment, published in the Journal of Refractive Surgery in 2023.3 Pilots are a unique professional group for whom excellent vision is critical. Binocular distance and near vision are both important for their work. All pilots treated with Presbyond achieved 20/20 vision for distance at 12 months. Of these, 78% also achieved the near vision equivalent of 20/20 (J1). Of the pilots who did not achieve J1 vision, 100% had J2 vision. This is good enough to read size four font, the equivalent of small-print legal disclaimers on a bank statement.4 Table 1 summarises some of the main studies that have published results for laser blended vision.3,5,6
Benefits of Laser Blended Vision Quick surgery and recovery. Laser procedures typically have minimal downtime, and most patients experience significant improvement in their vision within a few days. Additionally, the procedure is performed in our inhouse refractive laser suite and is a bilateral, simultaneous 10-minute procedure.
“Treating presbyopia is challenging as we are trying to attain perfection”
High precision and patient satisfaction. The ability to customise laser treatment for each patient allows for highly individualised outcomes. Additionally, patients have shown to have high satisfaction rates post procedure.
Reduced dependence on glasses or contacts. Like RLE, laser surgery can reduce or eliminate the need for reading glasses or bifocals, offering a more permanent and convenient solution to presbyopia. Specifically for contact lens wearers, it also mitigates the risk of contact lens associated keratitis.
Large range of treatments. Spherical equivalent (SEQ) -8D to +2D with maximum 2D of cylinder (recommended) can perform laser SEQ -14D to +8D with a cylinder up to 6D (at the discretion of the surgeon). The generally accepted range is SEQ +5D to -9D. One of the advantages for emmetropic patients, is that only the non-dominant eye needs to undergo surgery to achieve optimal surgical results. This further limits expense and risk for my patients.
Adaptable when a cataract forms later in life. The non-linear presbyopic ablation profile and the induction of natural spherical aberrations of the cornea increase the depth of focus with lasting effects. This means that when a cataract develops later in life, individuals will retain the Presbyond ablation profile after treatment. Therefore, a simple monofocal lens can be implanted without losing the benefit of laser blended vision for reading.
Minimal glare and haloes. Presbyond patients do not usually complain about glare and haloes as can be experienced by some standard LASIK treatments. This is because spherical aberrations are optimised, improving rather than hindering night vision and overall optical clarity.
Reversible and adjustable. If enhancements are required, this is a quick, minimally invasive, and highly effective means of ‘reinvigorating’ near vision across the decades.
Drawbacks of Laser Blended Vision Monovision limitations. While monovision is effective for some patients, others may struggle with binocular vision, depth perception, or adaptation issues. Some patients may find it challenging to switch between distance and near vision without noticeable differences. However, we find this to be the minority of patients. This can be screened for early on in the assessment with appropriate adoption of the cross-blur test. Overall tolerance with the ‘micromonovision’ that Presbyond provides is, in our experience, much better than a traditional monovision approach.
Increased risk for dry eye. Laser procedures can exacerbate or trigger dry eye symptoms, especially in patients who are predisposed to this condition.
“All pilots treated with Presbyond achieved 20/20 vision for distance at 12 months”
Not suitable for everyone. Not all patients are candidates for laser surgery. Factors such as corneal thickness, age, and the presence of other eye conditions must be considered before proceeding with laser treatments.
Period of neuroadaptation. Presbyond has a period of neuroadaptation, which is usually six to 12 weeks. During this time patients may experience some instability of vision for either near or distance. With time this stabilises. If required, temporary glasses can be prescribed.
Enhancement rate. The reported enhancement rate of laser blended vision is 5–10% across the lifetime of the patient. This makes sense as a 40-year-old pre-presbyope who only tolerates 0.75 anisometropia will need to be enhanced later on when they are in their 50s and are experiencing the full effects of presbyopia. It is important that patients are aware of this from the outset.
CORNEAL INLAYS
Corneal inlays are small, disc-shaped devices that are implanted into the cornea to improve near vision. Typically placed in the nondominant eye, these inlays aim to provide a ‘reading boost’ to patients with presbyopia. The procedure is minimally invasive, performed in an outpatient setting, and generally has a quick recovery time. Several types of corneal inlays were available, including the Kamra inlay and the Raindrop inlay. These are no longer routinely used due to inadequate results and are now out-of-vogue.
A more modern variation of these now redundant prosthetic inlays is the Allotex corneal inlay. While in its infancy, preliminary results have been promising. The benefit of these allogenic corneal inlays is that they are highly biocompatible so are more likely to integrate well into the tissue and less likely to cause visually disturbing haze or scarring (one of the issues with the Kamra inlays). A simple, safe, and effective solution for emmetropic presbyopia and mild hyperopia, the inlay can be implanted under a LASIK flap at a depth of 100 μm or within a small incision lenticule extraction (SMILE) lenticule. Allotex corneal inlays can be useful in patients with previous refractive surgery, particularly LASIK, as the pre-existing flap can be opened up and the inlay inserted. There are, to date, very low reported rejection rates. One of the obvious drawbacks is that this inlay is only suitable for select cases and there is no longer-term follow-up data at this stage. (For more information on Allotex, turn to page 76.)
REFRACTIVE LENS EXCHANGE
Refractive lens exchange, also known as clear lens extraction, involves removing the eye’s natural lens and replacing it with an intraocular lens (IOL). While this procedure is traditionally performed to treat cataracts, it has also become a popular option for addressing presbyopia, particularly in patients over 45 who are no longer good candidates for traditional refractive surgery due to the natural ageing of their lenses, or where laser surgery is contraindicated.
RLE can be performed with different types of IOLs, including monofocal IOLs, multifocal IOLs, and accommodating IOLs. The goal of RLE in the presbyopic patient is to provide functional vision at various distances, reducing or eliminating the need for glasses.
With a wide range of lenses on the market, my refractive practice RLE patients have a number of options with respect to lens choice. Again, lens selection should be customisable to the individual based on aberrometry profile, previous history of refractive surgery, tolerance of monovision, corneal tomography appearance, personality, and occupation of the patient. For instance, in some situations, an aspheric lens may be preferable. Generally, my preferred lenses are the PureSee extended depth of focus (EDOF) lens (Johnson and Johnson) for which I find a mini-monovision setup of -0.5D works well. The trifocal lenses I have been using are the Panoptix Clareon platform (Alcon) and more recently, the Galaxy spiral lens (Rayner). I am a true believer that lenses should be selected at an individual level and also that new technologies should be tried, where appropriate, as each generation of lens – whether they be EDOF or trifocal – seem to be better than the last. Improvements in lens technology have both increased the range and quality of achievable vision and reduced side effects. The Galaxy lens has been designed with the purpose of minimising dysphotopsias (glare and haloes) that have traditionally been a problem with trifocal lenses.
Benefits of Refractive Lens Exchange Comprehensive vision correction. RLE can correct both presbyopia and refractive errors, such as myopia, hyperopia, and astigmatism. By replacing the natural lens with a multifocal IOL, patients can achieve a broader range of vision, including near, intermediate, and distance vision. Toric lenses very accurately correct residual astigmatism (assuming they adopt a regular pattern on tomography scans) and integrated K formulas can be used through the Barrett Universal calculator, which again increase accuracy as multiple device measurements are optimised.
No need for glasses or contacts. Depending on the choice of IOL, many patients experience significant improvement in their visual acuity and function without reliance on corrective eyewear.
Long-lasting results. The IOLs used in RLE procedures are designed to last a lifetime, providing a permanent solution for presbyopia.
Drawbacks of Refractive Lens Exchange Risk of retinal detachment. RLE, particularly when performed in younger presbyopic patients who have not yet had posterior vitreous detachment (PVD), carries an increased risk of retinal detachment. The removal of the natural lens can alter the dynamics of the vitreous body, increasing the likelihood of vitreoretinal traction and subsequently, retinal tears or detachment.
Intraoperative complications. As with any surgery, RLE carries the risk of complications, including retinal detachment, loss of endothelial cells, infection, aberrations, posterior capsular opacification, macular oedema, and suprachoroidal haemorrhage to name a few. Patients must be appropriately counselled that this is a more invasive approach than laser and corneal inlay options. Realistic expectations must be set from the beginning, and a comprehensive consent process must be undertaken. While the procedure is generally complication free, the potential for complications must be discussed with patients beforehand.
Not all patients adapt to multifocal or accommodating IOLs with equal ease. Some may experience haloes, glare, or difficulty with contrast sensitivity, especially in lowlight conditions. Patients must allow adequate time for neuroadaptation. It can be useful to trial an in office dysphotopsia (glare and halo) simulator to try to simulate potential postoperative conditions for the patient.
“RLE, particularly when performed in younger presbyopic patients who have not yet had posterior vitreous detachment (PVD), carries an increased risk of retinal detachment”
Retinal Detachment Risk and PVD
As described above, one critical concern with lens-based surgeries, such as RLE, is the increased risk of retinal detachment (RD), particularly for younger patients who have not experienced posterior vitreous detachment (PVD). PVD is a natural process in which the vitreous gel separates from the retina, and while it occurs in many individuals after age 50, it can leave the retina more vulnerable to traction and detachment.
For patients undergoing refractive lens exchange, especially those without PVD, it is important to emphasise the potential risk of retinal detachment. The removal of the natural lens may disturb the vitreous body, which can lead to increased vitreoretinal traction. In these cases, retinal tears or detachment can occur, which may necessitate surgical intervention.
It has been reported that there is a 12-fold increased risk of pseudophakic retinal detachment in myopes aged 60 and under undergoing lens-based surgery. Axial length and age are both markers of risk:7
• If the axial length is >25 mm (myopic eyes) there is a six-times increased risk of RD,
• In younger eyes < 60 years of age there is a six-times increased risk of RD,
• So younger age and increased axial length increase the risk of RD in myopes.
• The risk is lower for hyperopes and emmetropes.
A more recent study determined that the incidence of RD after RLE was double that observed after cataract surgery with a minimum of 24 months and a median of four years follow up. RD is classified as rare post-standard cataract surgery (0.001%) and an uncommon complication after RLE surgery (0.002%).8
“While the perfect solution for presbyopia still does not exist, every year we are getting closer to finding the ultimate solution for this troublesome condition”
Another tool I find useful to help quantify risk for my patients was designed by a Danish research team. The ‘For Your Eyes Only’ (FYEO) medical RRD risk calculator can be accessed via the below link and uses the patient’s age, axial length, presence or absence of lattice degeneration, and the presence or absence of a PVD to stratify the overall risk of RD following RLE. Visit: medisch.fyeo.nl/retinal-detachment/retinal-detachment-calculator.
In contrast, laser-based presbyopia correcting procedures do not involve the removal of the lens, and thus they do not carry the same risk of retinal detachment associated with RLE. While any refractive surgery carries some inherent risks, the likelihood of retinal complications is generally lower with corneal-based procedures than with lens exchange surgeries.
CONCLUSION
Surgical management of presbyopia offers a wide range of options for patients seeking to reduce their dependence on reading glasses or bifocals. Refractive lens exchange, corneal inlays, and laser refractive surgeries such as monovision, Presbyond, and PresbyMax each offer unique advantages and limitations. Optometrists play a crucial role in assessing patients’ suitability for these procedures and providing detailed information on the benefits and potential risks, including the possibility of retinal detachment for patients undergoing lens surgery.
Ultimately it is the responsibility of the refractive surgeon to choose the most appropriate surgical treatment based on individual patient’s needs, criteria, and anatomy. There is no one-size-fits-all approach and that is why the work-up for the surgical correction of presbyopia is time consuming, challenging, and requires forward thinking and effective planning.
Patients and surgeons must work together to find a solution; realistic expectations must be set from the beginning; and importantly, comprehensive diagnostic testing must be performed to ensure safety and reproducibility of results. While the perfect solution for presbyopia still does not exist, every year we are getting closer to finding the ultimate solution for this troublesome condition – whether that be in the form of laser, corneal inlays, or lens-based procedures.
To earn your CPD hours from this article, visit mieducation.com/individualised-solutions-surgicalmanagement-of-presbyopia.
References
1. Reinstein DZ, Archer TJ, Gobbe M. LASIK for myopic astigmatism and presbyopia using non-linear aspheric micro-monovision with the Carl Zeiss Meditec MEL 80 platform. J Refract Surg. 2011 Jan;27(1):23-37. doi: 10.3928/1081597X-20100212-04.
2. Evans BJW. Monovision: a review. Ophthalmic and Physiological Optics. 2007 Sep;27(5):417–39. doi:10.1111/j.1475-1313.2007.00488.x
3. Reinstein DZ, Ivory E, Parbhoo M, et al. Presbyond laser blended vision LASIK in commercial and military pilots requiring class 1 medical certification. J Refract Surg. 2023 Jan;39(1):6-14. doi: 10.3928/1081597X-20221129-02.
4. McDonald MB, Barnett M, Trattler WB. Classification of presbyopia by severity. Ophthalmol Ther. 2022 Feb;11(1):111. doi: 10.1007/s40123-021-00410-w.
5. Hernández-Lucena J, Alonso-Aliste F, Amián-Cordero J, Sánchez-González JM. Outcomes of corneal compound myopic astigmatism with presbyopia by Zeiss Presbyond laser blended vision lasik using default crs-master target refractions for reduced anisometropia. J Clin Med. 2024 May 20;13(10):3011. doi: 10.3390/jcm13103011.
6. Russo A, Reinstein D, Semeraro F, et al. Visual and refractive outcomes following laser blended vision with non-linear aspheric micro-anisometropia (PRESBYOND) in myopic and hyperopic patients. J Refract Surg. 2022. 38(5):288-297. doi: 10.3928/1081597X-20220323-01. Erratum in: J Refract Surg. 2022 Jul;38(7):474. doi: 10.3928/1081597X-20220630-01.
7. Srinivasan S. Pseudophakic retinal detachment: a ticking time bomb. J Cataract Refract Surg. 2023 Mar 1;49(3):225226. doi: 10.1097/j.jcrs.0000000000001157.
8. Chan E, Varma S. Refractive lens exchange - the evidence behind the practise. Eye (Lond). 2025 Feb;39(2):208-209. doi: 10.1038/s41433-024-03478-3.

Dr Erica Darian-Smith MBBS MMed GradDipRefCatSurg FRANZCO is an ophthalmologist who specialises in refractive, cataract, and corneal surgery. Dr Darian-Smith completed her training in ophthalmology at Prince of Wales hospital in Sydney. Afterwards, she undertook an intensive, world renowned, two-year fellowship in corneal, refractive surgery and external eye diseases in Toronto, Canada where she gained subspecialty expertise in laser eye surgery and treatment of all corneal diseases, including corneal transplants.
Dr Darian-Smith is a director and cofounder of Eagle Eye Surgeons, a state of the art refractive and comprehensive ophthalmology clinic with locations in Mosman and Nepean in Sydney, Australia. She is a Clinical Lecturer at Save Sight Institute, the University of Sydney, and a Visiting Medical Officer (VMO) at Nepean Public Hospital.