mieducation
Supporting Sight: The Evidence for Nutraceutical Supplements
Glaucoma is a leading cause of irreversible blindness and affects over 200,000 Australians over the age of 50, with an increasing prevalence. 1 Intraocular pressure (IOP) is considered the most important modifiable risk factor in glaucoma, and this underpins the principles of glaucoma management in the clinical setting. However, glaucoma can still progress despite well-controlled IOP, suggesting that other non-pressure dependent mechanisms exist.
There is a significant body of research looking at these often interconnected non-pressure dependent factors, and how they can be effectively targeted to provide neuroprotection for those with – or at risk of – glaucoma.
By linking specific nutrients to the non-pressure dependent factors and biocellular risks underlying the mechanisms of glaucoma, Drs Brian Ang and Varun Chandra highlight the scientific basis underpinning the potential roles of supplements in the prevention and management of glaucoma.
WRITERS Dr Brian Ang and Dr Varun Chandra
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Understand the pathophysiology and risk factors underpinning glaucoma progression,
2. Identify key nutraceutical supplements and their potential role in addressing risk factors for glaucoma progression, and
3. Be equipped to have informed discussions with patients regarding nutraceutical supplementation for glaucoma management.
MANAGING INTRAOCULAR PRESSURE
Bilberry-Maritime Pine Bark IOP is currently the only proven modifiable risk factor in glaucoma. The most accepted mechanism of glaucoma is elevated IOP increasing the pressure gradient across the lamina cribrosa and compressing retinal ganglion cells (RGCs), leading to neuronal damage and eventual cell death.2
In 2008, Steigerwalt and colleagues published the first paper on the IOP-lowering effect of a combination of bilberry combined with maritime pine bark. In this study, they found that the bilberry-French maritime pine bark supplement was able to reduce IOP from 25.2 (±3.1) mmHg to 22.0 (±2.6) mmHg after three months in asymptomatic ocular hypertensive (OHT) patients, while there was no change in IOP in the control group.3
In a subsequent trial, the same group randomly assigned 79 asymptomatic ocular hypertension (OHT) patients to receive either the bilberry-maritime pine bark supplement, latanoprost eye drops, or both in combination. After 24 weeks, the IOP reduction achieved with a combination treatment of bilberrymaritime pine bark supplement and latanoprost (39.5%; from baseline 38.0 mmHg to 23.0 mmHg) was significantly greater than latanoprost alone (27.9%; from baseline 37.7 mmHg to 27.2 mmHg).4
The bilberry-maritime pine bark combination has also been evaluated in primary openangle glaucoma (POAG) patients. In their pilot study, Manabe and colleagues found that in POAG patients taking one to three types of antiglaucoma medications, mean IOP decreased significantly from 17.2 (±2.3) mmHg to 15.7 (±1.9) mmHg after four weeks of supplementation with bilberry-maritime pine bark tablets.5
The efficacy of the bilberry-maritime pine bark combination is likely due to its respective active ingredients: anthocyanins in bilberry, and proanthocyanidins in maritime pine bark. Bilberry is one of the richest natural sources of anthocyanins, containing significantly higher amounts of anthocyanins compared with other berries. Maritime pine bark, together with grape seed, is one of the best natural sources of proanthocyanidins.
While both anthocyanins and proanthocyanidins are powerful flavonoid antioxidants, it is not entirely clear how they combine to reduce IOP. Possible mechanisms include increasing trabecular meshwork outflow through antioxidant activity at the trabecular meshwork or reducing aqueous production through enhanced microcirculation and capillary resistance at the ciliary body. Additionally, proanthocyanidins from maritime pine bark and grape seed are also known to improve endothelial function and reduce systolic and diastolic blood pressure, which in turn may indirectly lead to decreased IOP.6-9
Saffron
Another natural plant extract that has been shown to reduce IOP is saffron. Saffron has been widely used for hundreds of years in Ayurvedic and Persian remedies for its traditional medicinal effects. Its bioactive compounds, the carotenoids crocin and crocetin, are not available in any other food sources. Saffron is now increasingly recognised and researched for its eye health benefits, particularly for macular degeneration and diabetic maculopathy.
A pilot study by Bonyadi et al. demonstrated an ocular hypotensive effect of oral saffron extract. In this small trial of stable POAG patients on timolol-dorzolamide eye drops, saffron significantly decreased the IOP from a mean of 12.9 (±3.7) mmHg to 10.6 (±3.3) mmHg after three weeks. At the end of the one-month washout period, the IOPs returned to their original levels. 10
One possible theory offered by the authors was that saffron counteracted the oxidative stress and extracellular matrix alterations at the trabecular meshwork, which caused increased IOP.10 Another possible theory is that saffron indirectly reduces IOP by improving psychological stress and consequently decreasing circulating stress hormone levels.
ADDRESSING VASCULAR DYSREGULATION
Impaired vascular perfusion of the optic nerve has been implicated in glaucoma for over a century, mainly from vascular dysregulation, with evidence accumulated in normal tension glaucoma (NTG) studies. 11 A large body of evidence exists demonstrating impairment of optic nerve blood flow in glaucoma patients, including recent studies using optical coherence tomography angiography (OCT-A).12
It has long been postulated that improving ocular blood flow to the optic nerve and surrounding peripapillary retina could slow visual field progression in glaucoma patients, particularly those in whom the IOP is already well-controlled or low. Most of the literature on the impact of nutraceuticals on ocular blood flow and glaucomatous visual field progression revolves around anthocyanins and ginkgo biloba.
Anthocyanins
The bilberry anthocyanin-maritime pine bark combination, in addition to its IOP-lowering effect, has been shown to increase ocular blood flow, particularly in the systolic and diastolic blood flow velocity of the central retinal artery, ophthalmic artery, and posterior ciliary artery.13-15 In a retrospective study of 132 Korean subjects with NTG, supplementation with bilberry anthocyanins resulted in a statistically significant improvement in mean deviation from -6.44 (±7.05) dB to -5.34 (±6.42) dB after two years.14
“ It is ginkgo biloba, however, that has received the most interest around ocular blood flow and peripapillary microcirculation ”
Blackcurrant-derived anthocyanins have also demonstrated increased ocular blood flow haemodynamics and slowing of visual field progression in open-angle glaucoma (OAG) in a randomised placebo-controlled study by Ohguro et al.16 The authors found that the treatment group had no significant decrease in mean deviation over the 24-month observation period, whereas a statistically significant decrease from 12 months to 24 months was noted in the placebo group.16 The same authors published a follow-up study reporting a normalisation of serum endothelin-1 levels in glaucoma patients taking anthocyanin, thus providing a hypothesis on how anthocyanins may modulate the regulation of ocular blood flow.17
Gingko Biloba
It is ginkgo biloba, however, that has received the most interest around ocular blood flow and peripapillary microcirculation. Ginkgo biloba extract (GBE) is derived from the leaves of the ginkgo tree, which contain over 60 bioactive compounds, including a high concentration of flavonoids and terpenoids. It has been used as a traditional medicinal plant for over 2,000 years in China and other parts of the world.
GBE addresses vascular dysregulation by reducing blood viscosity and inhibiting platelet aggregation through increasing concentrations of thrombolytics. Specific to the eye, improvements in ocular blood flow have been demonstrated in the retinal capillaries, peripapillary region, retrobulbar blood vessels, and ophthalmic artery. 18-20
In their long-term study of NTG patients with a mean follow-up of 12.3 years, Lee et al. showed that GBE administration slowed the progression of visual field damage in NTG patients from a visual field index (VFI) rate of -2.153 (±0.142)% per year to -1.212 (±0.166)% per year.21
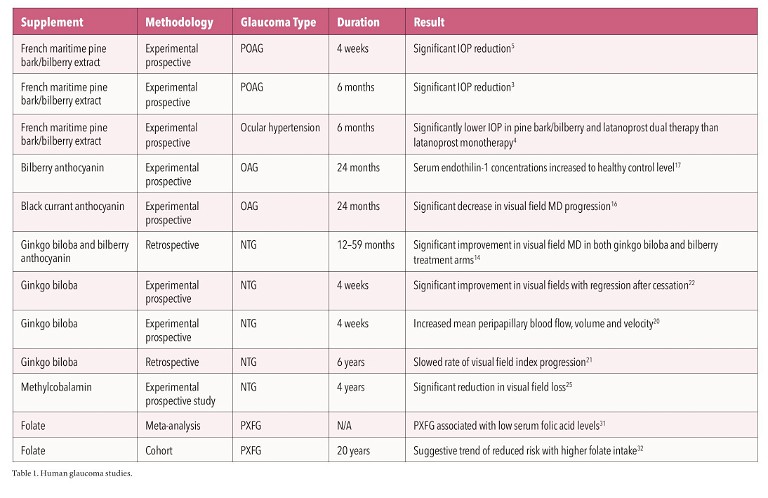
The strongest evidence supporting GBE use in glaucoma is from a randomised crossover trial of NTG patients by Quaranta and colleagues. The study analysed the effect of GBE 40 mg three times daily on visual fields. After four weeks of treatment, a significant improvement in visual field indices, including mean deviation and pattern standard deviation, was reported. A regression in visual field indices did occur after treatment cessation, suggesting a limited duration of action of GBE.22
SUPPORTING NEURONAL FUNCTION
RGC axons are a key component in glaucoma and are responsible for mitochondrial transport within individual cells. Elevated IOP interrupts axonal mitochondrial transport in animal models. RGC axons are particularly susceptible to kinking and stress as they pass through the lamina cribrosa, rendering them vulnerable to compression in glaucoma. Moreover, intraocular RGC axons are unmyelinated for optical purposes and unmyelinated axons require four-fold more energy, placing a higher burden on axons within the intraocular portion of the optic nerve.11
Vitamin B12 is important for phosphatidylcholine synthesis, which in turn is essential for the preservation of the myelin sheath around neurons, maintenance of nerve cell membrane stability, and synthesis of neurotransmitters – all vital for nerve function. Methylcobalamin is the most bioavailable form of vitamin B12, and its efficacy in improving neuronal function and treating peripheral neuropathy has previously been reported.23,24
Given that glaucoma is a neuropathy, there has been interest in supporting and promoting neuronal function with methylcobalamin to improve visual outcomes in glaucoma patients. Yamazaki and colleagues had previously reported that NTG patients treated with methylcobalamin showed significant improvements in retinal sensitivity compared to the untreated group.25 A subsequent followup prospective trial by the same group suggested a slower progression of visual field loss in NTG patients supplementing with methylcobalamin over the long term. The authors found that over four years, progression of visual field defects occurred in only 14% of NTG patients taking oral methylcobalamin, compared with 59% in the control group.25
Methylcobalamin supplementation is of particular relevance to vegetarian patients, as unlike other vitamins, the major source of vitamin B12 in our diets is from animal-derived products.26 It is also relevant for older patients because vitamin B12 deficiency increases with age due to the progressive inability to effectively absorb vitamin B12 from food.27
LOWERING HOMOCYSTEINE LEVELS
Elevated levels of serum homocysteine, a non-proteinogenic amino acid, have been associated with neurodegenerative conditions including glaucoma, and may present a risk factor for the development and progression of glaucoma. Numerous studies have reported higher serum homocysteine levels in not just pseudoexfoliation glaucoma, but also in POAG and NTG.28,29 In addition, retinal nerve fibre layer defects have also been associated with elevated homocysteine levels.30
The methyl group in methylcobalamin is used not only for phosphatidylcholine synthesis, but also for the synthesis of methionine from homocysteine; methylcobalamin deficiency therefore contributes to elevated homocysteine levels. The ability to metabolise and reduce homocysteine is considered another possible mechanism by which methylcobalamin confers neuroprotective effects in glaucoma.2
“ Elevated levels of serum homocysteine, a non-proteinogenic amino acid, have been associated with neurodegenerative conditions including glaucoma, and may present a risk factor for the development and progression of glaucoma ”
Like methylcobalamin, folate is also an important coenzyme involved in homocysteine metabolism. Low serum folate levels are associated with elevated plasma homocysteine levels and pseudoexfoliation glaucoma, based on a 2012 meta-analysis. 31 In a national prospective cohort study of nearly 120,000 subjects, over more than 20 years of follow-up, those with higher folate intake were found to have lower rates of pseudoexfoliation glaucoma.32 Interestingly, the same study did not reveal any association between vitamins B6 and B12 with pseudoexfoliation glaucoma.
Folate absorption, similar to vitamin B12 absorption, decreases with age. However, from a bioavailability standpoint, the commonly commercially available folic acid is not the best option to supplement folate levels. This is because folic acid must first be converted into the biologically active form by reduction and methylation, and even then, it may not be effectively transported through the blood-brain barrier.32 L-methyl folate, on the other hand, already in its biologically active form, does not require further metabolisation, and is readily transported through the blood-brain barrier via the reduced folate carrier.33,34
MITIGATING MITOCHONDRIAL DYSFUNCTION
The role of mitochondrial dysfunction in glaucoma and RGC loss has garnered significant research interest. In mice models, a differential expression of genes encoding mitochondrial proteins has been reported. In human studies, mitochondrial DNA abnormalities have been detected in POAG patients, and mitochondrial DNA lineages may modulate the risk of developing POAG in European populations.11
A key cofactor for mitochondrial function and energy metabolism is nicotinamide adenine dinucleotide (NAD+). NAD+ levels naturally decline with age, resulting in reduced mitochondrial activity in RGCs and increased vulnerability to glaucoma damage.
Nicotinamide is the amide of vitamin B3 and a major natural precursor of NAD+. It is highly bioavailable to the eye and can rapidly increase NAD+ levels in the retina. This improves mitochondrial function in RGCs and reduces their susceptibility to damage during periods of elevated IOP.
The impact of nicotinamide supplementation in glaucoma was first reported in 2020. Hui and colleagues conducted a crossover randomised clinical trial that examined the effect of short-term, high dose oral nicotinamide supplementation on inner retinal function in glaucoma patients.
Participants received six weeks of 1.5 g daily, then six weeks of 3 g daily, then crossover to placebo or vice versa. The authors reported an improvement in inner retinal function in stable glaucoma patients with nicotinamide supplementation at a daily dose of 3 g.35
Two other commercially available NAD+ precursors are increasingly popular, namely nicotinamide riboside and nicotinamide mononucleotide (NMN). From the glaucoma perspective, nicotinamide is preferable over either of them because of its ability to increase NAD+ levels in the retina the most rapidly. In addition, NMN supplementation can trigger axon degeneration in susceptible eyes when NAD+ levels are low, and so should ideally be avoided in those at risk of glaucoma. 36
IMPROVING GLUCOSE METABOLISM
Elevated IOP dramatically alters energy metabolism in retinal ganglion cells (RGCs). It induces transcriptional changes in pyruvate metabolism, glycolysis pathway, fructose metabolism, and gluconeogenesis. 37 In mice models, Harder et al. detected a 50-fold elevation of retinal glucose levels linked to an IOP-dependent decline in pyruvate levels and dysregulated glucose metabolism. In these models, oral pyruvate supplementation strongly protected RGCs from neurodegeneration.38
A
B
C
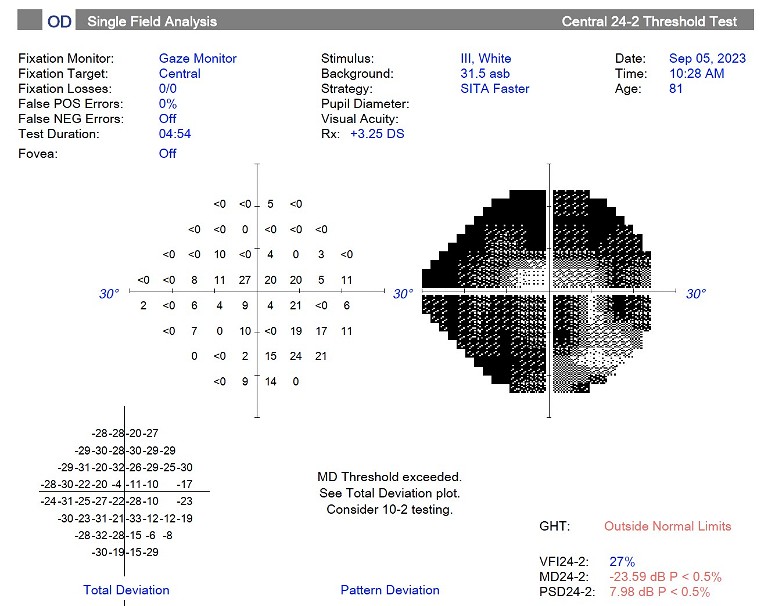
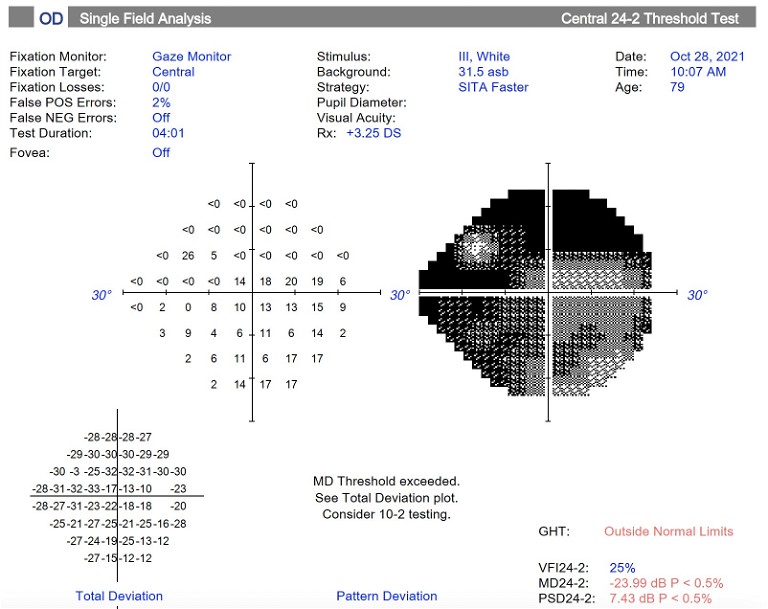
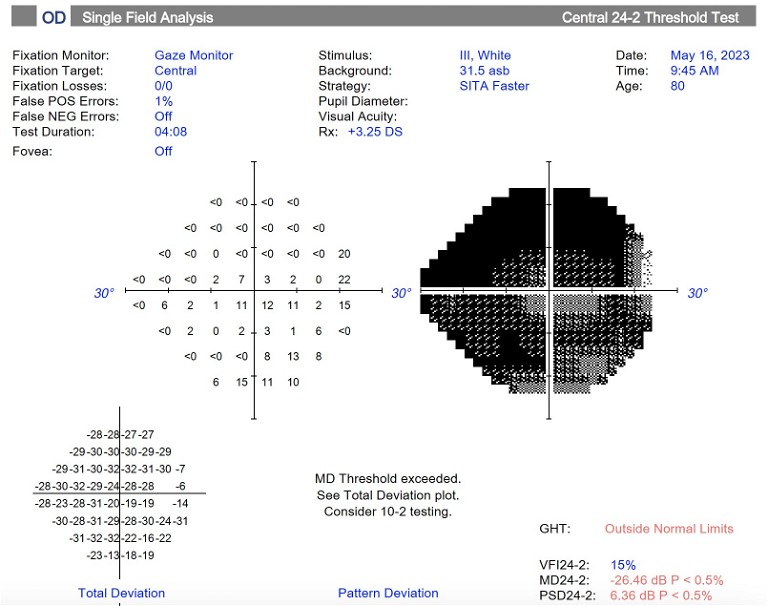
Figure 1. Humphrey visual field 24-2 of the right eye demonstrating A) advanced glaucomatous field loss in October 2021, B) progression of visual field loss in May 2023, and C) improvement in visual field after taking nutraceutical supplement capsule for 3.5 months.
Pyruvate is a key intermediate in many biological processes, including glucose metabolism and cellular metabolism. It is vital for RGC health due to its role in preserving cellular glycolytic pathways. By increasing pyruvate levels through supplementation and improving glucose metabolism, the optic nerve becomes less predisposed to degeneration when IOP is elevated.
Pyruvate was evaluated in a clinical trial of mild to moderate OAG patients who were supplemented with both pyruvate and nicotinamide in increasing doses. Over a median follow-up of 2.2 months, the authors reported a significantly higher number of improving visual field test locations and pattern standard deviation improvement, although there was no significant improvement in mean deviation (MD).39
While the results are promising , further research is required to determine the optimal long-term dose of pyruvate and nicotinamide for glaucoma neuroprotection.
COMBATING OXIDATIVE STRESS AND REDUCING NEUROINFLAMMATION
A large body of literature exists implicating oxidative stress in glaucoma as well as its role in glaucoma progression.28,40 RGCs are metabolically very active and the subsequent reactive oxygen species produced are theorised to contribute to RGC loss in glaucoma.28 Oxidative stress leads to increased inflammation, which in turn is implicated in glaucomatous disease progression. An increase in anti-inflammator y white cells has been detected in glaucomatous optic nerves, and systemic inflammator y markers have been demonstrated to be significantly increased in POAG patients.40
The natural plant extracts discussed above, such as ginkgo biloba leaf, bilberry, maritime pine bark , grape seed, and saffron all have strong antioxidant activity and contribute to a reduction in oxidative stress and inflammation. All have been investigated for their potential benefit on RGC health in animal models.
GBE contains phytochemical antioxidants that act at the mitochondrial level, unlike general antioxidants such as vitamin C. This helps with stabilising the inner mitochondrial membrane and assists with cellular energy production.41,42 In a rat model of NTG, GBE was shown to improve RGC survival.43
Grape seed proanthocyanidins have potent antioxidant activity that is 20 times greater than vitamin E and 50 times greater than vitamin C44 and has been shown in mouse models to protect RGCs by inhibiting oxidative stress and mitochondrial alteration.45 Crocetin from saffron has been shown to reduce inflammation and the proportion of apoptotic RGCs in glaucoma rats,46 while bilberr y administration was also able to suppress RGC death following optic nerve injury.47
ADDRESSING MACULAR PIGMENT DEFICIENCY
Macular pigment, comprising the essential carotenoids lutein and zeaxanthin, is highly concentrated at the fovea. It is an important component of central visual function and plays an important supportive role through retinal antioxidant protection, improved visual performance, and increased neural efficiency.
Additionally, lutein and zeaxanthin are absorbers of blue visible light (400–500 nm) and thus protect the eye structures from dangerous doses of this radiation. This is important because short-wavelength blue light is high energy and highly reactive, and can enhance light-induced oxidative degeneration at the fovea.48 As a result, lutein and zeaxanthin have been extensively studied for their protective benefits in macular degeneration, and to a lesser extent, diabetic maculopathy.
Macular pigment optical density (MPOD) has been demonstrated to be lower in subjects with OAG compared to controls.49 Subsequent research found lower MPOD to be correlated with the extent of loss of the foveal ganglion cell complex and central 10-degree field.50,51 As macular involvement with corresponding central field defects may be more common in glaucoma than previously realised, it makes sense to support central visual function by augmenting macular pigment levels. In their 18-month randomised clinical trial, Loughman et al. reported that supplemental use of lutein and zeaxanthin in glaucoma patients did not just significantly increase MPOD, it also significantly improved mesopic contrast sensitivity under glare conditions. The greatest benefit was observed in patients with low baseline levels of these carotenoids.52
The average intake of lutein in adults ranges from 1–2 mg per day. This is far below the recommended dietary intake level of 10 mg of lutein and 2 mg of zeaxanthin per day to reduce the risk of macular degeneration.53 Given the beneficial impact on central visual function, perhaps the recommended dietar y intake level for lutein and zeaxanthin should also be adopted for glaucoma patients to reduce the risk of central vision deficits.
WHICH NUTRIENT TO TAKE?
Now that we have discussed the non-pressure dependent risk factors that contribute to glaucoma and the nutrients that may clinically mitigate these risks, we need to ask: which nutrient supplements should we prioritise?
There is no right or wrong approach, but in our opinion, all these mechanisms and risks need to be addressed if we want comprehensive glaucoma neuroprotection. Currently, no test can accurately identify the exact mechanisms of glaucoma progression for a particular individual. Even if such a test existed, it is possible that these mechanisms could change over time for that individual.
CASE STUDY
An 81-year-old man with advanced glaucoma in both eyes had previously undergone bilateral trabeculectomy, cataract surgery with iStent inject implantation, and selective laser trabeculoplasty multiple times. On maximal medical therapy, his IOP was well-controlled at ≤13 mmHg in both eyes.
Over a 19-month period from October 2021 to May 2023, the left eye remained stable, but the right eye showed perimetric progression (Figure 1A and 1B). The MD in his right field worsened from -23.99 dB to -26.46 dB and VFI decreased from 25% to 15%, despite IOP consistently measuring 12 mmHg.
At this point, the discussion was on whether to undergo yet another operation or to try a commercially available nutraceutical supplement capsule containing the nutrients discussed in this article (bilberry, ginkgo biloba, grape seed, L-methyl folate, lutein and zeaxanthin, methylcobalamin, nicotinamide, pyruvate, and saffron). The patient opted for the latter option. No changes were made to his existing medications.
On review 3.5 months later, IOP remained at 12 mmHg, and not only had his right visual field stabilised, it had even shown an improvement ( Figure 1C). The MD improved to -23.59 dB and the VFI increased to 27%. He reported no adverse effects from taking the supplement.
The patient remains under close monitoring. Data collection is ongoing for him as well as for other glaucoma patients who are also taking the aforementioned nutraceutical supplement capsule.
CONCLUSION
In the realm of glaucoma management, the role of nutritional supplementation holds great promise.
There is currently no higher-level evidence in the form of a well-designed randomised clinical trial proving that taking all these nutraceutical supplements altogether will prevent or slow the progression of glaucoma. However, there is a plethora of evidence demonstrating the safety profile of these supplements individually and their potential benefits, not just in glaucoma but systemically. Based on our clinical obser vations and appraisal of existing scientific data, we opine that there already exists enough evidence to open a discussion with patients about the roles of specific nutrients and nutraceuticals for glaucoma neuroprotection.
Acting in the best interests of our patients should be at the core of our clinical practice.
We believe this includes doing our best to educate our patients on options for neuroprotection based on the current evidence that is already available.
To earn your CPD hours from this article, visit: mieducation.com/supporting-sight-the-evidence-fornutraceutical-supplements-in-glaucoma.
References available at mivision.com.au

Dr Brian Ang FRANZCO FRCOphth FRCSEd(Ophth) is a Melbourne-based glaucoma specialist, clinical researcher, and co-founder of Nutravision (nutravision.com.au). He has over 70 peer reviewed publications, with research interests in novel surgical treatments and neuroprotection for glaucoma. Dr Ang is a keen advocate of ‘proactive glaucoma’ – the proactive management of risk for glaucoma and glaucoma suspect patients.

Dr Varun Chandra MBBS (Hons) is an Ophthalmology Fellow based at the Sunshine Coast University Hospital. Prior to completing ophthalmology training in Victoria, Dr Chandra completed his medical degree at the University of New South Wales. He was the recipient of the Adam Locket Memorial Award for Ophthalmic Anatomy from the University of Sydney in 2015.