mievent
World Congress of Optometry

at O=MEGA23
L-R: Professors Jennifer Craig, James Wolffsohn, and Lyndon Jones.
With numerous simultaneous streams covering a full spectrum of topics, we were spoilt for choice when the 4th World Congress of Optometry (WCO) partnered with O=MEGA23 in Melbourne. Alan Saks was among the 1,257 Congress delegates (including 200 from overseas) and 3,585 event attendees.
WRITER Alan Saks
The diverse, three-day WCO/O=MEGA23 event – held at the Melbourne Convention and Exhibition Centre in September – was chock full, with 88 presentations and 33 international presenters. Alongside the main conference streams there were also a number of excellent workshops and a strong dispensing program.
Mandy Nicholson and the Djirri Djirri dancers delivered a positive welcoming message and dance, setting the congress off to a great start.
The opening plenary talk, delivered by Associate Professor Peter Hendicott, of Queensland University of Technology, covered the World Health Organization
(WHO) World Report on Vision.1 More than one billion people experience vision loss primarily because they have no access to vision care. Ninety per cent of those live in low to middle income countries. Nearly 75% are over 50, and 55% are women. Ethnic minorities and Indigenous peoples are overrepresented in these groups. Ninety per cent of vision loss is preventable.
Poor vision creates a global productivity loss of around US$411 billion annually.
The WHO SPECS 2030 initiative envisions a coordinated global action for a world in which everyone who needs refractive error intervention has access to quality, affordable, people-centred services. Improved population education, cost reduction, surveillance, and research are further goals.
LET’S NOT FORGET HYPEROPIA
Keynote speaker Professor Susan Cotter from California started by showing that with all the focus on myopia, hyperopia is being ignored, quoting leading lights in eye care. With the program top heavy in myopia management, it was refreshing to see that other refractive issues were not being forgotten. It’s a serious issue.
Prof Cotter discussed the impact of hyperopia on younger people. Some potential consequences of moderate uncorrected hyperopia in young children included arrested development in the social, emotional, and physical sense. Educational performance and achievement can also be reduced, with direct and indirect economic effects and reduced quality of life influencing both the child and family.
Moderate uncorrected hyperopia led to significantly worse performance on the Test of Preschool Early Literacy in four-to-fiveyear-olds. Greater amounts of hyperopia are associated with slower reading speed. The Matthew effect is a phenomenon where performance differences between good and poor readers increases over time.
SPINNING THE DRY EYE WHEEL
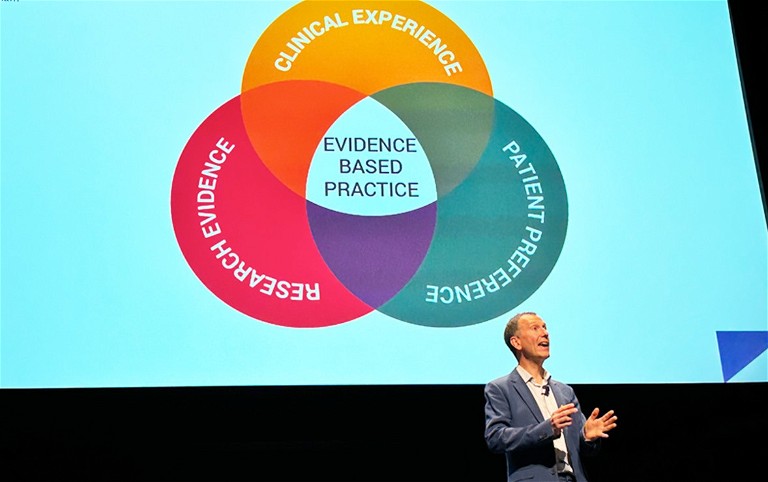
The next keynote address, by ever competent Professor James Wolffsohn of Birmingham, explained that it can take 17 years for research evidence to become sound clinical practice.
He noted how the Tear Film and Ocular Surface Society Dry Eye Workshop (TFOS DEWS) reports demonstrate how groups collaborate and collate research, data, and best practice to create sound guidelines. The nett result is that we should be able to make the same diagnosis, between various practitioners, when faced with a given set of signs and symptoms.
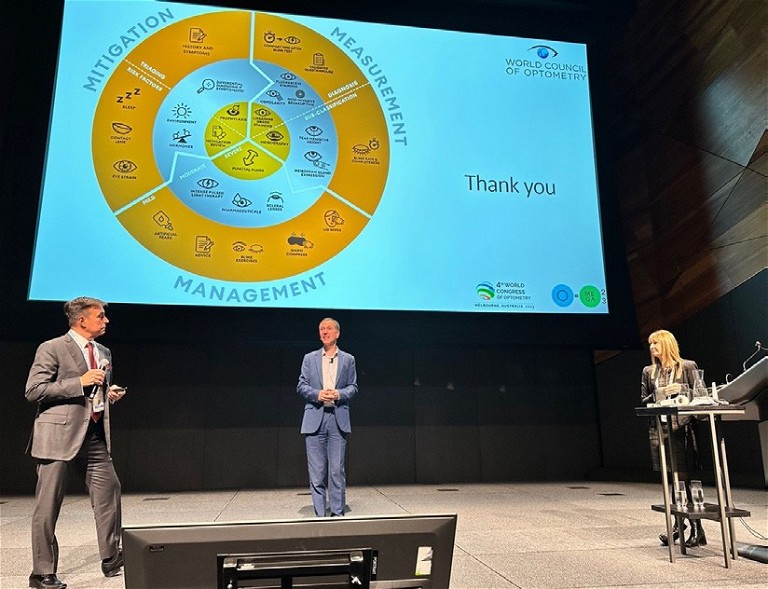
In a following tri-presentation, ‘The dry eye wheel – abetter way to tackle dry eye’, Professors Jennifer Craig (Auckland) and Lyndon Jones (Waterloo) joined Prof Wolffsohn to discuss detailed mitigation, measurement, and management of dry eye. They noted that dry eye is a subset of ocular surface disease and that the symptoms define it as dry eye. Patients need to sleep well, and follow a good diet. Compliance with eye drops is important.
They continued to ‘spin the wheel’ and rotate topics, delving ever deeper into the dry eye wheel, covering a great breadth of issues.
A warm facecloth does not meet the effectivity threshold for heating meibum and baby shampoo has also been shown to be rather ineffective. Today we have much better options with an increasing evidence base of effectivity.
Blink exercises can help manage dry eye. For incomplete blinkers it must be stressed that the eyes must be fully closed during such exercises. Apps can help with such blink training.
Eye drop therapy can be initiated where signs or risk factors of dry eye are noted, before they develop into symptoms.
“ with all the focus on myopia, hyperopia is being ignored ”
They got the audience to not blink and count the seconds before they noted the onset of symptoms – aquick and easy screening test we can do in practice. The average is 12.6 seconds, bigger is better and under 10 seconds is poor. They presented a systematic review of eye drops and modern lipid containing drops for lipid deficient/evaporative dry eye. Eye drops work well but it can take six months for full benefit.
Treat the masqueraders first: Itchy eyes are usually allergy so treat allergies to eliminate them as a cause of ‘dry eye’ symptoms. If one eye is worse, it’s not usually dry eye, nor is it sudden onset. They demonstrated various treatments, appliances, and diagnostic aids, like tear scopes and osmolarity measuring instruments.
SESSION HIGHLIGHTS
Optometrist Hirdesh Nair from Johnson and Johnson Vision spoke on ‘Contact lens wearer’s attitude, behaviours, and needs during and after pandemic restrictions in Australia’. Although COVID-19 reduced contact lens (CL) wear opportunities, their use for work-from-home increased (as did take away foods), while all other categories of CL use dropped – 42% of respondents reduced or completely stopped CL usage. Around eight in 10 cited lack of occasions as the key reason for reducing/stopping CL wear.
Singapore-based Kah Ooi Tan presented on a ‘Preliminary study: Practitioner perceptions of myopia management in China’. There was high interest and perceived knowledge of myopia control but a disconnect in practice. Traditional medicine and culturally accepted beliefs were perceived as effective and readily prescribed. Practitioners lack confidence in prescribing treatments. Parents are aware of myopia but lack awareness/understanding of myopia control and the need for it. The link to future vision impairment was not well known among the surveyed parents, consistent with the WHO 2018 meeting report on developing myopia control strategies.2 There are financial barriers to offering myopia management, one of the reasons why single vision lenses were prescribed over myopia controlling options.
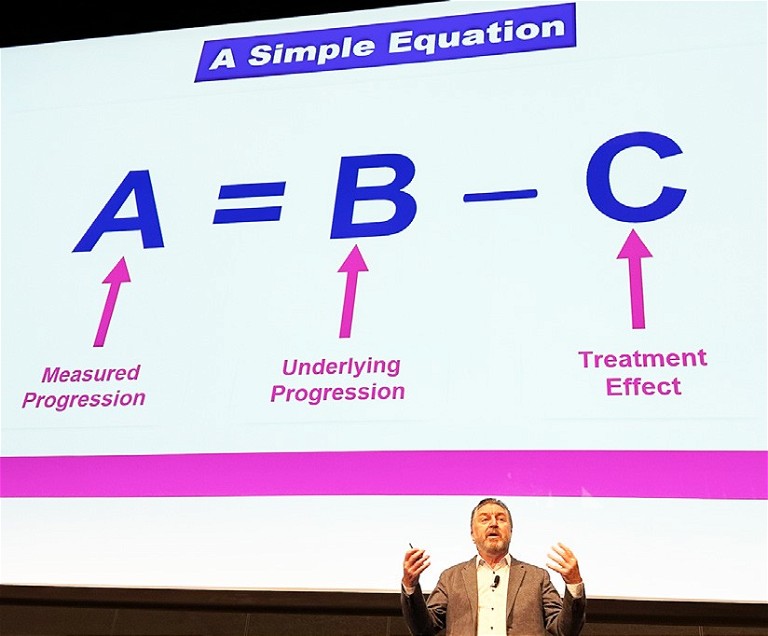
Jacksonville-based Melbournian Dr Noel Brennan was happy to be back in his hometown. His voice was recovering from a night at the Melbourne Cricket Ground watching his team win the footy, but nevertheless he presented ‘A breakthrough soft CL for myopia control?’, with his usual aplomb. With myopia control soft lenses there’s a need to balance efficacy and vision quality. He noted that we can see changes in choroidal thickness in a matter of half an hour, as a marker. The research team simulates and tests different designs with clever technologies to see how they affect such measures and noted that there’s a ‘dose– response’ effect. Lenslets and non-coaxial optics added a fourth mode of controlling efficacy. He discussed enhanced efficacy and enhanced vision designs.
There’s no safe level of myopia: Over 30% of people with myopic macular degeneration are not high myopes. Pathological myopia is already the leading cause of irreversible blindness in Taiwan, Japan, and China.
WCO DAY TWO
Associate Professors Andrew Anderson and Laura Downie from The University of Melbourne presented ‘Computer vision syndrome: Do blue light filtering lenses (and other therapies) help?’.
They explained computer vision syndrome (CVS) as vision related issues arising from prolonged electronic device use, such as blurred vision, dry eyes, redness, and headache. Around 60 million people worldwide suffer from CVS, with one million new cases each year. It’s been claimed that blue light emitted from screens has a role in CVS, and blue-light filtering (‘blue-blocking’) lenses are marketed to reduce CVS. They showed that there’s no hazard of retinal damage from screens. The brightest screen is 10 times less than sunlight exposure on a dull day. Sunlight is significantly more hazardous. Screen use may cause fatigue but ‘blue block’ lenses in their study had no effect in reducing CVS or critical flicker fusion frequency.
In ‘Unanswered questions in myopia management’ Doctors Kate and Paul Gifford, co-founders of Myopia Profile, addressed various issues with their usual style and clarity. Key points were to monitor progression and ocular health and to consider contact lenses. In adult myopia, progression is not just refractive and risk factors are less modifiable. Do young adults experience similar vision outcomes and acceptance as children? The latest white papers from the International Myopia Institute were discussed and they covered what the Myopia Profile site (myopiaprofile.com) offers parents, patients, and practitioners.
Professor James Wolffsohn.
L-R: Professors James Wolffsoh , Lyndon Jones. and Jennifer Craig.
Dr Noel Brennan.
“ They continued to ‘spin the wheel’ and rotate topics, delving ever deeper into the dry eye wheel, covering a great breadth of issues ”
Continuing along the myopia theme, in ‘Myopia: thinking globally, acting locally’ Professor Mark Bullimore delivered an insightful and entertaining talk noting that each dioptre increases visual impairment by 30%. We now have a better understanding of myopia’s role in visual impairment, and the ability to do something about it. We have evidence to treat pre-myopic children: 0.05% atropine can delay myopia onset by a year, which might save 0.75D in the longer term. We should care about the long-term visual health of every patient, not just address their current visual needs. 2050 projections estimate 307 million visually impaired people, with 207 million myopes. Myopia elimination would mean a large reduction in visual impairment. He presented a useful analogy citing the ‘Slip, Slop, Slap’ sun awareness campaign: Short-term benefit is reduced risk of sunburn with long-term benefit of reduced risk of skin cancer. With myopia control, the short-term benefit is better vision while longer-term benefits are reduced risk of eye disease and visual impairment.
In a masterclass session ‘Myopia management in practice – clinical knowledge isn’t enough!’, Matt Oerding, (California) and Dr Emma Gillies (Sydney), explored practical aspects of myopia management business and practice. Avoid complex explanations and mention excessive eye growth as a simple concept to discuss with parents/kids. A website is a key interface with basic information to get them to book an appointment via an online booking option, which is essential to ensure instant conversion. Video content is four- to 10-times more engaging than written content. Testimonials are great but not allowed in Australia. Social media is important with Facebook, Instagram and YouTube covering the different spectra of parents with school age, potentially myopic kids. Google ads and pay per click sponsored sites push you to the top three hits on a search. The cost is easily recouped in your initial consultation.
Johannesburg-based Elizabeth Chetty, a winner of one of the WCO bursary awards, discussed ‘Clinical profiles of keratoconus patients attending a South African specialty lens clinic’. An interesting slide presented prevalence rates in a variety of countries where mild cases represented around 4–15%, with the majority moderate-to-severe. Exceptions were Egypt, where mild cases were 54%, whereas in Kenya 71% of cases were severe.
Dr Chetty shared two interesting cases of keratoconus (KC) in oculocutaneous albinism sufferers. She noted that, like myopia, the younger KC manifests, the more severe the disease and that it is most prevalent in the non-Caucasian population.
THE HOME STRAIGHT
There was a strong theme covering Indigenous eye care and issues throughout the congress. Ophthalmic photographer James Rule ( Victoria) kicked off Sunday’s talks with ‘Retinal photography screening for diabetic retinopathy in Victorian Aboriginal Community Controlled Health Organisations (ACCHO)’. He noted that Indigenous Australians have poorer health outcomes with shorter life expectancy, with greater burden for a variety of conditions, including eye disease. Type 2 diabetes and diabetic retinopathy (DR) is a major issue: DR has more than doubled in the past two decades and is at 5.2% compared to 1.7% in the non-Indigenous population, with earlier onset by as much as 20 years. This increases the burden in terms of disability, loss of income, and ability to work. Unfortunately, many do not seek treatment, due to poor health literacy and lack of access.
Despite 17 non-mydriatic retinal cameras installed at Victorian ACCHOs, these cameras are – alarmingly – currently unused due to staffing issues. Cultural sensitivities in photographing family members and discussing the results were also noted. The situation does not provide an effective, safe, quality, health care service.
A homegrown innovation on display in the Congress exhibition might offer some solutions. Eyetelligence is an amazing battery powered, tablet-driven, shoe-box- sized, compact retinal camera. All a patient needs to do is follow voice prompts to look at a target and keep eyes open, so little or no training is needed. Artificial intelligence (AI) software instantly analyses the images, providing a cardiovascular health score and assessment of presence (with grading) or absence of diabetic retinopathy. Such compact systems can easily be transported and should be a boon for remote and Indigenous eye care.
MYOPIA
Professor Kathryn Saunders (Ulster), Doctors May Zhang (Singapore) and SooJin Nam (Sydney) shared a broad view of evidence and practice, providing valuable insights in their session ‘Lighting the way: new evidence and advances in myopia management’. Prof Saunders showed that defocus incorporated multiple segments (DIMS) based lenses were well tolerated with few or no symptoms and noted that 44% had <0.25D annual myopic change. Twenty-two per cent showed no change or reduction in myopia, comparing favourably with myopia control contact lenses. Children with bigger pupils showed significantly less myopic progression/axial growth. Dr Zhang highlighted evidence that shows a 60% myopia progression reduction over two years with a sustained myopia control effect over six years.

Associate Professor Petere Hendicott.

Dr Daniel Tilia.
Advice that children spend at least two hours a day outdoors is a significant parameter associated with preventing myopia development in school children and has been widely adopted. With this time outdoors, sunglasses or photochromic lenses are advised and are available in such myopia controlling lenses. Around 80% of parents were on board with sun protection options.
Dr Nam detailed myopia risk factors and atropine use – usually in addition to myopia controlling spectacles/contact lenses. She elaborated on how she explains myopia control options to parents and children, and presented interesting case studies relating each case to individual risk factors.
RETINAL PROSTHESES, PARKINSON’S DISEASE, AND MORE
In a talk, ‘Functional vision outcomes with a suprachoroidal retinal prosthesis in retinitis pigmentosa’, Dr Carla Abbott discussed the pros and cons of the various types of retinal prostheses, testing procedures, and results. Those with the device were 80% more successful in object avoidance than without.
In ‘Examination of visual measures in Parkinson’s disease’, Dr Katie Tran (Melbourne) explained the symptoms and underlying retinal features in Parkinson’s disease (PD) patients. Retinal dopamine deficiencies occur in PD. The condition leads to compromised retinal heath and cell responses. Optical coherence tomography (OCT) detects changes in retinal structure while electroretinography measures changes in retinal function. Changes in colour vision also occur.
“ There were about 108 posters presented in well-attended poster sessions in the exhibition hall during lunch breaks ”
Jagrut Lallu (New Zealand) shared valuable insights and tips in ‘Getting started with topography and orthokeratology using topography-based lens designs’. He made light work of it and a giant screen made for some impressive images. Mr Lallu encouraged less experienced practitioners to take on this trending method for successful CL fitting and management.
Just short of the end of three long days of education, Associate Professor Elena Biffi from Boston delivered an outstanding presentation on ‘Multimodal Imaging approaches to diagnosis of age-related macular degeneration’. In what is usually a dry topic on a leading cause of irreversible blindness in the over 65s, those present agreed that she did a remarkable job of succinctly illustrating the key points. She featured OCT and other imaging modes to aid differential diagnosis for a variety of macular degeneration conditions. Prevalence increases significantly after 50, is responsible for around 46% of cases of severe vision loss >6/60 in the over 40s, with 18% prevalence after age 85. There are 200 million affected worldwide, and this is predicted to increase to 288 million by 2040. She described various methods for diagnosing and tracking, explaining specific protocols and what instruments, settings, and filters to apply to best determine the defining features of each specific condition, including fundus autofluorescence, various OCT and angiography strategies.
In an adjacent room, it was standing room only for those attending a related session presented by the ever-popular Michael Yapp on ‘Choroidal neovascular membranes – how not to miss one’.
There were about 108 posters presented in well-attended poster sessions in the exhibition hall during lunch breaks. Presenters from 34 countries interacted with delegates, sharing the finer points of a broad selection of topics. Poster topics can be seen via this link; omegaevent.org/program, with additional links to the lecture program.
By all accounts, O=MEGA23/WCO was a great success and a fine effort.
References
1. World Health Organization. (2019) World report on vision, avail at: who.int/publications/i/item/9789241516570 [accessed 15 Sept 2023].
2. World Health Organization. Regional Office for the Western Pacific. (2018). Meeting on Developing Myopia Control Strategies, Singapore, 13–14 November 2018: meeting report, avail at: apps.who.int/iris/handle/10665/325951 [accessed 15 Sept 2023].

L to R: Dr Paul Gifford, Joe Tanner, Dr Kate Gifford and Dr Mark Bullimore.

L to R: Dr Philip Cheng, Dr Michelle Waugh, and Dr Noel Brennan.