mitechnology
WRITERS Adjunct Associate Professor Tze Lai and Dr Nicholas Ong
Towards the Light: IPL and Rexon-Eye for Dry Eye Treatment
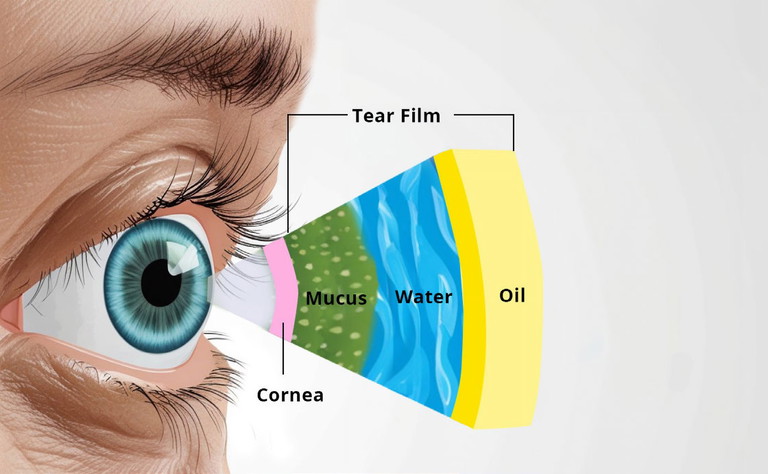
Figure 1. Layers in normal tear film.
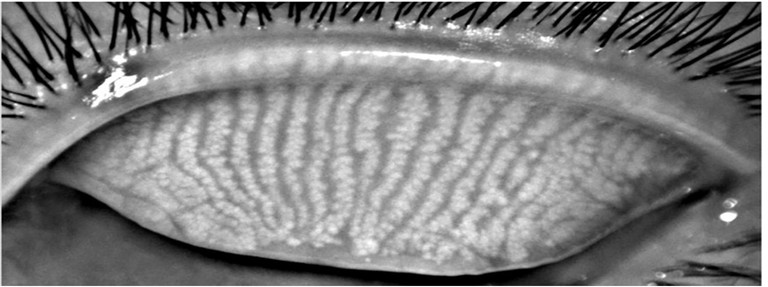
Figure 2: Normal meibomian gland, with glands running parallel and for the full length of the eye lid. Images courtesy of the Clinical Research Centre, University of California Berkley.6
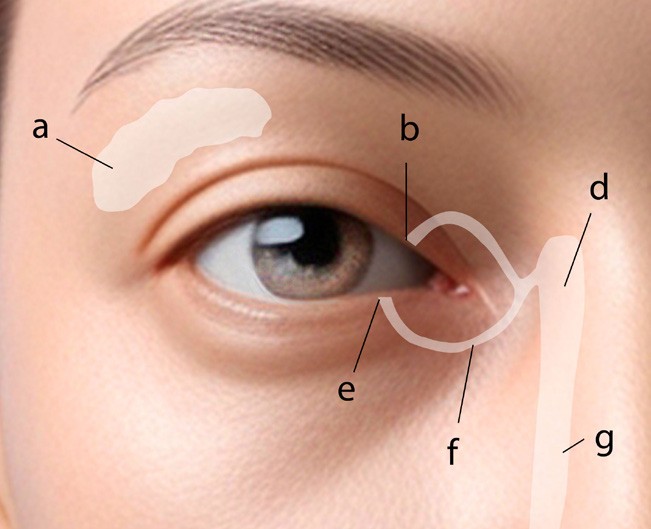
Figure 3: Tear system: a. tear gland / lacrimal gland, b. superior lacrimal punctum, c. superior lacrimal canal, d. tear sac / lacrimal sac, e. inferior lacrimal punctum, f. inferior lacrimal canal, g. nasolacrimal canal.7
With the burden of dry eye disease increasing, intense pulsed light (IPL) treatment and quantum molecular resonance (QMR) electrotherapy are proving to be useful tools in the dry eye armamentarium.
In this article, Adjunct Associate Professor Tze Lai and Dr Nicholas Ong review both the science behind the technology, and provide a useful guide as to how it has been incorporated into clinical practice at WA Eye Specialists.
Dry eye disease (DED) affects up to 50 million people worldwide and is driven by tear film hyperosmolarity (hyper-concentration of salts), structural instability, and rapid evaporation.1,2 In a normal tear film, there are three different layers of meibum (oil), aqueous (water), and mucous (proteins/carbohydrates) at fixed compositions that work in conjunction to lubricate and nourish the ocular surface.3
The meibum produced by the meibomian glands just beneath the eyelids is of a freeflowing olive oil texture that coats the surface of the eye, keeping the moisture locked in and preventing rapid evaporation.3-5 The aqueous produced by the lacrimal gland maintains the proper balance of electrolytes within the tear film, while the mucous produced by the goblet cells of the conjunctiva helps to provide additional lubrication.3
The causes for DED are multifactorial and range from various environmental factors, medical conditions/procedures, medications, diet, and changes to physiology,3 summarised in Table 1.8 The disease itself can be segregated into three different categories; aqueous deficient dry eye (ADDE), evaporative dry eye (EDE) or a combination of both.8 ADDE is characterised by a dysfunction in the production of aqueous by conditions affecting the lacrimal gland, resulting in hyper concentration of the salt content within the tear film, leading to early break down, and rapid evaporation.8 EDE, on the other hand, is primarily due to reduced meibum production, either from gland drop out or thickening of the meibum, which can subsequently occlude and cause the remaining glands to atrophy.9-12 Similar to the unstable tear film in ADDE, the loss of the moisture retaining oil also results in quicker evaporation, tear film instability, and hyper concentration of the salt content within the tear film.3,13
MEIBOMIAN GLAND DYSFUNCTION
As most DED globally is caused by EDE and characterised by meibomian gland dysfunction (MGD),4,5,8,14,15 this article focusses on the causes of MGD and treatment.
While initially unnoticeable, prolonged MGD can lead to symptoms typical of dry eye disease such as: grittiness, burning, itch, pain, blurry vision, excessive tears, redness, foreign body sensation, and abnormal blood vessel growth (telangiectasias).16,17 If MGD is allowed to continue untreated, the remaining glands that become occluded can further atrophy, resulting in worsening dry eye symptoms.14,15,17
All forms of DED are associated with poorer quality of life scores. In a cross-sectional study of 78,165 participants, DED was associated with poorer physical and mental health outcomes compared to those that did not suffer from DED.18
At our own dry eye clinics at WA Eye Specialists, we have noted that 60% of clients have reported symptoms that were subjectively moderate to severe, with 48% reporting that their DED had a significant impact on quality of life, either limiting function or affecting the performance of tasks (Table 2).
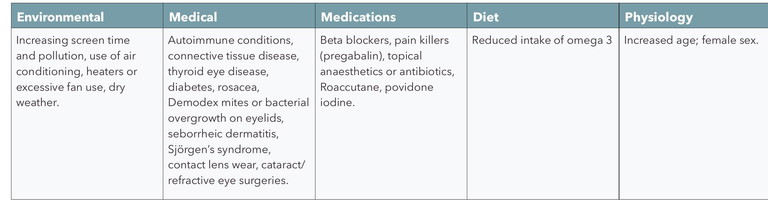
Table 1. Common causes of DED.8
Unmodifiable Risk Factors
DED is more common in females (76%) compared with males (20%).8 Since the meibomian glands are regulated by circulating androgen sex hormones that are higher in concentration in men, it is not surprising that comparatively more women experience DED.8,19,20 Increasing age was also a risk factor for MGD associated DED.8 As people age, circulating androgen levels tend to decline, which can further compound the dysregulation of the meibomian glands.19-21 This could explain why most (70%) of the clients attending our dry eye clinics are between 60–80 years old.22
MODIFIABLE RISK FACTORS
Increased screen time is a modifiable risk factor for MGD8,23-26 as use of screens affects blinking characteristics by reducing blink rate and complete blinks, which in turn reduces the lipid spread over the ocular surface, resulting in increased evaporation.24 Not just limited to adults, increased screen time has also been associated with MGD in children as young as four years old.16,25-27
Given screens are now ubiquitous, it is important to provide patients with advice regarding the importance of taking short breaks from extensive screen use.28
From our own patient questionnaires, we found that 20–25% of clients experienced subjective worsening of their DED post cataract or LASIK (laser assisted in situ keratomileusis) surgery, a well-known phenomenon.29,30 As patients undergoing cataract surgery tend to be older (pre-existing risk factor) with other medical comorbidities such as diabetes, they are already predisposed to developing post-surgical exacerbations of their DED.8,31 Moreover, intraoperative preparation of the eye with povidone iodine for longer than 30 seconds has been associated with ocular toxicity that may further precipitate MGD.32,33
Manipulation of the cornea during surgery has been shown to disrupt the corneal nerve plexus, reducing corneal sensitivity, increasing blink rate, and worsening tear film instability.30,34 On top of the pre-operative and intra-operative risk factors, the use of topical anti-inflammatory or topical antibiotics is common practice after surgeries, which can damage the ocular surface if used for prolonged periods of time.32
TREATMENTS
Given the link between surgery and worsening of DED symptoms discussed above, improvement of client satisfaction may require optimisation of all conditions before, during, and after the operation. For example, studies have shown improvement in symptoms of post-operative DED through three intense pulsed light (IPL) sessions spaced two weeks apart prior to eye surgery.35,36 Proper counselling, screening for DED with meibography, treatment with perioperative IPL, and reduction of the duration of ocular toxic medications may aid with symptom reduction and client satisfaction post-operatively.32
Additionally, there may also be a role in early treatment and regeneration of the meibomian glands with novel therapies, such as IPL therapy or quantum molecular resonance electrotherapy (QMR or Rexon-Eye).37-47
Currently, the mainstay of treatments for MGD includes lid hygiene wipes, topical antibacterial drops, topical lubricant drops, topical antiinflammatories, or supplementation with foods rich in omega 3, which only results in a temporary resolution of symptoms.15,41,43,46,48,49 In our patient survey, we found 42% of clients were still using eye drops after one year, with 31% hoping to reduce their dependence on drops for symptom control. One study has reported that adherence to prescribed therapies such as eye drops could be as low as 10%.48 Oftentimes, because of the combinations of short-term relief, lack of commitment, poor adherence or sudden cessation, the return of dry eye symptoms is not uncommon.50

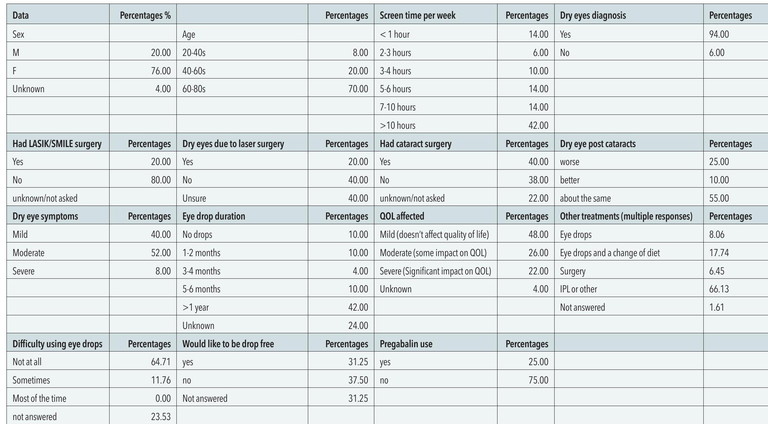
Table 2. Summary of data from WA Eye Specialists’ patient questionnaire. QOL = quality of life.
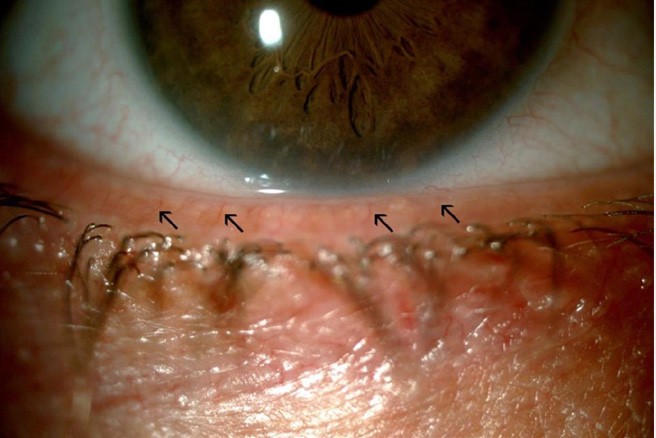
Figure 4. Black arrows show abnormal blood vessels, grey arrows show meibomian gland obstruction.12
INTENSE PULSED LIGHT AND REXON-EYE
Use of IPL or Rexon-Eye in conjunction with other dry eye therapies has been shown in numerous studies to improve overall meibomian gland flow and function, as well providing secondary anti-bacterial and anti-inflammatory effects over an extended period of time.39-46
Initially used for dermatology and skin rejuvenation, the use of IPL was also noted to incidentally improve dry eye symptoms.42,51 By pulsing a light through a 500 nm filter in contact with the skin, the light is absorbed as heat in the meibomian glands, liquefying the viscous oil making the flow easier.42,51 Apart from enhancing oil flow, IPL is also useful in the treatment of blepharitis or eye lid inflammation caused by accumulation of bacteria and mites known as demodex along the lid margins.52 The associated inflammatory responses of the body to the bacteria or mites are a well-known cause of MGD.40,42,51 In IPL, the intense light and heat generated eradicates the demodex and bacteria and coagulates abnormal blood vessels, through which flow various pro-inflammatory mediators, which can occlude and further damage the existing meibomian glands.42,51 This creates a conducive environment for the damaged meibomian glands to recuperate and to be restored to original viability.42,51 With RexonEye, instead of light, heat is generated through high frequency electric currents.53 Rexon-Eye’s QMR technology employs low-power, highfrequency electric fields to stimulate cellular metabolism and natural regeneration as well as reduce inflammation. It treats both meibomian glands as well as the lacrimal glands and has the benefit of treating clients who suffer from a combination of both ADDE and EDE.38,47,54
TREATMENT PLANS
At a patient’s first visit to the clinic, an initial assessment is performed to assess the overall health of the ocular surface. This should include measuring the tear break-up time (TBUT), tear meniscus height, meibography, close up photos of telangiectasias/eye lid pathologies, and measuring the damage to the cornea with fluorescein dye.
After assessment, the treating dry eye clinician would generally recommend four initial sessions spaced two to four weeks apart and then four booster IPL sessions, with appointments for boosters separated across a period of three months to a year, depending on a client’s symptoms.37 The treatment schedule for Rexon-Eye is similar, with a recommendation for four initial treatments, each spaced one week apart.38 If a weekly session is not possible, the treatment for Rexon-Eye can be conducted every second week.
WHAT HAPPENS DURING TREATMENT?
At each treatment for IPL, the eyes are covered with eye shields and medical grade gel is applied to the malar region of the face. The appropriate filter is installed into the machine and the power settings can be adjusted up or down according to client comfort. The IPL probe is placed on a client’s lower lids and individual pulses of light are delivered at regularly spaced intervals from tragus to tragus. This is known as the first ‘pass’ and there two passes for each treatment.
For the Rexon-Eye treatment, the eyes are covered with a disposable tissue and the eye mask is fitted snugly. The power settings are adjusted, starting with ‘5’ and the eye mask is left on for 20 minutes.38 The eyes are treated one at a time with short intervals between each eye.
Sunscreen is applied after both treatment options and clients must be educated to avoid excess sun exposure/heat after treatment.40,47
EFFECTS
Most effects of improved meibomian gland function with IPL and Rexon-Eye can be seen immediately, with effects lasting anywhere from days to weeks after the first two sessions. The effectiveness of the treatments extends with each session, with relief of symptoms lasting for six to eight months after completion of the four treatments.37,38

COMPARING THE TWO
Currently, there are no studies comparing benefits between IPL and Rexon-Eye for the treatment of MGD and DED. Both treatments are very safe with most clients only reporting a slight increased warmth of the skin.37,38,42 When deciding on the treatments, there are a few features of each modality to consider, which I have outlined below.
“Meibomian gland dysfunction is the leading cause of dry eye disease with risk factors being female sex, age, cataract/ LASIK surgeries, increased screen time and other factors”
Intense Pulsed Light
The intense light of IPL is absorbed by pigments within the skin, which helps to rejuvenate meibomian glands as well as lighten dark spots.55 Another advantage of IPL is that it is a quick procedure, taking only 10 to 20 minutes from set up to treatment.42,51 Unfortunately, the advantage that IPL has in lightening dark pigments also becomes its disadvantage. Since all pigments absorb light which is then converted to heat, IPL cannot be used in clients with Fitzpatrick IV skin types and above, as the heat absorbed may be too intense, leading to severe burns.42
Rexon-Eye
As mentioned above, Rexon-Eye uses high frequency electric currents instead of light. The heat generated is localised and can therefore be used in all skin tones. Another added benefit of Rexon-Eye is that it stimulates and promotes the natural regeneration of cells, which may improve both meibomian and lacrimal gland function.47,53,56
TAKE HOME POINTS
DED causes significant stress to clients and can significantly impact quality of life.
Meibomian gland dysfunction is the leading cause of dry eye disease with risk factors being female sex, age, cataract/LASIK surgeries, increased screen time and other factors.
Given the large burden of DED, which will only increase over time, it is important to optimise ocular surface health by offering screening processes, providing good perioperative counselling, advising on screen time reduction/taking more frequent breaks, reducing duration of ocular toxic chemicals, and making referrals for perioperative IPL/Rexon-Eye treatments.
The use of novel treatments like IPL and Rexon-Eye, together with conventional DED treatments, have been shown to improve long-term control of symptoms by reducing eyelid inflammation and liquefying the meibum within the glands. Sessions spaced two to four weeks apart have shown good symptom relief for up to 18 months and early referral should be considered.
Adjunct Associate Professor Tze Lai MBBS BMedSc MPHC FRANZCO completed her ophthalmology specialist training in Western Australia prior to undertaking an internationally renowned surgical fellowship subspecialising in complex cataract and glaucoma surgery (including minimal invasive glaucoma surgery), in Toronto, Canada. She practises in Perth at WA Eye Specialists and St John of God Healthcare.
Dr Nicholas Ong is a medical doctor who graduated from the University of Western Australia and practises at the Saint John of God health groups in Perth. He has a special interest in ophthalmology and is currently working on a dry eye disease research project with Adj Prof Lai at the WA Eye Specialists.
References available at mivision.com.au.
