The MYOPIA ISSUE
mieducation
Atropine and Myopia Management
Low dose atropine has been integrated into the management of childhood myopia progression. Drs Linda Zheng and Caroline Catt detail the practicalities of prescribing and monitoring the effect of treatment.
WRITERS Dr Linda Zheng and Dr Caroline Catt
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Know about atropine for the treatment of myopia, what doses can be used, and its side effects,
2. Know how to define high myopia, and
3.Understand the causes of myopia and its complications.
Myopia is a condition in which the spherical equivalent refractive error of an eye is ≤−0.5D when ocular accommodation is relaxed. Low myopia is a condition in which the spherical equivalent refractive error of an eye is ≤−0.5D and >−6.00D when ocular accommodation is relaxed (accompanied by an axial length <26mm). High myopia is a condition in which the spherical equivalent refractive error of an eye is ≤−6.00D when ocular accommodation is relaxed (accompanied by an axial length ≥26mm).
Ocular morbidity due to myopia increases per dioptre and per mm of axial length, and includes myopic macular degeneration, retinal detachment, primary open angle glaucoma, macular hole, retinoschisis, and nuclear and posterior subcapsular cataract.
AETIOLOGY OF MYOPIA
Animal experiments have shown that myopia is not driven by excessive accommodation, but predominantly by hyperopic projection of light on the peripheral retina (peripheral defocus). The current consensus is that light projection on the retina triggers a signalling cascade, which flows into the sclera via the retina, retinal pigment epithelium (RPE), and choroid. There, re-modulation of collagen structures takes place, making the eye longer. The molecular structure of the signalling cascade is slowly becoming clearer, and dopamine is deemed to be an important player. Animal experiments have shown that this neurotransmitter is secreted by the amacrine cells after light exposure and acts as a stop signal for growth. Atropine increases dopamine levels in the retina, which inhibits eye growth. Another effect of atropine is an increase in nitric oxide (NO), which can also serve as a mediator of eye growth.1
WHEN TO START ATROPINE
Consider commencing atropine when there is evidence of myopia progression across two visits, with a proven increase in refractive error and axial length.
LOW DOSE ATROPINE EVIDENCE
There have now been randomised controlled studies (ATOM 1 and 2 and LAMP Studies) that support the use of low dose atropine in slowing myopia progression.
ATOM 1 and 2: Main Summary Points
• Randomised controlled study of 400 children who received atropine 0.5%, 0.1%, or 0.01% atropine.
• 24 months of treatment (Phase 1), then a 12-month washout period (Phase 2).
• Children who progressed in Phase 2 were restarted on 0.01% atropine for 24 months.
• The decrease in spherical equivalent was significant for all concentrations, however the decrease in axial length growth was only significant for atropine 0.5% and 0.1%.
• When treatment was discontinued after two years, a rebound effect of refractive error was observed for high dosages (0.5% and 1.0%), however axial length was still most reduced for these concentrations.
• There was a dose-related response to slowing myopia progression.2
LAMP Study: Main Summary Points
• Randomised controlled study of 383 children over two years of age comparing 0.05%, 0.025%, and 0.01% atropine with placebo.
• After Phase 1 (Year 1) all children on placebo were switched over to 0.05% atropine. The rest of the children were continued on the same doses in the second year.
• In Phase 2 (Year 2) the efficacy of 0.05% atropine observed was double that observed with 0.01% atropine.
• Phase 3 (Year 3) saw half of the children continue with 0.05%, 0.025% or 0.01% treatment and the other half ceased, to test for a rebound effect. Progression was faster in the non-treated groups, and the formerly 0.05% group showed a slightly faster ‘rebound’ but only by around 0.04mm over one year, which was considered clinically insignificant. Younger children (six to eight years) were more likely to show greater rebound.
• 0.05% is the most effective of the low dosages, but still not as effective as the higher dosages 0.1% and 0.5%.3
TITRATING AND WEANING ATROPINE
Atropine dosage can be titrated up if there is still progression despite treatment. Atropine dosage can be titrated down if there are significant side effects to treatment or if there is no significant myopia progression for one to two years.
The aim is to wean the dose of atropine slowly to prevent the rebound effect that often occurs with abrupt cessation.
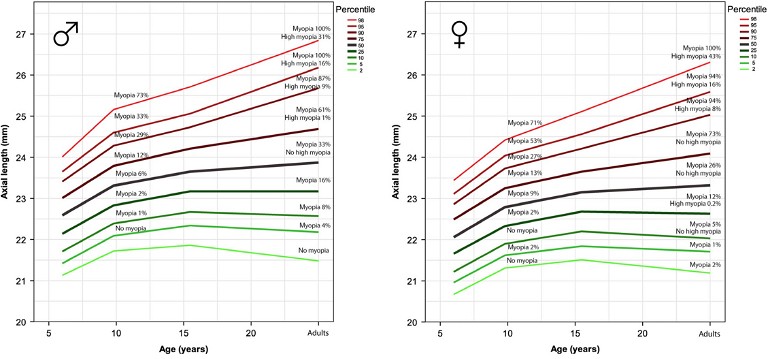
Table 1: Table from Rotterdam study plotting age and axial length showing the percentile risk of developing high myopia.4
HIGH MYOPIA TREATMENT
High concentration atropine (0.5%–1.0%) has been shown to have the most reduction in axial length progression but has drawbacks of light sensitivity and loss of accommodation.
When these side effects are mitigated by multifocal photochromatic glasses, the long-term adherence to high dose atropine is high. High dose atropine can be considered in patients at risk of high myopia and progressing despite all other treatments.
In our Australian population of children, high concentration atropine is rarely used.
Rotterdam Study: Main Summary Points
• Investigated the real-world effectiveness of high dose atropine (0.5%) for high myopia in European children.
• Seventy-seven myopic children with mean age 10.34 (±3.21), axial length> 75th percentile, and myopia progression> 1D per year were treated with atropine 0.5%. After one year, progression was 0.04mm per year, 0.16mm per year for the second year and 0.14mm per year for the third year.
• In the study, 78% of the children adhered well to the treatment; however, children frequently reported photophobia (72%) and reading problems (38%). The largest dropout occurred within the first month, after which it seemed easier for the children to tolerate the side effects.
• It was reported that 74% managed to progress < 0.2mm per year after three years. This was significantly less than the 0.34mm per year progression for non-treated children with axial length >75th percentile in the population-based children cohort Generation R, which served as a reference group.
• With multifocal, photochromic optical spectacle correction, 73% of the children were able to adhere to treatment for the entire three-year study period. These glasses should be prescribed as first line to children who are having issues tolerating the side effects of atropine treatment.4
Table 1 from the Rotterdam Study shows the percentile risk of developing high myopia.4 Axial lengths on the 75th percentile or higher are at risk of high myopia. These lengths should be targeted with the most effective regimens, as only minimal progression will prevent high myopia in adulthood. Axial lengths below the 75th percentile can cope with a more relaxed control with low dose atropine.
OTHER CONSERVATIVE METHODS TO HALT PROGRESSION
Outdoor Time
The protective effect of being outside is currently explained by a high light intensity leading to a higher retinal dopamine secretion. Outdoor time and sunlight have been shown to decrease onset of myopia and prevent progression.5 We support advising every patient with myopia or at risk of myopia (‘premyopia’) about the importance of natural light play and encourage spending a minimum of two hours per day outside, taking the usual measures for sun protection including sunscreen, hats, sunglasses, and seeking shade.
Orthokeratology
The compressive effect of orthokeratology (OK) lenses provide myopic defocus in the peripheral retina. Orthokeratology can correct myopia up to −6D without optical aids in the daytime. Orthokeratology and night-time contact lens wear in children has the risks of virulent bacterial and anaerobic keratitis that can lead to permanent vision loss.6
Peripheral Hyperopic Spectacle Lenses and Contact Lenses
These lenses can have a gradual increase of plus addition in the periphery to create optical myopia correction at the macula, and a myopic defocus in the periphery. This prevents the hyperopic defocus in the periphery that is theorised to lead to myopia progression. These lenses are useful for mildto-moderate myopia but not high myopia.
MiyoSmart lenses correct the refractive error in the central visual axis and have Defocus Incorporated Multiple Segments (DIMS) – honeycomb-shaped segments in the peripheral treatment zone – to provide myopic defocus on the peripheral retina to slow down myopia progression (Figure 1). A two-year clinical trial showed that daily use of MiyoSmart spectacle lenses slowed down myopia progression on average by 60% compared with standard single vision lenses.7

Figure 1. Defocus Incorporated Multiple Segments (DIMS) design used in HOYA’s MiyoSmart lenses.7
Essilor Stellest lenses also provide a central clear zone for refractive error correction and work using 11 peripheral rings of aspherical lenslets (highly aspherical lenslet target (H.A.L.T.) technology) that create a volume of myopic defocus (VoMD) (Figures 2 and 3). This creates a spread of non-focussed light rather than the single focus power. It is proposed that this VoMD creates an even more significant slow-down signal for axial length growth and has been supported by the outcomes of animal model studies. One-year and two-year randomised control trial data in children who wore Essilor Stellest lenses for at least 12 hours per day, seven days per week showed that their final axial length and myopia was respectively 0.41mm and 0.99D less than children who wore single vision spectacles.8,9
TREATMENT PEARLS
• Follow up examinations with measurements of refractive error and axial length should take place every six months, and atropine concentrations can be increased or reduced depending on the progression of axial length.
• The axial length at follow up should be plotted in the growth curves, allowing visualisation of the reduction in axial length percentile high myopia risk profile.

Figure 2. Highly Aspherical Lenslet Target ‘H.A.L.T.’ technology used in Essilor Stellest lenses. Image courtesy of Myopia Profile.
• Treatment will generally take place up to age 15 years or beyond. When axial length has stabilised (growth < 0.1mm year) for more than a year, the atropine concentration can be gradually tapered to prevent rebound effect.
• Treatment can be stopped when significant axial elongation is no longer expected (axial length growth ≤0.05mm year).
• Some children in the highest percentiles may need to continue treatment after their 15th birthday.

Figure 3. H.A.L.T. technology creates a spread of non-focussed light rather than the single focus power.8
To earn your CPD hours from this article, visit mieducation.com/atropine-and-myopiamanagement.
This article was sponsored by Aspen Austalia.
References
1. Smith, E.L. 3rd, Kee, C.S., Ramamirtham, R., et al., Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci 2005; 46: 3965–3972. 2. Chia, A., Lu, Q.S., Tan, D., Five-year clinical trial on atropine for the treatment of Myopia 2: Myopia Control with Atropine 0.01% Eyedrops. Ophthalmology. 2016 Feb;123(2):391–399. DOI: 10.1016/j.ophtha.2015.07.004. Epub 2015 Aug 11. PMID: 26271839.
3. Yam, J.C., Zhang, X.J., Zhang, Y., et al., Three-year clinical trial of low-concentration atropine for myopia progression (LAMP) study: Continued Versus Washout: Phase 3 Report. Ophthalmology. 2022 Mar;129(3):308–321. DOI: 10.1016/j. ophtha.2021.10.002. Epub 2021 Oct 7. PMID: 34627809.
4. Klaver, C., Polling, J.R., Erasmus Myopia Research Group. Myopia management in the Netherlands. Ophthalmic Physiol Opt. 2020 Mar;40(2):230–240. DOI: 10.1111/ opo.12676. PMID: 32202320.
5. Xiong, S., Sankaridurg, P., Naduvilath, T. et al., Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol 2017; 95: 551–566.
6. Sun, Y., Xu, F., Zhang, T. et al., Orthokeratology to control myopia progression: a meta-analysis. PLoS ONE 2015; 10: e0124535.
7. Lam, C.S.Y., Tang, W.C., Tse, D.Y., et al., Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomized clinical trial. British Journal of Ophthalmology. Published Online First: 29 May 2019. DOI: 10.1136/.
8. Bao, J., Yang, A., Huang, Y., et al., One-year myopia control efficacy of spectacle lenses with aspherical lenslets. Br J Ophthalmol. 2022 Aug;106(8):1171–1176.
9. Bao, J., Huang, Y., Li, X., et al., Spectacle lenses with aspherical lenslets for myopia control vs single-vision spectacle lenses: A randomized clinical trial. JAMA Ophthalmol. 2022 May 1;140(5):472–478.

Dr Linda Zheng MBBS(Hons) MMed FRANZCO is a comprehensive ophthalmologist who treats both adult and paediatric ophthalmology patients. She studied at the University of New South Wales with Honours, and completed a further Masters of Medicine at the University of Sydney and a Fellowship at Westmead Children’s Hospital.
Dr Zheng is currently a Consultant Ophthalmologist at Royal Prince Alfred Hospital, Sydney Children’s Hospital Randwick, and The Children’s Hospital Westmead, and has private consultation rooms across Sydney.

Dr Caroline Catt MBBS MMed(OphthSc) BMedSc FRANZCO is a highly trained and skilled eye surgeon, with expertise in both adult and paediatric eye surgery. She has studied at The University of Sydney and The Flinders University, South Australia and completed a Fellowship position in Toronto Canada.
Since returning to Australia, Dr Catt has worked as a consultant paediatric and adult ophthalmologist and eye surgeon at Sydney Eye Hospital and the Children’s Hospital at Westmead. She is the ophthalmologist for the Liverpool Hospital Neonatal Intensive Care unit, a partner at Sydney Ophthalmic Specialists in Sydney, and also works at St Leonards Eye Centre.