mieducation
Halting the Myopia Tsunami: Why Starting Early Matters
Myopia management has come a long way in a very short time. We have a better understanding about the risk factors for myopia onset and progression, especially the role of outdoor time and near work. There is now a bigger range of optical interventions (incredible that we started with just orthokeratology (OK)), the application of low dose atropine, and, of course, the increased popularity of combination treatment. Even so, many questions remain unanswered, including being able to predict accurately who will develop myopia (and when) and how to best customise the current treatment options to improve long-term outcomes. This article will explore the current understanding of myopia risk factors that are clinically relevant.
WRITERS Soojin Nam
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Realise the need to adopt the globally agreed myopia standard of care,
2. Understand the modifiable and non-modifiable risk factors for onset of myopia,
3. Be aware of screening tools for pre-myopia and myopia, and
4. Be aware of existing and emerging myopia management techniques.
The late Professor Brien Holden predicted that 50% of the world’s population would be myopic by 2050 and 10% would have high myopia.1 The relevance of this paper, which was published back in 2016, lives on in the Update on Global Prevalence by the Institute of Myopia Management (IMI) that will be published later this year.2
MYOPIA MANAGEMENT IS THE STANDARD OF CARE
Optometry Australia issued a new position statement on myopia management in June 2024,3 supporting the 2021 World Council of Optometry Resolution on The Standards of Care for Myopia Management,4 which essentially stated that just correcting myopia refractive error wasn’t enough anymore. This shouldn’t come as a surprise as it comes off the back of recommendations made, as far back as 2018, by the Australia and New Zealand Child Myopia Working Group on standards of care for the management of myopia.5 And it is reassuring to know that the eye care profession is on the same page with the World Society of Paediatric Ophthalmology and Strabismus, which released a resolution in 2023 stating, “There is sufficient evidence to warrant the adoption of myopia prevention and control measures in clinical practice in children with progressive myopia of childhood”.6
With this background in mind, as eye care professionals, there is a compelling ethical and legal obligation to provide patients with evidence-based myopia management.
WHERE TO START
Start with the clinical procedures conducted within your consulting room. This is not about re-inventing the wheel but checking in to see if your myopia management protocol follows international guidelines for best practice. The ‘Clinical Tests’ table from 20197 is still relevant (Figure 1), you just need to include interventions available from your practice.
RISK FACTORS
There is ongoing research on trying to understand the risk factors associated with myopia, particularly in regions of high myopia prevalence.8 We can break them down into two groups: risk factors you can do something about (modifiable risks), and risk factors that you can’t influence but need to be aware of (non-modifiable risks).
• Non-modifiable risk factors include parental myopia, age at onset, near esophoria, and high lag of accommodation.
• Modifiable risk factors include environmental factors such as exposure to outdoor light and near work activities.9
When reviewing the risk factors, ‘The Myopia Progression Risk Assessment Score’ (MPRAS) model10 may be a useful tool for clinicians to identify whether patients with myopia are at risk, low risk or high risk for myopia progression. Another useful guide to calculate the risk of myopia onset is the ‘Risk score system for myopia symptom warning’.11
These tools may help identify the high-risk myopes, as they warrant a more aggressive treatment, such as combination therapies, due to their higher risk of ocular pathology.
Understanding the risks inherent to the individual patient allows for customisation of their myopia management. However, patient engagement is the key to compliance, as it ultimately impacts the efficacy of the intervention. Compliance can improve when software programs like Myopiacare,12 the BHVI (Brien Holden Vision Institute) myopia calculator,13 and Ocumetra14 are used to help visually explain the risks and goals of myopia management.

Figure 1. Clinical tests for myopia.
“Like many diseases, prevention is key. The sooner we identify the risk of myopia, the earlier we can begin management and treatment, and the better the patient’s visual outcome is likely to be”
Non-Modifiable Risks for Developing Myopia
Genetics: Genetic factors play a significant role in the development of myopia, with several syndromes such as Marfan syndrome, Stickler syndrome, and congenital night blindness being associated with high myopia.9 Myopia in children under the age of six is not very common, only 0.2% in Singapore,15 so further tests and tertiary referral may be warranted.
Parental Myopia: The risk of developing myopia increases two-fold if one parent is myopic and five-fold if both parents are myopic.16 This correlation is less likely genetic and more likely due to home lifestyle factors.17
Gender: Although there is no basic difference in myopia prevalence related to gender, more recent studies18 report higher rates of myopia in girls. This trend may be linked to social factors like educational demands, attitudes towards near work, and time spent outdoors.
Ethnicity: Ethnicity also influences myopia prevalence, with higher rates observed in East and Southeast Asia.1 Environmental exposures may mediate these differences, and Asian children tend to experience faster myopia progression compared to non-Asians.
Age of Onset: Age of onset is the key factor for expected progression,19 with faster progression observed in children who develop myopia younger than age 10.20 The risk of high myopia in adulthood is up to 50% for those with onset younger than age 10, compared to just 1% for those with onset greater than age 10. The rate of progression, which is non-linear, increases 1.00D by age seven, and decreases to 0.50D by age 11–12.20
Initial refractive assessment flowchart
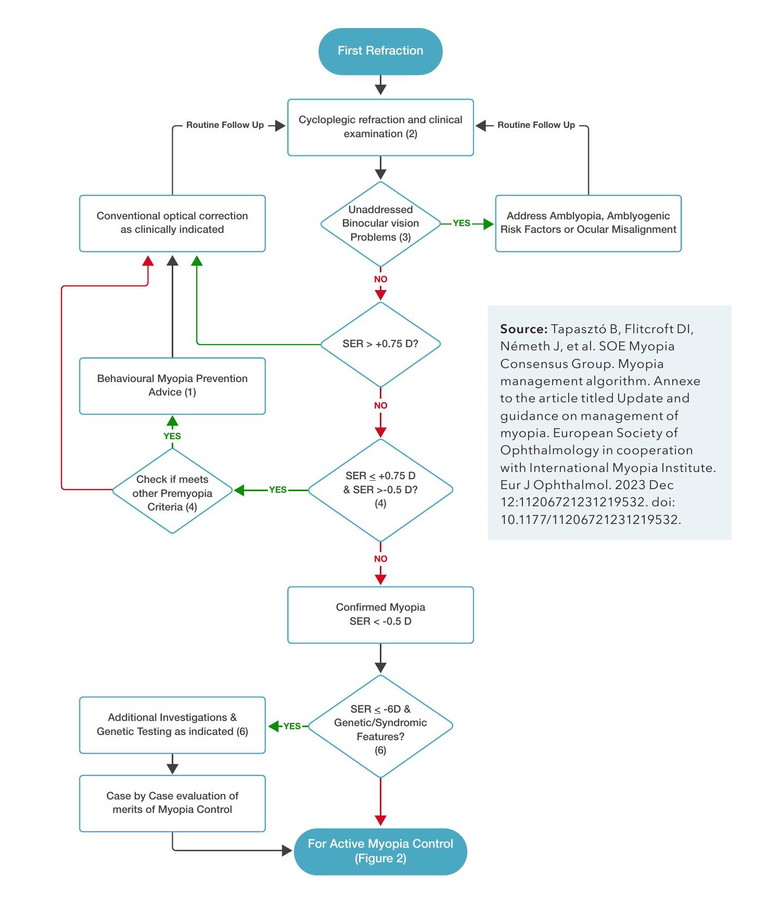
Figure 2. Initial refractive assessment flowchart.34 Algorithm for the primary and secondary prevention of myopia. Numbers refer to the states identified in the text. The flowchart needs to be read from top to bottom, however at some decision points, certain responses are going upward and eventually returning to an earlier level of the flowchart, showing the necessity for repeated cycles to monitor and follow-up on myopia development and intervention procedures. D: Diopter, SER: Spherical equivalent refraction.
Other Factors: Other factors also play a role, including being a first-born child, height, intelligence, physical activity, sleep, socioeconomic status, smoking, diet, urban versus rural living conditions, pollution, housing, and circadian rhythms. These multifactorial risks may be important when customising recommendations.21
Modifiable Risks for Pre-Myopes
Time Outdoors: For the pre-myope, longer outdoor time is associated with slower axial elongation. However, this effect does not appear to apply to existing myopes.22 Spending less than two hours per day outdoors increases risk.23 A 2024 study by Yang et al. found the risk of myopia was higher in overweight children with decreased outdoor time.24 Hypotheses for the myopia-protective effect of outdoor activity include reduced peripheral defocus, increased vitamin D synthesis, melatonin regulation, and dopamine upregulation.25 The clinical recommendation remains that the benefit of outdoor time should be discussed and not overlooked.
Spending 40–80 minutes outdoors daily is linked to reduced myopia incidence due to dopamine release, vitamin D, increased depth of field, and light exposure. Greater daily light exposure, specifically more than 3000 lux, is also associated with slower axial elongation.26
Reading: While the link between reading and myopia has been inconsistent, some studies have shown an increased risk. Continuous reading (either paper or computer) for more than 30 minutes increases myopia risk by 1.5x and closer reading distances (less than 30 cm) by 2.5x.27 The recommendation is to take regular breaks from near tasks and increase the working distance greater than 30 cm. The Harmon Distance,28 that is, the distance from your fist at your chin (or eye) to your elbow on the desk, is still a useful and practical visual recommendation for students.
Screen Time: Similarly, the link between digital devices and myopia is unclear, however more screen time generally means less outdoor time. General advice is against giving digital devices to infants, as screen time during age one was found to be predictive of children’s screen time from ages two to five.29 There is a four to eight times increased risk when playing games for more than two hours and studying for more than four hours.30 Contrast has been found to significantly influence retinal processing, with bright letters on a dark background showing to be protective against myopia.31
SCREENING FOR PRE-MYOPIA
Baseline Refractive Error
Refractive error is currently considered to be the strongest predictor of myopia onset. While it’s expected to see a high variability in childhood hyperopia, less hyperopia than +1.00D requires a closer look. Zadnik et al. found that hyperopia of +0.75D at the age of six, +0.50D at the age of seven to eight, +0.25D at the age of nine to 10, and plano at the age of 11, are highly likely to be myopic by age 13.32 Additionally, the younger the onset, the higher the risk of high myopia: a sevento eight-year-old at onset has a 50% risk, whereas a 12+ year old has a 5% risk of high myopia.33 The Initial Refractive Assessment Flowchart34 (Figure 2) is a useful clinical reference.
High Astigmatism
Children with mixed astigmatism (e.g. +1.00/2.00) showed minimal refractive changes until they convert to simple astigmatism (eg plano/-2.00) or compounded astigmatism (eg -1.00/-2.00).35 About 10% of pre-schoolers have astigmatism 36 and given that corneal curvature doesn’t change much during schoolage years,37 topography changes should raise red flags. Corneal steepening changes can be an indicator of corneal ectasia and there have been case studies of keratoconus onset as early as four years of age.38 This is a concern as paediatric keratoconus can have a prevalence of up to 5% in some countries. 39
Axial Length
Similar to using the percentiles of a growth chart when monitoring height in boys and girls, the ocular axial growth chart provides a benchmark to identify and monitor premyopes. The COMET trial found that a younger age at baseline was strongly associated with faster myopia progression and greater axial elongation.40 Axial length longer than 22.33 mm for fiveto six-year-old Asian children41 and longer than 23.2 mm for sixto seven-year-old European children42 are predictive of myopia onset less than 10 years of age.
The axial length growth chart can help predict those at risk of high myopia43 and thus requiring a more aggressive approach earlier rather than later. Biometry is not widely available and so, for practices without access, ocular axial length can be estimated with cycloplegic refractive error and average keratometry values.44
Peripheral Refraction
Peripheral refraction is potentially a risk factor for myopia onset and can be categorised as: low risk < +0.25D; intermediate risk +0.25 to +0.50D; and high risk > +0.50D.10 Lin et al.45 found a significant correlation between the superior retina’s myopic defocus and myopia progression, indicating relative myopic defocus in the superior retina can be an early predictor of central myopic shift in initially emmetropic children. This suggests that interventions aimed at maintaining emmetropic conditions in the superior retina may help prevent the onset of central myopia in children, and this is an area where further research will help guide clinical recommendations.
Binocular Vision Dysfunction
Mutti et al. published a number of papers on the link between binocular vision and myopia
“… patient engagement is the key to compliance, as it ultimately impacts the efficacy of the intervention”

“While significant effort is going into slowing progression of myopia… delaying onset by one year can potentially reduce myopia refraction by 0.75D or more”
onset. Children with myopia measured a higher accommodative lag up to four years before the onset of myopia.46 Binocular vision risk factors also included near esophoria,47 lower amplitude of accommodation and accommodative infacility,48 and higher AC/A ratio in both pre-myopes and progressing myopes.49
MANAGING THE PRE-MYOPE
There was a strong global focus at the International Myopia Conference (IMC), held in China in September 2024, on delaying (not just managing) the onset of myopia in children, particularly those identified as high risk.
Outdoor time: We know that outdoor light has protective benefits for myopia, especially in pre-myopes, and families should be encouraged to incorporate a lifestyle that takes them outdoors. Meta-analysis suggests outdoor time has similar efficacy to more costly myopia interventions to control myopia.50
Low dose atropine: Recent studies have shown that low-concentration atropine eye drops effectively delay the onset and progression of myopia in children. Yam et al. found that 0.05% atropine eye drops in pre-myopic children can reduce myopia incidence from 53.0% to 28.4% over two years.51 Even at a lower dose of 0.01%, atropine can reduce myopia incidence from 30.7% to 10.7.52 These studies support a much earlier retrospective study published in 2010 that showed 0.025% atropine delayed myopia onset.53 This is a simple intervention to consider for high-risk children.
Myopia control spectacles and contact lenses: Myopia control contact lenses (MCCL) would likely be a challenge to prescribe for a pre-myope without a perceived need for distance correction. Similarly, myopia control spectacle lenses (MCSL) may not have the required 12+ hours wear that is required to attain efficacy. However, for high-risk premyopes, wearing these lenses could create that protective peripheral myopic shield on the retina and delay the onset of myopia. At IMC 2024, Australian optometrist Dr Oliver Woo presented a 12-month retrospective study of 49 Asian children (aged five to eight years) from a clinical practice, and found a mean axial length change of 0.16 mm when they wore H.A.L.T. lenses (Essilor Stellest).54 In another study, 24 pre-myopic children (mean age five years) wearing photochromic DIMS (Defocus incorporated multiple segments, HOYA MiyoSmart) for six months progressed a mean of 0.10 mm over a six-month period.55 Future studies with control groups will shed more light.
For myopia control efficacy, peripheral defocus spectacle lenses are recommended to be worn for 12 hours a day. The necessary wearing schedule can be a challenge for younger children who have no visual acuity benefit in wearing spectacles. DIMS power range starts from plano, while H.A.L.T. lenses are available in low plus combined with minus cylinder. This means that although plano or low plus could be prescribed for the pre-myope, wearing compliance may be questionable.
Repeated Low-Level-Red Light (RLRL) therapy: While there are quite a few metaanalysis studies on RLRL efficacy in myopia progression, there are not many on pre-myopia. Two studies, a prospective study published in 2024,56 and a randomised control trial from 2023 conducted in 10 primary schools in China,57 found RLRL significantly reduced the incidence of myopia in pre-myopic children, both in terms of axial length and SER. While safety issues remain a concern, no visual acuity or structural damage was reported.
EMERGING MANAGEMENT OPTIONS FOR PRE-MYOPES
Modifying the environment: Using high spatial frequency classroom images (custommade wallpaper with forest and sky scenes) showed some protective benefits in myopia onset in Chinese classroom.58 Could this be a potential public health initiative one day?
Violet light, cyan light, blue light exposure: Will certain light wavelength exposure become a practical intervention one day? Violet light, which is available outdoors but not indoors, has been found to prevent myopia onset through the non-visual photoreceptor, OPN5. The use of violet-lightemitting frames (360–400 nm at 310 μW/cm²) in children has also been shown to provide some benefit (a change of 0.5D in 24 weeks) with further studies underway.59 Exposure to cyan light showed a reduction of axial length and choroid thickening, both in young children and adults.60 Interestingly, even wearing blue-tinted sunglasses also showed a reduction of 0.24 mm compared to the control group over a two-year period.61
CONCLUSION
Taking a proactive approach to halting the myopia tsunami begins by identifying those at risk of myopia and advising on strategies to manage modifiable risks. Early treatment, personalised to the patient’s needs, can slow progression and can greatly improve their long-term outcomes. While significant effort is going into slowing progression of myopia once they are myopic, delaying onset by one year can potentially reduce myopia refraction by 0.75D or more.62
Regular reviews, consistent monitoring of treatment effectiveness, and knowing when to refer patients to tertiary care are all important steps. Staying up to date with emerging treatments ensures that families are educated on the latest interventions. By considering clinical data and individual risk factors, optometrists can offer detailed evaluations and targeted treatment plans.
To earn your CPD hours from this article, visit mieducation.com/halting-the-myopia-tsunami-why-starting-early-matters.
References available at mieducation.com.

SooJin Nam MOptom BOptom MBA (exec) is a part-owner of five Eyecare Plus optometry practices in Sydney and has a strong interest in three main areas: binocular vision dysfunctions, myopia control, and orthokeratology. She was previously a director for both Optometry NSW/ ACT and Eyecare Plus and is a current director of the Australian Optometric Panel. She is a regular contributor to the optometry industry as a key opinion leader.