mieducation
Anterior Segment Reconstruction: Techniques and Tips for Optimum Outcomes
Most anterior segment reconstruction occurs following ocular trauma. Trauma is one of the most devastating causes of vision loss in both the developed and the developing world and leads to severe visual impairment if it is not properly managed.1 The impact of ocular trauma is not limited to loss of sight. Many cases can also lead to major cosmetic problems with the resultant significant psychological burden.
WRITERS Dr June Artaechevarria-Artieda and Dr Alex Hamilton
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Realise the different types of ocular trauma that can present in practice,
2. Be aware of the different approaches to ocular trauma repair that may be necessary,
3. Understand the need for prompt action to optimise visual outcomes, and
4. Understand optometrists’ role in long-term management of these patients.
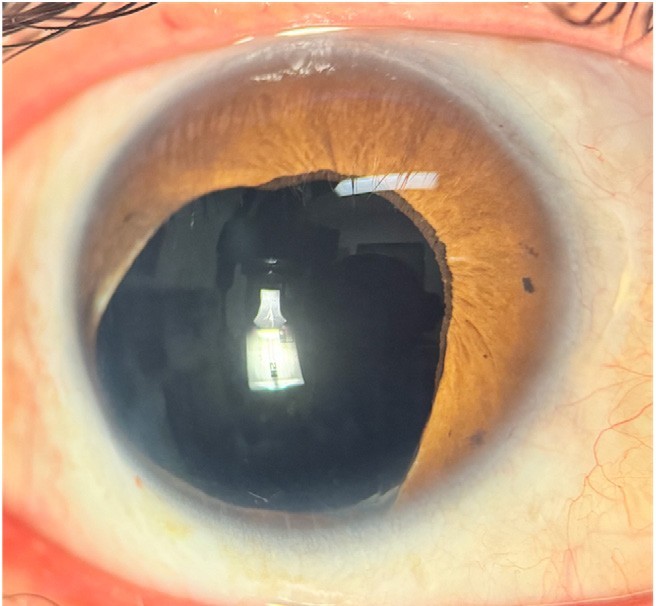
Figure 1. Patient with partial aniridia and aphakia, after battery explosion.
Data from the World Health Organization Programme for the Prevention of Blindness suggests that 55 million eye injuries occur globally each year, including 200,000 open-globe injuries. There are approximately 1.6 million people who are blind from eye injuries and 2.3 million people with bilateral low vision from trauma. Almost 19 million people globally have unilateral blindness or low vision from trauma.2
Due to the external mechanism of both blunt and penetrating trauma, the structures that are most frequently affected are those that are most anterior: the cornea, the iris, and the lens (Figure 1). Effective acute and longterm management of the damaged structures is essential for optimising the visual and cosmetic outcomes for the patient.
ACUTE TRAUMA MANAGEMENT
A thorough assessment of an acutely injured patient is crucial for preserving vision. Patients must be provided with appropriate analgesia and a complete anterior, and posterior segment examination should be performed. The globe must be protected from additional harm. In cases where patients have penetrating eye injuries with an open globe and experience nausea or vomiting, the administration of antiemetics is necessary to prevent the potential extrusion of intraocular contents. Furthermore, the early initiation of systemic antibiotic therapy is important to decrease the risk of endophthalmitis.
In general, open globe injuries should be repaired within 12 to 24 hours of the injury to improve visual outcomes and lower the rate of infectious endophthalmitis.3
Corneal Lacerations
The cornea is the most likely structure to be injured in trauma cases, as it is the most anterior part of the eye. Corneal lacerations can vary in size, shape, and depth. These lacerations can be linear, such as might occur from a sharp blade, through to more complex stellate patterns, such as might occur from injury with a nail. Corneal lacerations can be partial or full thickness. Every corneal injury is different, and management needs to be individualised in each case.4
Most corneal lacerations will require primary surgical repair, which should be performed as soon as possible. The aim is to create a watertight wound closure, restore the tectonic integrity of the globe, and minimise the amount of post-operative corneal scarring and astigmatism.
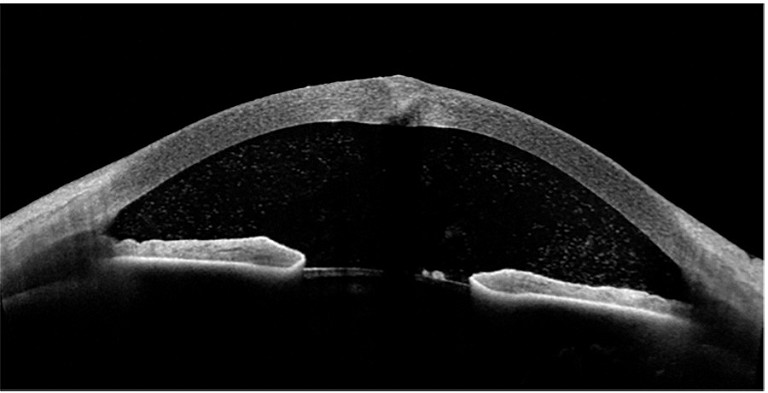
Figure 2. AS-OCT image showing a full-thickness central corneal laceration.
Shallow, partial thickness lacerations can sometimes be managed conservatively with a bandage contact lens. In all cases, the presence of aqueous leak needs to be thoroughly assessed with a Seidel test using fluorescein dye. If present, surgical repair is generally required.
Occasionally, the depth of the laceration is difficult to assess clinically. In these cases, anterior segment optical coherence tomography (AS-OCT) can be used to help determine the depth of the corneal laceration (Figure 2).
When the laceration is limited to the cornea, surgical repair using interrupted 10/0 nylon sutures is the most common approach. If the laceration extends to the limbus, or beyond the limbus to the sclera, stronger sutures such as 8/0 or 9/0 nylon are preferred.5
Tissue adhesives, such as cyanoacrylate glue, are also effective in sealing corneal perforations. They can be used alone in small perforations or in addition to sutures if any residual leak is noted (Figure 3).6
In all cases, topical and systemic antibiotic therapy is used to minimise the risk of keratitis and endophthalmitis.
Hyphaema
Hyphaema is the accumulation of blood in the anterior chamber (AC). It can range from microscopic blood cells floating in the AC (microhyphaema) through to complete filling of the AC with blood (the so-called eight ball hyphaema). Hyphaemas can occur secondary to both penetrating and blunt trauma.
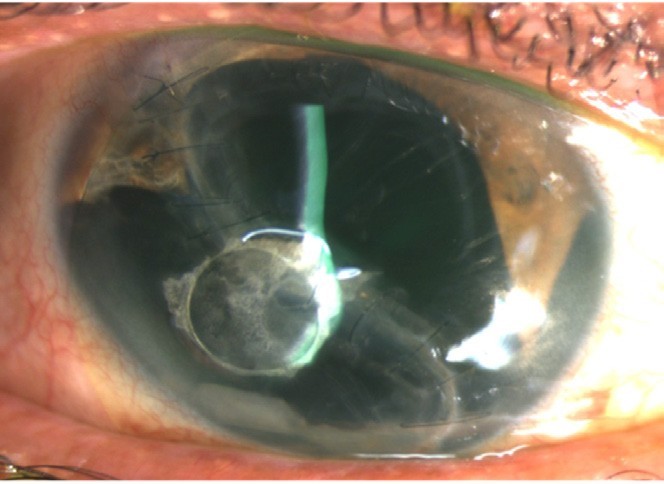
Figure 3. Large post-traumatic corneal laceration that has undergone primary closure with 10/0 nylon sutures and then required cyanoacrylate glue.
Uncomplicated hyphaemas are managed conservatively. Maintaining the head elevated to 45 degrees allows the blood to settle inferiorly and to clear the visual axis. Topical steroids are added to reduce the associated inflammation and topical cycloplegic agents are used to reduce the ciliary spasm and formation of posterior synechiae. The benefit of using antifibrinolytic agents, such as epsilon‐aminocaproic acid and tranexamic acid, is unclear.7
In the case of large hyphaemas, uncontrolled elevated intraocular pressure (IOP), or active bleeding, surgical intervention may be required and consists of anterior chamber irrigation and aspiration (AC washout). If left untreated, the blood can stain the cornea, causing irreversible corneal opacification due to haemosiderin becoming embedded within the corneal stroma (Figure 4).
Patients should be monitored closely for the first three to seven days, as during this period there is a significant risk of re-bleeding. Rebleeds may be more severe than the initial bleed and more likely to cause complications such as glaucoma, corneal blood staining, and formation of posterior synechiae.8
Lens Rupture
In the case of eye trauma, the crystalline lens can also be injured, and cataract formation often occurs. Cataract extraction may be performed immediately following penetrating eye injury as a ‘primary’ procedure, or deferred for weeks or months after the trauma and performed as a ‘secondary’ procedure.
If the lens capsule is ruptured in a penetrating eye injury, lens material can be released into the anterior chamber. The lens proteins can impair the aqueous outflow, either directly obstructing the trabecular meshwork (known as lens-particle glaucoma) or creating an inflammatory reaction in the AC (phacoantigenic glaucoma).9
Removal of the lens may occasionally need to be performed urgently if there is capsule rupture with active lens material leak, phacoantigenic glaucoma, or any other conditions that increase the risk of developing inflammation and elevated IOP. However, early lens removal can be challenging. The other associated injuries often lead to poor visualisation of the lens, in particular due to corneal oedema and difficulty maintaining AC stability due to leaking corneal wounds.
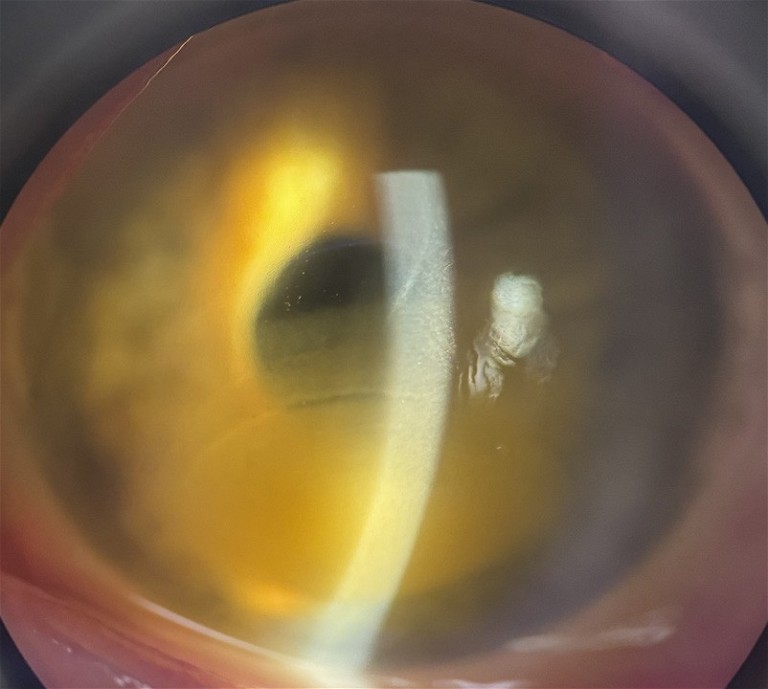
Figure 4. Corneal blood staining.
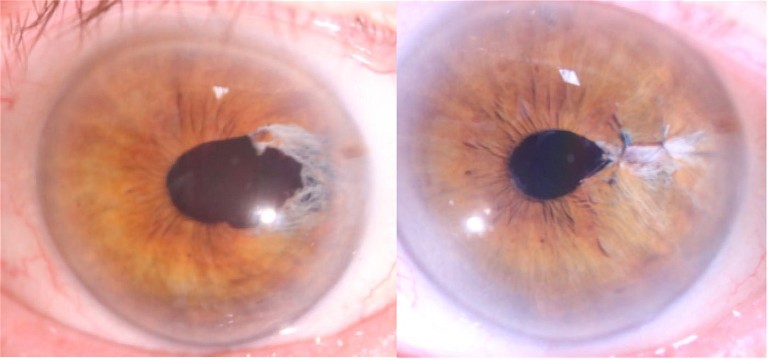
Figure 5. Postsurgical iris defect managed with iris suturing.

Figure 6. New iris suturing technique with modification of the Siepser sliding suture.18
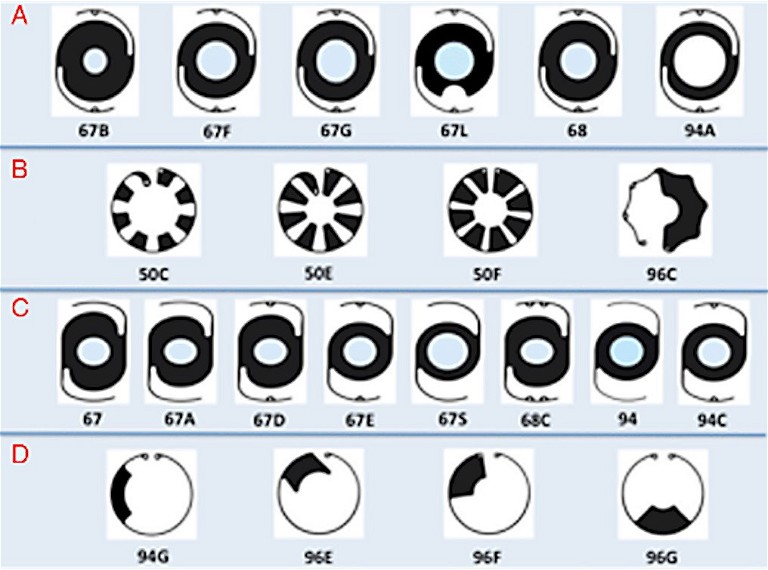
Figure 7. Currently available model of aniridia implants from Morcher GMBH (Suttgart, Germany).
Where possible, it is preferable to delay lens-based surgery and address a traumatic cataract at a later stage. By performing cataract surgery as a ‘secondary’ procedure, the surgery can be carefully planned. The eye is less inflamed, the cornea is tectonically stronger, and biometry can be more accurately performed, all of which leads to an improved visual outcome for the patient.
In blunt trauma, the lens can be partially or completely dislocated. If it becomes anteriorly displaced, it can block the angle and cause acute glaucoma. Rarely the lens can remain in position but can swell, such that the anteroposterior diameter increases and occludes the angle (phacomorphic glaucoma). In these cases, an urgent cataract extraction may be required.9
SURGICAL RECONSTRUCTION TECHNIQUES
After the acute trauma has been managed and the eye has been stabilised, the degree of iris damage and post-traumatic cataract needs to be assessed and managed. Each case will be different, and the appropriate management needs to be tailored to the individual.
Iris Repair
The iris is the structure responsible for maintaining the size and diameter of the pupil. It also helps achieve good quality of vision by reducing the optical aberrations from the cornea and the lens, limiting the amount of light entering the pupil, preventing excessive glare, and enhancing the depth of focus. Patients with traumatic injuries to the iris usually complain about glare, photophobia, decreased contrast sensitivity, and poor cosmesis.10 Depending on the size of the defect, different surgical techniques may be required: small residual iris defects can be managed with suturing techniques, whereas large iris defects, with or without lens injuries, can be managed using prosthetic iris devices.
Iris Sutures
Localised iris defects can be repaired by performing a pupilloplasty, in which the iris margins are brought together and sutures placed through the iris stroma (Figure 5).
Many different suturing techniques have been described, and the appropriate technique to use depends on the nature and location of the defect (pupil margin, central iris, iris root).10 Iris root disinsertions (iridodialysis) usually require suture placement to tether the iris root to the scleral wall.11
The principle of suturing iris defects is to tie the knot outside the eye and slide the knot into the appropriate position inside the eye. The technique broadly consists of passing a long single-armed prolene suture through both ends of the pupillary defect. The distal thread is then pulled back with a Sinskey hook, placing the loop outside the eye. A double sliding knot is performed, and both ends of the sutures are pulled. As such, the knot is introduced into the eye and can be tightened. Then the process is repeated again to lock the first suture in place.
Some of the techniques described include the Siepser sliding knot, the single-pass four-throw technique, and the McCannel suture (Figure 6).
Prosthetic Iris Devices
Iris-Lens Diaphragms
Iris lens diaphragm implants consist of a central clear optic surrounded by a black ring that simulates the natural iris. The most common models available are the Morcher lenses. There are numerous models with different pupil apertures for use in either the capsular bag or fixated to the sclera (Figure 7A, 7C).
The main advantage of this type of prosthesis is the ability to correct both the aniridia and aphakia with a single implant, without the need for an extra intraocular lens (IOL). However, these devices are large and require large corneal incisions (between 150–180°) for their implantation.12 These prostheses are also black, meaning patients, particularly those with light coloured irises, can have suboptimal cosmetic outcomes with significant iris heterochromia post operatively.
Endocapsular Capsular Tension Rings
These devices consist of a capsular tension ring (CTR) with segmental iris diaphragm. There are many different models, and they can be used alone or in combination to cover a larger area of iris defect (Figure 7B, 7D).
The main benefit of using the CTR-based segments is the smaller corneal incision that is required for their implantation, reducing the risk of intra and postoperative complications. However, an intact capsular bag is required for the placement of these implants.12
Artificial Iris
Artificial irises are individually customised iris implants designed to be colour matched to the fellow eye. The HumanOptics CustomFlex artificial iris is custom made based on a photograph of the healthy iris of the fellow eye (Figure 8).13
It is composed of a flexible biocompatible silicone elastomer, which enables the insertion of the device through a very small corneal incision of between 2.5–3.5 mm.
These implants are versatile. They can be placed in the capsular bag in front of an IOL or sutured to the sclera in cases where there is inadequate capsular support.
One benefit of this type of artificial iris is that it is foldable and can be easily introduced into the eye through a small incision. The customisation of the iris also results in good cosmetic outcomes for patients. Furthermore, this artificial iris can be implanted with a wide range of IOL models.12
Another artificial iris that is available in Australia is the Reper artificial iris, which is a combined IOL and artificial iris in a single implant. The advantages include a single device insertion, the small incision needed, and the good cosmetic outcomes that are achieved due to the many different iris colours available.14
Secondary Lens Repair
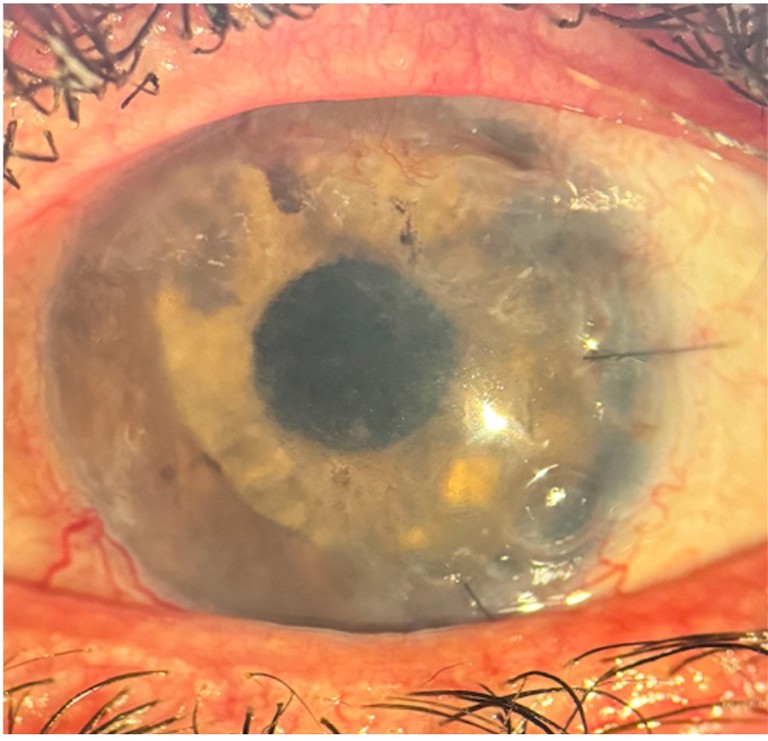
Figure 8. HumanOptics CustomFlex artificial iris and IOL implant on the first day after surgery.
In many trauma cases, a traumatic cataract will develop rapidly. When possible, delayed repair is preferred. The timing needs to be tailored to the patient, often occurring weeks or months after the original injury.15 There is no consensus as to the best timing for this procedure.16

Figure 9. A step-by-step anterior segment reconstruction including: A) corneal laceration with sutures and cataract formation, B) worsening cataract and sutures removed, C) post-op after cataract surgery, and combined IOL-artificial iris complex implant. D) Binocular photo showing the good cosmetic result after the reconstruction.
“Patients with traumatic injuries to the iris usually complain about glare, photophobia, decreased contrast sensitivity, and poor cosmesis”
There are numerous benefits to delaying cataract surgery in these cases. If there are corneal sutures, ideally these should be removed at least one month prior to performing biometry. Improving the accuracy of the biometry and the lens calculation leads to better refractive outcomes. In the early period after trauma, the cornea will often be quite hazy due to inflammation. Over time the injured cornea will often clear significantly, improving visualisation during surgery and thereby reducing the risk of surgical complications. Insertion of an IOL should be performed where possible (Figure 9).17
LONG-TERM MANAGEMENT
All patients require long-term management after eye trauma and anterior segment reconstruction. This requires input from both the ophthalmologist and the optometrist.
Long-term complications can impact any part of the eye. After significant corneal injury, the cornea changes can limit visual acuity. Corneal scarring across the visual axis, irregular astigmatism, and corneal decompensation due to endothelial damage can all occur. In such cases, a partial or fullthickness corneal transplant may be required.
The posterior segment must also always be examined. In trauma, there is a risk of vitreous haemorrhage, retinal tear, and retinal detachment. Posterior segment issues can occur early and as late complications of trauma.
Glaucoma is a common long-term problem after trauma and occurs through multiple mechanisms. It is essential to monitor IOP and regularly assess the optic nerve to determine appropriate management.
Optometrists play a key role in monitoring this over time.
Optometrists also play an important role managing the optical correction of residual refractive errors. These are generally complex, as the astigmatism produced after corneal injury is often irregular and higher order aberrations are usually present. When glasses or soft contact lenses are not able to correct the optic aberrations, rigid gas permeable or scleral contact lenses may be needed.
CONCLUSION
Anterior segment reconstruction is challenging as every case is different, and the repair must be individualised to each patient. A step-bystep approach is recommended to guarantee the best long-term visual outcomes. Thanks to the development of new intraocular devices, we can now hope to achieve both improved visual acuity and very good cosmetic outcomes for patients. Optometrists play a key role in monitoring for potential long-term complications and helping to provide patients with the best long-term quality of life.
To earn your CPD hours from this article visit: mieducation.com/anterior-segment-reconstruction-techniques-and-tips-for-optimum-outcomes.
References
1. Patel, A.S., Al-Aswad, L., Justin, G.A. et al., Ocular trauma: acute evaluation, cataract, glaucoma. EyeWiki, American Academy of Ophthalmology (web page). Updated April 2023, available at: eyewiki.aao.org/Ocular_Trauma:_Acute_
Evaluation,_Cataract,_Glaucoma [updated April 2023, accessed March 2024].
2. Négrel, A.D., Thylefors, B., The global impact of eye injuries. Ophthalmic Epidemiol. 1998 Jan 1;5(3):143–69.
3. Zhou, Y., DiSclafani, M., Jeang, L., Shah, A.A., Open globe injuries: Review of evaluation, management, and surgical pearls. Clin Ophthalmol Auckl NZ. 2022;16:2545.
4. Legault, G.L., Kumar, B., Corneal laceration repair [Updated July 2023]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available at: ncbi.nlm.nih.gov/books/NBK576444/.
5. Rashad, R., Hussain, A., Ament, C., Surgical principles for management of corneal lacerations, EyeNet magazine, 2023 June; available at: aao.org/eyenet/article/principlesfor-management-of-corneal-lacerations [accessed March 2024].
6. Sharma, A., Kaur, R., Patnaik, B., et al., Fibrin glue versus N-butyl-2-cyanoacrylate in corneal perforations. Ophthalmology. 2003 Feb;110(2):291–8.
7. Gharaibeh, A., Savage, H.I., Lindsley, K., ey al., Medical interventions for traumatic hyphema. Cochrane Database Syst Rev. 2019 Jan 14;2019(1):CD005431.
8. American Academy of Ophthalmology, 2020–2021 BCSC Basic and Clinical Science Course, Ch 14: Clinical aspects of toxic and traumatic injuries of the anterior segment (web page), available at: aao.org/education/bcscsnippetdetail.aspx?id=31b9e6a0-5abe-4f7c-b457-ceafadddab3d [accessed March 2024].
9. Zamora-de la Cruz, D., Garzón, M., Arrieta-Camacho, J., Management of traumatic cataract, EyeNet Magazine. 2016 Aug; available at: aao.org/eyenet/article/management-oftraumatic-cataract [accessed March 2024].
10. Gurnani, B., Kaur, K., Traumatic iris reconstruction. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024, Available at: ncbi.nlm.nih.gov/books/ NBK578200 [accessed March 2024].
11. Shekhar, M., Prasad, R.S., Anusha, A. Iridodialysis repairA simplified approach. Indian J Ophthalmol. 2022 Mar;70(3):1073.
12. Srinivasan, S., Ting, D.S.J., Koch, H.R., Prosthetic iris devices. Can J Ophthalmol. 2014 Feb;49(1):6–17.
13. Mayer, C.S., Hoffmann, A.M., Khoramnia, R., Functional outcomes after combined iris and intraocular lens implantation in various iris and lens defects. BMC Ophthalmol. 2020 Sep 15;20(1):370.
14. Frisina, R., De Biasi, C.S., Gambato, C., et al. Reper intraocular lens with artificial iris: implantation techniques and outcomes. Eur J Ophthalmol. 2021 May;31(3):1469–74.
15. DelMonte, D.W., Murchison. A., Rizzuti, A., et al., Traumatic cataract surgery, EyeWiki, American Academy of Ophthalmology (web page, updated April 2024), available at: eyewiki.aao.org/Traumatic_Cataract_Surgery [accessed April 2024].
16. Tabatabaei, S.A., Rajabi, M.B., Yaseri, M.. Early versus late traumatic cataract surgery and intraocular lens implantation. Eye Lond Engl. 2017 Aug;31(8):1199–204.
17. Agarwal, A., Kumar, D.A., Nair, V.m Cataract surgery in the setting of trauma. Curr Opin Ophthalmol. 2010 Jan;21(1):65–70.
18. Schoenberg, E.D., Price, F.W. Jr., Modification of Siepser sliding suture technique for iris repair and endothelial keratoplasty. J Cataract Refract Surg. 2014 May;40(5):705-8.

June Artaechevarria-Artieda MD FEBO is currently completing the Mabs Melville Cornea fellow at Sydney Eye Hospital. Prior to completing her ophthalmology training in Madrid (Spain), she finished her medical degree at the University of Basque Country (Spain) and completed her internship in Cologne (Germany). Dr ArtaechevarriaArtieda has a special interest in corneal transplants, as well as in anterior segment reconstruction. She has presented at several international congresses.

Dr Alex Hamilton BMed MPHTM (Dist) FRANZCO is a Sydney based ophthalmologist specialising in cataract, corneal and refractive surgery. For two years he undertook subspecialty training at Manchester Royal Eye Hospital and Moorfields Eye Hospital in London. He now works at Sydney Eye Hospital where he trains registrars and international fellows, and is in private practice in Sydney.