mieducation
Corridor Conundrums Optimising Progressive Addition Lenses
In her roles as Training Manager and then Professional Services Manager at Rodenstock, Nicola Peaper was often asked about corridor lengths in progressive addition lenses (PALs) and the impact they have on intermediate and reading areas, along with the problems that patients encounter.
In this article, Ms Peaper examines how corridor performance is affected by lens design and compensation. Additionally, she discusses considerations when choosing a corridor length and the implications of fitting decisions.
WRITER Nicola Peaper
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Minkwitz astigmatism and corridor length affects the width of a corridor,
2. Different methods of insetting a corridor affects the usable width available to a patient, and
3. Giving preference to visual tasks at distance, intermediate and near working distances affects the positioning of aberration on a lens.
It used to be that choosing a corridor length was easy. When PALs first came to market, they were all long corridor, most about 22 mm, and patients adapted or, more likely, practitioners adapted their fitting methods to allow for successful use.
Then came the shallow frames of the 1990s and short corridors became the norm. The only problem was that the corridor needed to be short enough to give a reasonable near area. However, at the turn of the century, digital surfacing meant corridors were no longer fixed in length by being moulded on to the front surface of the lens. The new free form lenses could have corridors of any length, between maximum and minimum limits, and be measured to 0.1 mm. The minimum limit is set by the amount of Minkwitz aberration produced and the maximum limit set by posture. At the same time, frames started to become deeper again, and at that point the whole process of choosing a corridor length became more complex.
MANAGING ABERRATIONS
PALs, like any other lens, are subject to general aberrations such as oblique astigmatism, spherical aberration, and distortion. On top of this there is the added aberration of Minkwitz astigmatism, unwanted cylinder power that sits either side of the corridor. The Minkwitz theorem states that, perpendicular to the vertex line, the surface astigmatism changes twice as quickly as the rate of change of power along the vertex line.1 In other words, as the power of a lens increases by 1.00D vertically,
2.00D of unwanted cyl is produced horizontally. This aberration cannot be eliminated but can be controlled from a positioning point of view by design.
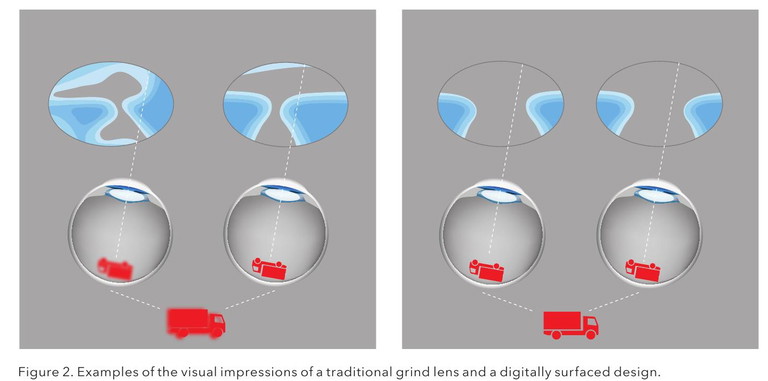
In the last century, when lenses were produced with traditional grind techniques, the general aberrations could add into the Minkwitz astigmatism to reduce the width of usable vision over all portions of the lens. (Figure 1A). This tended to mean that practitioners were wary to use PALs with patients with high distance scripts.
However, with the introduction of digital surfacing at the turn of the century, along with compensations for base curve and position of wear, these general aberrations were much reduced (Figure 1B), resulting in a consistent aberration pattern dictated by the add power rather than the distance script. This means that if a patient notices a reduced clear area for distance vision with a modern, compensated design, it is unlikely to be related to the distance script.
Much of the research and development going into lens design now is about controlling Minkwitz astigmatism with the aim to give the patient the maximum use of the full possible width of the corridor and to reduce the experience of swim caused by unwanted cyl power in the periphery.

A

B
Figure 1. Lenses showing A) base curve effect and B) reduced base curve effect.
For the former, the aim is to make the corridor as symmetrical as possible and to ensure the pupil follows the centre of the corridor. To achieve minimum exposure to unwanted cyl power, the aberration can be moved around the lens, removing it from the most used portions of the lens. This can be dictated by both lifestyle and physiological aspects.
To ensure that the pupil follows the centre of the corridor, the method of calculating the inset on a lens is important. Initial lens designs had a standard inset. This is illustrated on most lens marking up charts with a near reference circle 2.5 mm inset from the fitting cross. There are two problems with this.
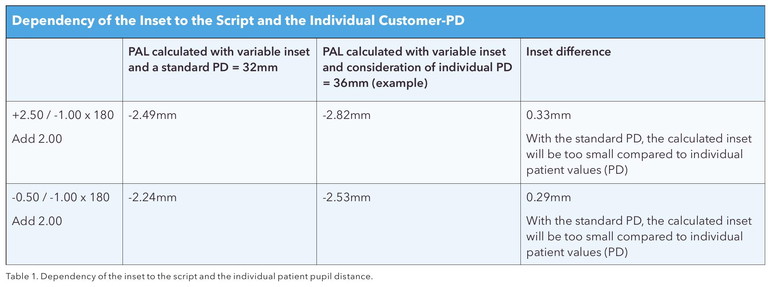
Firstly, a standard inset does not consider the eye experiencing prism as it converges. A myope will experience base in prism and a hyperope base out. This will influence the amount that a person converges, and the corridor needs to be arranged accordingly. The term for this is variable inset i.e., the inset varies due to the distance script and also the reading distance dictated by the addition. The second problem is that the individual pupillary distance (PD) needs to be considered. If variable inset alone is used with an average PD of 64 mm, then a patient with a PD of 72 will converge too much for the inset provided and may find near blur. Conversely, a patient with a PD of 55 will not converge enough and will experience narrowing of the corridor temporally. Table 1 shows the difference both variable inset and PD optimisation can make. This, of course, makes checking the near power on a PAL difficult as the inset is not known unless recorded on the lens packet. For some lens designs it is possible for the practitioner to order a specific inset. This is useful with patients that may not converge normally, such as a congenital monocular patient where an inset of zero would probably be appropriate.
LENGTH VS WIDTH
Corridor length plays a large part in the available corridor width. The shorter the corridor, the faster the rate that power increases. Sheedy et al.1 produced a graph of predicted corridor widths as a function of power rate in the middle of a corridor. Looking at this for an add of +2.00D increasing at a rate of 0.14D/mm (a 14 mm corridor), the zone width in the centre of the intermediate area, as predicted by Minkwitz theorem, is 1.9 mm wide. If the rate reduces to 0.11D/mm (18 mm corridor) the width increases to 2.3 mm (width is defined as the point at which 0.25D of unwanted cyl power is present). For a 1.00D add, the widths would be 3.5 mm and 5.0 mm for the same corridor lengths. Obviously, most patients will tolerate 0.25D or 0.50D of unwanted cyl power. As such, the usable corridor is wider than these figures. However, this illustrates the fact that it is beneficial to provide the longest corridor that a patient can comfortably wear to give the maximum width and reduce head movements during intermediate and close work.
One aspect of lens design that allows for maximum use of corridor, when we consider the rate at which unwanted cyl comes in, is power optimisation in both right and left scripts. If the peripheral aberrations don’t match, differing amounts of cylinder power will be experienced as the eye moves from the centre of the corridor, and stereopsis will not occur. If the aberration is similar, then clear vision will be achieved further into the periphery of the lens. Again, this technology is enabled by digital design and surfacing (Figure 2).
While corridor length selection was dictated by shallow frame choice in the past, now with deeper frames, the choice is wider. However, the depth of the frame does not dictate the length of corridor chosen. If the frame has a depth that will allow for an 18 mm corridor, it does not mean that length is ideal. If a patient has always had a short corridor, it does not mean that they should repeatedly have the same corridor length.
The deciding factor for a corridor length should be dictated by the patient’s comfortable – and to some extent habitual – head and eye posture in a ‘normal’ reading position. Reading tasks involve a combination of dropping the eye and lowering the chin and this varies depending on the task. A comfortable vertical lowering of the eyes for pre-presbyopic patients can be considered to be around 25°.3,4 Head position then takes up the remainder of the gaze lowering and can vary significantly from reading in a chair to reading text on a desk.
These ‘habitual postures’ can, and indeed are, changed in PAL use as the patient is shown that reading tasks now require different head and eye positions. The question then is: Can a patient that has become accustomed to one corridor length, and indeed lens design, adapt to change? A 2007 study5 took 10 presbyopic subjects and put half in a short corridor design PAL and the remainder in a long corridor. They wore the lenses for a month, had a week without, and then changed designs. Over the course of adaptation, the participants used more head movements, especially for near work, as was to be expected. Seven of the 10 participants preferred the second lens worn. Although the lenses were worn over a comparatively short period of time, this showed that patients can adapt to new designs and corridor lengths.
One important consideration, if we are attempting to replicate a patient’s experience with a previous corridor length, is how do we measure it?
Do we give it a numerical value that measures from fitting cross to an arbitrary point for near vision? At this point it is worth mentioning that not all manufacturers measure to the same near point. Some measure to the top of the near reference circle and some to the middle. So, considering a near reference circle diameter of 6 mm, one manufacturer’s 11 mm corridor can be another’s 14 mm corridor.
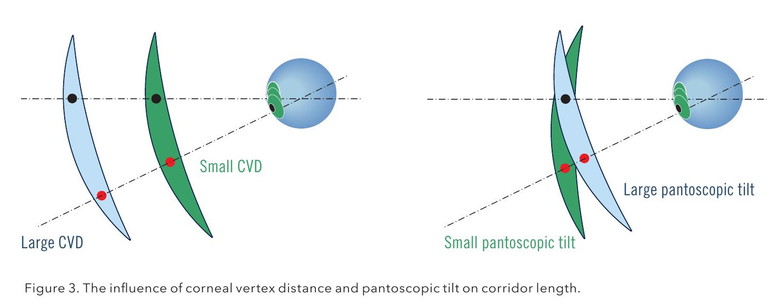
Should we instead consider how much the patient must lower their gaze, both head and eye? If we consider Figure 3 and try to maintain the patient’s habitual posture, the greater the corneal vertex distance (CVD) or the lower the pantoscopic tilt (PT), the longer the corridor necessary. This explains why, when dispensing two different frames with identical lenses fitted in the same way, a patient invariably prefers the comfort of one pair over the other.
One way to avoid this problem is to use a lens that has corridor length as part of its design. If dispensed as a position of wear version, the corridor will be different in every pair, but the patient’s experience will be consistent. If this solution is unavailable, then in a frame with a larger CVD or lesser PT, choose a slightly longer corridor.
Measuring Individual Zones
When measuring the individual zones on several different lens designs, Sheedy2 found that there were correlations between zone widths. Larger distance zone widths and areas were generally associated with narrower intermediate widths and areas and vice versa. The wider the zones for intermediate, the smaller the zone for near and vice versa. He stated, “Not surprisingly, all of the interzone relations are negative; that is, making one viewing zone wider or larger tends to result in the other two becoming narrower and smaller. By far, the strongest negative relation is between the intermediate and near zones… The Minkwitz theorem appears to predict the average zone width/power rate relationship over the length of the corridor. Individual lenses can be designed to exceed the predicted zone width in some areas, but as a result must have compensatory areas with less-thanpredicted width.”
Indeed, to make progressive addition lenses more comfortable in daily life, manufacturers have developed various lens designs that promise to suit the needs of the wearer. The designs can differ from each other in parameters, such as position and size of the viewing zones, the refractive power gradient (where the add power starts to come in and the speed at which it changes), and the distribution of unwanted astigmatism (the degree of softness or hardness of the design).6 The softer the design i.e. the slower the unwanted astigmatism comes in, the more suitable it is for dynamic tasks as the effect of swim is reduced.
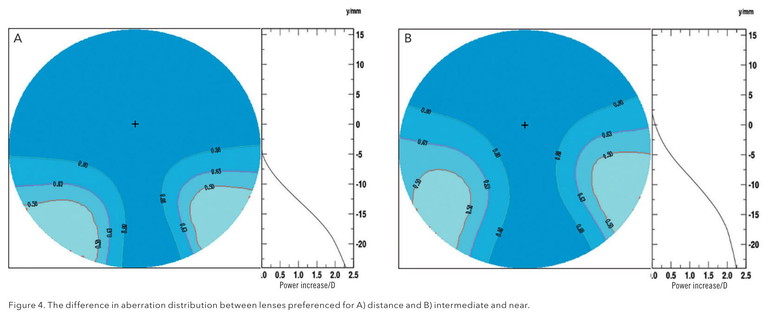
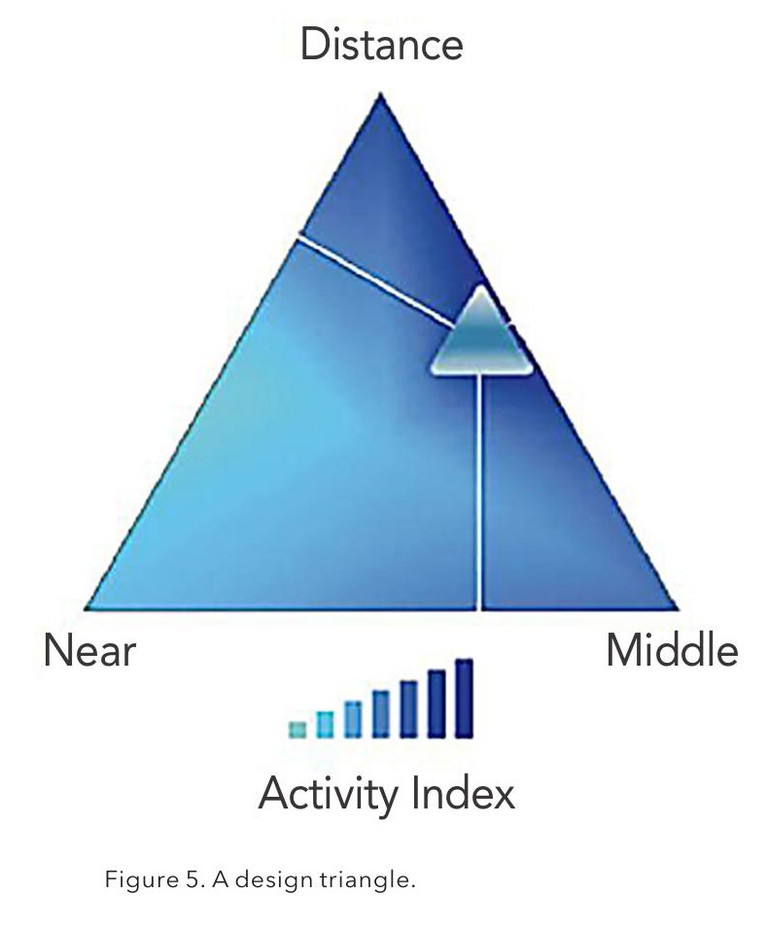
For each design, levels of preference can be given to each visual task; distance, intermediate, and near; and set designs in ‘suites’ of lenses can be produced for set lifestyles. For instance, a person who drives for a living would need preferences in the order of distance for clarity out to the periphery of the lens; intermediate for viewing dashboard, navigation aids, and side mirrors; and a fairly low degree of preference for near. This will produce a lens with the aberration pattern shown in Figure 4A. Conversely, a patient who drives a short distance to work and then uses laptops, tablets, and the occasional desktop, would need a lens with preferences in the order of intermediate and near for digital devices, with a lower preference for the reduced amount of distance use. This would produce an aberration pattern shown in Figure 4B.
There are an infinite number of design preferences that can be given to a lens for distance, intermediate, and near; and weighting can be decided by putting those three options in a triangle (Figure 5). Every point inside the triangle will give a different preference to a visual task. The design preferences in Figure 5 would produce a design like that in Figure 4a. In practice, most manufacturers give a choice of three to five designs to cover all lifestyles.
The influence of both corridor length and the starting point of the corridor can also be seen from the graphs showing power increase in Figures 4A and 4B. On the distance preferenced lens (4A), the add starts at 5 mm below the fitting cross. This lens will give rim to rim clarity at the fitting cross and will allow for the pupil to dilate for driving at night, without the add impinging on acuity. It also means the power gradient is steep, bringing the add in quickly for the patient to still maintain a reasonable downward gaze to read. Eighty-five per cent of the full add power is present at about 18 mm below the fitting cross.
On the intermediate and near preferenced lens, the add starts 2 mm above the fitting cross, meaning the power gradient is lower, giving a wider corridor. It also means that about 85% of the add is present at 15 mm below the fitting cross. If a patient has been wearing a short corridor standard lens design previously, then this design would give them a similar power experience but with a wider corridor than they had previously experienced.
ACCURACY OF FITTING AND FITTING HABITS
When progressive lenses were first introduced to market, they tended to have long corridors of up to 22 mm and so reading areas could be hard to access. Because of this, various fitting practices arose. In Germany, it was common to change the distance prescription by -0.25D and increase the add by +0.25D.7 In the United Kingdom, it was common practice to fit the lens 1–2 mm high. Even though lens corridors have become shorter and are ergonomically designed for a comfortable head and eye position, I still walk into practices and am told ‘we fit our lenses high to ensure the reading comes in quickly’ or ‘we fit our lenses low to reduce the effects of swim’.
As previously discussed, these effects can be gained now with different lens designs and if fitted correctly, these ‘lifestyle type’ lenses will address how quickly the add comes in or where the aberration appears on a lens to reduce swim while giving the patient access to the full corridor width.
If old fitting techniques are still used, the risk is that the patient will not have the ideal lens experience. With traditional PAL designs, if lens markings were not still visible, the distance script could be fairly confidently measured at the top of the lens and the full near script found at the bottom of the lens. This is not the case now. Wavefront calculations and digital surfacing means aberrations can be minimised at every vision point on the lens. What this means is that the power that can be measured on a digitally surfaced lens changes every 0.5 mm or so as the compensations change. Consequently, if the lens is fitted 2 mm above or below the pupil, the patient will experience the incorrect power.
A second problem with fitting the lens incorrectly is that the patient will access the corridor in the incorrect place and will therefore not follow the centre, resulting in asymmetry and apparent reduced corridor width. Inherent in a lens design is the positioning of the corridor so that the pupil enters the centre of it as convergence and downward gaze starts. If a lens is fitted high, then the patient will start to converge before entering the corridor. This will result in ‘over convergence’ and possible near blur. Conversely, if fitted low, under convergence for the corridor position will result in the corridor being narrow temporally.
The development of progressive lenses, including both the technology behind design and digital production, means that the performance of modern lenses bears little resemblance to those of the last century. While many technologies are similar between different manufacturers, some are unique and the variation in designs from one manufacturer to another is enormous. This tends to mean that if a practitioner changes lens casters, the ‘like for like’ lens lists available mostly represent marketing and pricing information, rather than technology.
For progressive lenses to perform as they should, it falls upon the practitioner to understand the different designs available and how they will suit the individual patient. And of course, it is up to the lens manufacturer to provide enough detailed information for this to be possible. No matter what, it is essential that the manufacturer’s fitting recommendations be followed to achieve the best performance possible. Although corridor length is often built into lifestyle designs, patients still vary in their postural preferences and may prefer something different to the ‘norm’. This makes it important to understand how the lens design affects the power profile of the addition and the implications of shortening the recommended corridor length.
To earn your CPD hours from this article visit: mieducation.com/corridor-conundrumsoptimising-progressive-addition-lenses.

Nicola Peaper BSc (Hons) Ophthalmic Optics, Cert 4 TAE, qualified as an optometrist in the United Kingdom in 1985 and practised in private and corporate practice in there for 20 years. In 2001–02 she was employed as ophthalmic advisor to Kensington, Chelsea, and Westminster Health Authority.
Since moving to Australia in 2005, she has worked in fitting laboratories advising on procedures and quality. In roles as state and national training manager, she has gained extensive experience in presenting the technology behind, and the prescribing and fitting of, ophthalmic lenses.
Nicola Peaper recently retired from her role as Professional Services Manager for Rodenstock Australia.
References
1. Sheedy J, Campbell C, Hayes JR et al., Progressive powered lenses: The Minkwitz theorem. OptomVis Sci. 2005 Oct; 82 (10), 916-924. doi: 10.1097/01. opx.0000181266.60785.c9.
2. Sheedy J. Correlation analysis of the optics of progressive addition lenses. Optom Vis Sci. 2004 May; 81:350-361. doi: 10.1097/01.opx.0000134909.51768.5e.
3. Hill SE, Han H, Thorn F, The ergonomics of reading: The relationship of head and eyes to book position. Invest Ophthal. Vis. Sci. 2006 May;47(13):1184.
4. Mon-Williams M, Burgess-Limerick R, Wann J, et al. Vertical gaze direction and postural adjustment: An extension of the Heuer model. Journal of Experimental Psychology: Applied. 1999, Mar 5(1):35-53. doi: 10.1037/1076-898X.5.1.35.
5. Hutchings N, Irving EL, Lillakas L, et al. Eye and head movement alterations in naïve progressive addition lens wearers. Ophthalmic Physiol Opt. 2007 Mar;27(2):142153. doi: 10.1111/j.1475-1313.2006.00460.x. Erratum in: Ophthalmic Physiol Opt. 2007 May;27(3):320. Lillakas L. [added].
6. Forkel J, Reiniger JL, Baumbach P, et al. Personalized progressive addition lenses: Correlation between performance and design. Optom Vis Sci. 2017 Feb;94(2): 208-2018. doi: 10.1097/OPX.0000000000001016.
7. Köppen W. Progressive memories and calculus [webpage] July 2016; available at: wernerkoeppen.com [accessed May 2024].