mieducation
Elevating Eye Care to Alleviate Digital Dry Eye Symptoms
Many patients suffer from digital eye strain driven or exacerbated by the environments we live and work in. A study has found that Systane Hydration Preservative-Free, which is available in multi-dose bottles and unit dose vials, can relieve the ocular discomfort symptoms associated with digital eye strain. 1 The formulation’s multi-dose container may also appeal to more environmentally aware patients, as Megan Zabell explains.
WRITER Megan Zabell
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Explain the mechanisms behind digital eye strain,
2. Offer evidence-based solutions to help alleviate symptoms of digital eye strain,
3. Describe the features/key ingredients of Systane Hydration Preservative-Free, and
4. Detail the mechanism of the PureFlow technology bottle.
In October 2023 Alcon introduced Systane Hydration Preservative-Free (PF) lubricant eye drops to Australia – the familiar formulation of Systane Hydration UD lubricant eye drops, now available in a 10 ml multi-dose preservative-free bottle.
Some patients may still prefer the environmental sustainability and convenience of a multi-dose eye drop container, hence the need to expand Systane’s multidose preservative-free family. Alcon has been exploring initiatives to reduce its environmental impact, including making the Systane range of ocular lubricants certified plastic neutral through Plastic Bank since the beginning of 2023. For each ton of plastic used to make our Systane range of eye drops, Plastic Bank will collect the same amount of ocean-bound plastic from vulnerable coastal communities. Plastic Bank recycles plastic ocean waste for reintroduction into the global supply chain. Collectors receive bonuses for the materials they collect, which helps them provide basic family necessities such as groceries, cooking fuel, school tuition, and health insurance.
The three products in the multi-dose preservative-free range all offer the unique benefits of the various Systane products, in a 10 ml multi-dose bottle that can be used for up to three months after opening. This is made possible by the PureFlow technology of the bottle. There is a one-way valve at the tip to prevent any backflow into the container. 2
There is also a fine silicone membrane to filter returning air. Both mechanisms aim to prevent contamination of the remaining product in the container. 2 Additionally, the products in the Systane multi-dose preservative-free range feature a relatively soft bottle for comfortable instillation, with a force similar to that of a preserved drop bottle, and a blue tip to assist in targeting when instilling the drops. 2,3
Systane Hydration PF combines the key ingredients of HP-Guar and borate with 1.5% sodium hyaluronate, the salt form of hyaluronic acid (HA), to provide long-lasting dry eye symptom relief, through hydration and protection of the ocular surface. 4-6 This unique combination of ingredients has been shown in a laboratory study to provide two-times greater moisture retention compared with hyaluronic acid alone. 4
Various studies have shown that sodium hyaluronate or hyaluronic acid may have potential wound healing properties. 7 Systane Hydration has been shown, during in vitro testing, to assist with corneal wound healing, making it a suitable recommendation to relieve dry eye symptoms pre- and postocular surgery. 8,9 A study by Carlson and team, investigating the healing effects of various HA-containing eye drops in an in vitro animal model, found that Systane Hydration supported faster corneal reepithelisation compared with the other products tested. 8 Another study found that using Systane Hydration four times a day for a week before cataract surgery and two months after cataract surgery was effective at reducing post-operative discomfort and tear instability. 9
An interesting note is that this study by Favuzza and colleagues compared three groups: those who used Systane Hydration both pre- and post-operatively; those who used the lubricant only post-operatively; and a group who didn’t use ocular lubricants at all in the peri-operative period. 9 While it may be unsurprising that both groups using the ocular lubricant in the peri-operative period had better outcomes (in terms of symptoms, tear break-up time, and fluorescein staining), there were significant differences at certain time points between patients who instilled the lubricant both before and after surgery, as opposed to just after. 9

Figure 1. The Systane multi-dose preservative-free range.
DIGITAL EYE STRAIN AND DRY EYES
A condition often accompanied by symptoms of dry eye, such as sore, watery, red, or tired eyes is digital eye strain, also referred to as computer vision syndrome. 1 The computer vision symptom scale questionnaire (CVSS17) includes questions about symptoms that overlap with dry eye symptoms, including dry, red, wet, or irritated eyes. 10,11 In fact, most signs of dry eye have been shown to correlate with increased screen time in sufferers of computer vision syndrome. 10 This becomes particularly relevant as, according to research conducted by Optometry Australia, 42% of Australians experienced a rise in their screen time in 2022 compared with the previous 12 months. 12 The findings that large proportions of Australians experienced sore or tired eyes when using a computer, tablet, or smartphone whether for work or for personal use, 12 is consistent with the broader research about the link between increased digital device use, digital eye strain, and dry eye symptoms. 1,10
According to the Tear Film and Ocular Surface Society (TFOS) Lifestyle report on the impact of the digital environment on the ocular surface, the definition of digital eye strain is “the development or exacerbation of recurrent ocular symptoms and/or signs related specifically to digital device screen viewing”. 13 The proposed mechanisms of digital eye strain are: altered blinking behaviour – specifically reduced blink rate and incomplete blinking – under corrected or uncorrected refractive error, and underlying binocular vision anomalies. 13 The report stated that while more research is needed to look specifically at the effects of ocular lubricants on the symptoms of digital eye strain, strategies such as improving blinking, optimising the work environment, and encouraging regular breaks may help. Blue light blocking interventions do not appear to help relieve the symptoms of digital eye strain, while nutritional supplements may help. 13
To contribute to the evidence regarding lubricant drop recommendations for modernday sufferers of dry eye symptoms, a study was designed to assess the short-term impact of using Systane Hydration PF on symptoms of dry eye for digital device users. 1 A group of participants who suffer mild-to-moderate dry eye symptoms and used digital devices, was recruited, and instructed to use Systane Hydration PF at least four times per day. Participants were randomised into two groups and used either the unit-dose or multi-dose delivery system of this drop for one week, before switching for a second week. Patients were given a daily log to record the number of drops used and notes about eye comfort throughout the day. At their initial, week one, and week two follow-up visits they completed the Ocular Surface Disease Index (OSDI) and Impact of Dry Eye on Everyday Life Quality of Life (IDEEL-QoL) questionnaires. Comfort was also analysed on a 0–100 visual analogue scale (VAS) with a higher score indicating higher levels of comfort. 1
The participants were surveyed about their digital device use during the study period. Overall their digital device use averaged 12.4 ± 3.9, 12.9 ± 5.0 and 10.7 ± 4.2 hours per day at baseline, week one, and week two respectively. This was split across several different digital devices, including computers, mobile phones, televisions, and tablets. 1
While the instructions were to use the drops at least four times per day, participants were able to use the drops more frequently if they wanted to. On the first day, the average reported drop frequency was 4.4 ± 0.8 drops per day. During the second week, drop frequency grew to 5.1 ± 1.4.9. No explanation was postulated for this change by the authors, but perhaps it could indicate that the patients either became more comfortable with using either delivery format of the drops, or that they enjoyed the relief associated with drop instillation, and some chose to use it closer to five times per day.
“ Systane Hydration PF did help to relieve patients’ dry eye symptoms and improve their quality of life ”
The results of the study indicated that Systane Hydration PF did help to relieve patients’ dry eye symptoms and improve their quality of life. 1 The IDEEL-QoL administered at each visit can be divided into three separate subsections that consider patients’ quality of life in the areas of work, daily activities, and feelings. The questions around work touch on the topics of needing to take breaks or change the way in which the patient works, and feeling distracted or having difficulty concentrating; the daily activities cover tasks such as driving, computer use, close work, wearing makeup or contact lenses, and being around smokers or scented products; whereas the feelings category covers feeling of irritability, impatience, sadness, and attitudes around how people may be perceiving their eyes. Each of these categories improved significantly (p<0.0001) following the use of Systane Hydration PF at least four times per day for two weeks. 1 The work category was the one in which patients experienced the biggest change from baseline. 1 This is especially important considering that the presence of digital eye strain has been associated with lower quality of life and reduced work productivity. 13
The OSDI is a verified 12-item patient questionnaire used to assess symptoms of eye dryness. It can be used to classify the dry eye symptoms as either normal (having no dry eye), mild, moderate or severe, depending on the resulting score. 14 The OSDI result should be a whole number from 0–100, with a lower score indicating less severe symptoms. Patients with a score of 0–12 are classified as normal, 13–22 is mild dry eye, 23–32 is moderate dry eye, and 33–100 is severe dry eye. 14 For this study, all patients recruited initially had an OSDI that classified their symptoms as either mild or moderate (between 13 and 32). At the conclusion of the two-week period there was a significant improvement in the average OSDI (p<0.0001). This improvement also met the minimal clinically important difference (MCID) for mild-moderate dry eye symptoms on the OSDI. 1,14
Ocular comfort was assessed constantly throughout the study using a VAS. Participants were asked to rank their ocular comfort upon waking, at the beginning of digital device use, at the middle of digital device use, at the end of digital device use, and at the end of the day. The VAS ocular comfort scores improved significantly for all time points during the course of the study (p<0.003). 9 LogMAR visual acuities were also assessed in each eye at the baseline, week one, and week two, and there was no statistically significant difference observed. 1
A secondary outcome of the study was to investigate patient preferences for the delivery modality of the drop (a multi-dose container compared to unit dose). 1
Patient preferences were gathered using a Likert survey, which is a series of questions using a satisfaction scale as possible answers. Overall, it was found that the participants were split on which dispensing system they preferred during the study, with 55% preferring the unit dose vials and 45% preferring the multi-dose bottle. When asked if they ‘would’ or ‘probably would’ continue using the different delivery systems, 55% indicated they ‘would’ for unit dose vials, whereas 80% said they ‘would’ for the multi-dose bottle. This is one of the first studies investigating preferences between different delivery systems of the same lubricating eye drop, with similar studies previously being completed with glaucoma drops and not lubricating ones. 1
Interestingly, despite the roughly even preference between the two delivery systems, 80% of participants indicated that they ‘would’ or ‘probably would’ continue using the multi-dose delivery system, compared with 55% for the unit dose vials. A higher proportion of participants indicated that they found the multi-dose container more environmentally friendly in comparison to the unit dose vials as well: 86% for the multidose bottle and 45% for the unit dose vials. 1
ALTERNATIVE STRATEGIES FOR DIGITAL EYE STRAIN SYMPTOM RELIEF
The TFOS Lifestyle report on the impact of the digital environment on the ocular surface identifies the alterations that occur in the tear film and ocular surface that are associated with digital eye strain. These include: tear film instability, enhanced tear evaporation rate, reduced aqueous tear production and volume, meibomian gland dysfunction, and alterations to the tear film lipid and mucin layers. 13
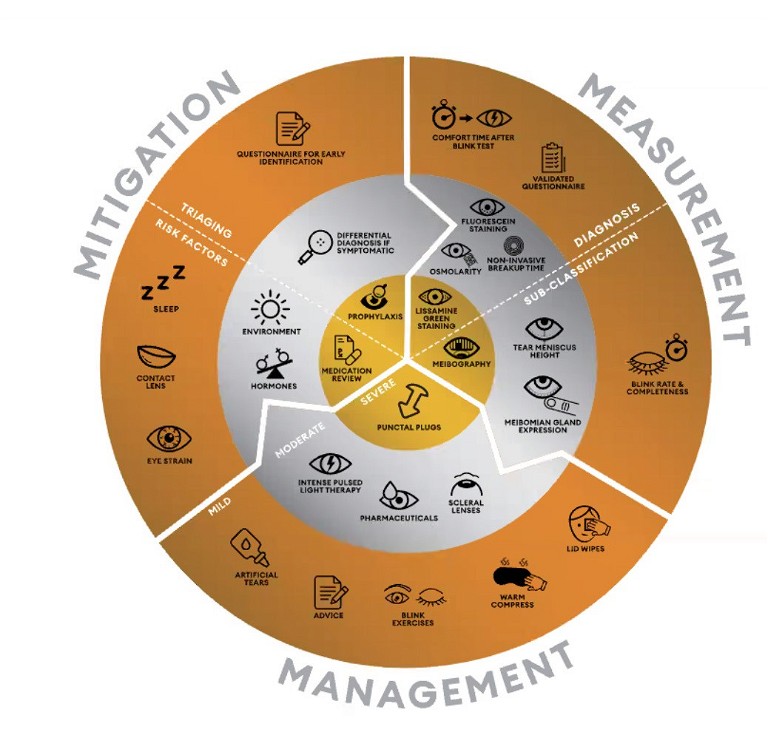
Figure 2. The dry eye wheel.
While effects on the tear film were not measured in this study, there is biological plausibility surrounding its suitability. It also contains the HP Guar technology used in the entire Systane range of lubricating eye drops, plus the added benefits of sodium hyaluronate. HP Guar has been shown to have mucomimetic properties, making it a suitable choice for a condition that presents with altered mucin properties of the tear film. 7 It should also help to improve tear film stability. The demulcents (propylene glycol and polyethylene glycol-400), should bulk up the aqueous layer of the tear film, addressing the reduced aqueous tear volume.
An alternative strategy to consider, although this topic hasn’t yet been addressed in the literature, is to recommend that patients with digital eye strain and dry eye symptoms use an ocular lubricant that helps relieve the symptoms of all types of dry eye (evaporative, aqueous deficient, and mixed dry eye) by supporting both layers of the tear film. 15 Systane Complete has been shown to provide up to eight hours of relief from all types of dry eye and is well-tolerated by patients suffering from dry eye symptoms. 15 It contains a nanolipid complex of mineral oil and phospholipids that migrate to the top of the tear film and fuse with existing tear film lipids to supplement and stabilise gaps that may have developed due to lipid insufficiency, as well as the demulcent propylene glycol and HP Guar to supplement the mucoaqueous layer of the tear film. 15
The TFOS Lifestyle report on the effect of the digital environment on the ocular surface recommends mitigating symptoms of digital eye strain by assessing and managing the different components that can be associated with, or even causative in, this condition. The report recommends assessing the tear film and instigating dry eye management where necessary, assessing the patient’s binocular vision status and instigating oculomotor management where necessary, checking the patient’s refraction and being sure to fully correct it. The TFOS Dry Eye Workshop (DEWS) II group established a comprehensive guide that may simplify the diagnosis of dry eye and make it easier to manage using their four-step recommended therapy algorithm. 7,11 To meet the TFOS DEWS II criteria, a patient must have symptoms of dry eye, and also display ocular signs of a loss of tear film homeostasis, such as a reduced tear break-up time, ocular surface staining, or increased osmolarity. For those unfamiliar, the World Council of Optometry (WCO) worked with members of TFOS and developed the dry eye wheel, which is a useful clinical tool for day-to-day reference. An interactive version of this, along with a series of webinars detailing the process behind developing the wheel, and how it may be applied in clinic, are available on the WCO website.
Ultimately, many patients are suffering from digital eye strain because of the environments we all live and work in. Digital eye strain can be driven or exacerbated by changed blinking behaviours that lead to tear film instability, binocular vision abnormalities, and/or uncorrected refractive error. It is recommended to assess the tear film of patients presenting with symptoms of dry eye and digital eye strain, and to address any underlying dry eye. Systane Hydration PF has been shown to relieve the ocular discomfort symptoms associated with digital eye strain. 1 It is available in Australia in either a multi-dose bottle or unit dose vials and, although there is no clear patient preference for one over the other, patients may be more likely to continue to use the multi-dose preservative-free bottle and they may find it more environmentally friendly. 1 For patients concerned about the environmental impacts of their ocular lubricants, it can be good to know that all Systane eye drops in Australia and New Zealand are certified plastic neutral through Plastic Bank.
To earn your CPD hours from this article visit mieducation.com/elevating-eye-care-to alleviatedigital-dry-eye-symptoms.
Megan Zabell is employed by Alcon, manufacturer of Systane products.
AU-SYY-2400001
References
1. Pucker, A.D., Lievens, C., Wolfe G.S., et al., Quality of life in digital device users who are treated with Systane Hydration PF. Clin Optom (Auckl). 2023; 15: 45–54.
2. Campolo, A., Crary, M. and Shannon, P., A review of the containers available for multi-dose preservative-free eye drops. Biomed J Sci & Tech Res 2022; 45: 36035–36044.
3. Davidson, Z. and Rose, C., The pivotal role played by device developers to improve patient eye care. On Drug Delivery 2021; 118: 14–18.
4. Rangarajan, R., Kraybill, B., Ogundele A., Ketelson H.A., Effects of a hyaluronic acid/hydroxypropyl guar artificial tear solution on protection, recovery, and lubricity in models of corneal epithelium. J Ocul Pharmacol Ther. 2015; 31(8): 491–497.
5. Davitt, W.F., Bloomenstein, M., Christensen, M., Martin, A.E., Efficacy in patients with dry eye after treatment with a new lubricant eye drop formulation. J Ocul Pharmacol Ther. 2010; 26(4): 347–353.
6. Rolando, M., Autori, S., Badino, F., Barabino, S., Protecting the ocular surface and improving the quality of life of dry eye patients: a study of the efficacy of an HP-guar containing ocular lubricant in a population of dry eye patients. J Ocul Pharmacol Ther. 2009; 25(3): 271–278.
7. Jones, L., Downie, L.E., Korb, D., et al., TFOS DEWS II management and therapy report. Ocul Surf. 2017; 15(3): 575–628.
8. Carlson, E., Kao, W.W.Y., Ogundele, A., Impact of hyaluronic acid-containing artificial tear products on reepithelialization in an in vivo corneal wound model. J Ocul Pharmacol Ther. 2018; 34(4): 360–364.
9. Favuzza, E., Giansanti, F., Mencucci, R., et al., Protecting the ocular surface in cataract surgery: The efficacy of the perioperative use of a hydroxypropyl guar and hyaluronic acid ophthalmic solution. Clin Ophthalmol. 2020; 14: 1769–1775.
10. Sánchez-Valerio, M.D.R., Baez Duarte, B.G., Vallejo-Ruiz, V., Dry eye disease association with computer exposure time among subjects with computer vision syndrome. Clin Ophthalmol. 2020; 14: 4311–4317.
11. Wolffsohn, J.S., Arita, R., Chalmers, R., et al., TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017; 15(3): 539–574.
12. Optometry Australia. 2022 Vision Index. Available at optometry.org.au/wp-content/uploads/GVFL/Vision_ Index/2022-Vision-Index-Report.pdf [accessed Feb 2024].
13. Wolffsohn, J.S., Lingham, G., Downie, L.E., et al., TFOS Lifestyle: Impact of the digital environment on the ocular surface. Ocul Surf. 2023; 28: 213–252.
14. Miller, K.L., Walt, J.G., Mink, D.R., et al., Minimal clinically important difference for the ocular surface disease index. Arch Ophthalmol. 2010; 128(1) :94–101.
15. Silverstein, S., Yeu, E., Tauber, J., et al., Symptom relief following a single dose of propylene glycol-hydroxypropyl guar nanoemulsion in patients with dry eye disease: A phase IV, multicenter trial. Clin Ophthalmol. 2020; 14: 3167–3177.

Megan Zabell graduated from the University of Melbourne as a therapeutically endorsed optometrist and later returned to complete her Master of Clinical Optometry. She worked in a private optometry practice for seven years and also taught preclinical optometry at the University of Melbourne. Ms Zabell is passionate about the diagnosis and treatment of dry eye, as well as fitting contact lenses. She has been a member of Alcon Vision Care’s professional affairs team since 2018.