mieducation
Finding Focus with a Myopia Management Strategy
Myopia is associated with socio-economic consequences, visual impairment, and secondary diseases in adulthood. Therefore, and because of its increasing prevalence worldwide, a strategy is needed to minimise the impact of myopia. On this basis, for several years the optical and ophthalmic industry has been putting a lot of effort into providing tools to control and manage myopia progression during its different stages: onset, progression, and stabilisation. Myopia control management represents a paradigm shift in treatment for myopia, from correcting a refractive error to managing its various stages with a well-defined focus and strategy.
As Nicola Peaper writes, the aim of myopia management is to detect the development of myopia as early as possible, and to act as soon as possible. In this regard, every dioptre counts.
WRITER Nicola Peaper
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Realise that peripheral refraction and eye length varies in different parts of the retina,
2. Realise that differences of asymmetries in the peripheral refraction and the eye shape can be demonstrated for progressive and non-progressive myopes, and
3. Understand how a spherical single vision lens can, in certain children, cause axial elongation.
In 2016 Holden et al1 estimated that by 2050 approximately five billion people would require correction for myopia and about 900 million of those would suffer from high myopia.
The Australia and New Zealand Child Myopia Report 2022/23 – Reducing the Risk to Vision,2 updates these figures locally to 55% of the population being myopic by 2050 with a current rate of 36%. The report goes on to state: “Furthermore, Australia is expected to have 4.1 million high myopes (-6.00D and over) and New Zealand over 600,000 high myopes by 2050, unless myopia management is implemented by everyone, and many more children have eye examinations at five to six years of age.”
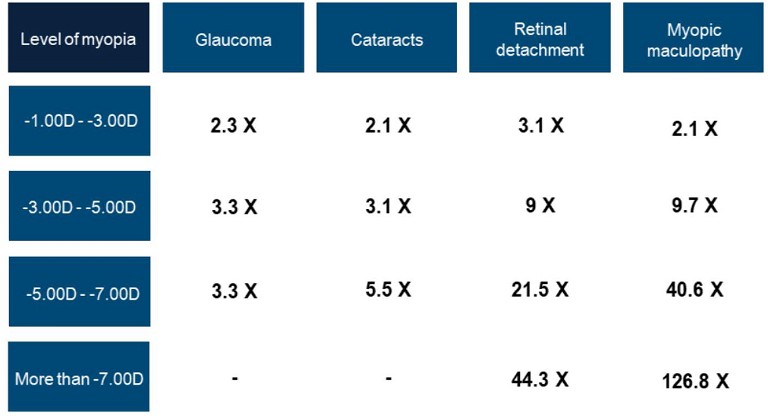
Figure 1. Risk of developing certain diseases according to the level of myopia (adapted from Flitcroft, 2012).4
While we all may be aware of the implications of developing myopia during the growth stage, it is also important to consider the longterm implications and consequences. Where myopia progresses, the risk of developing certain eye disorders, such as glaucoma, cataract, macular disorders, and/or retinal detachment, increases.
Studies have shown that the risk associated with diseases resulting from myopia increases dramatically according to the level of myopia.3–5 Figure 1 shows how these risks vary depending on the individual’s myopia. For example, in the case of an individual with myopia between -3 and -5D, the risk of retinal detachment is nine times higher than the risk for an emmetrope. This goes up to a staggering 44 times higher risk once the myopia goes over -7.00D and nearly 127 times higher risk of maculopathy.
It is, therefore, extremely important to encourage early detection and to attempt to slow the progression of myopia from the moment it is detected. Slowing the progression of myopia by one dioptre during childhood reduces the risk of developing myopic maculopathy by 40%.4,5
As practitioners, we need to be able to identify those children most at risk and monitor and advise accordingly. Myopia has a multifactorial aetiology, with genetic, behavioural, gender, and environmental factors playing a significant role:
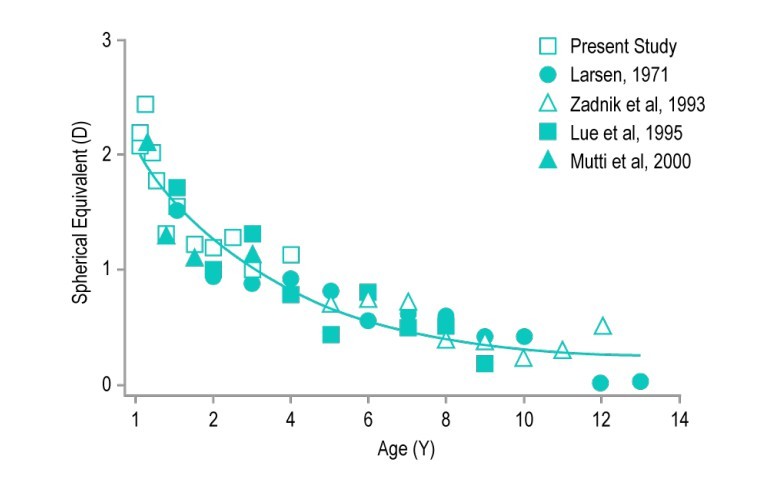
’ Figure 2. Normal refractive development of a child’s eye
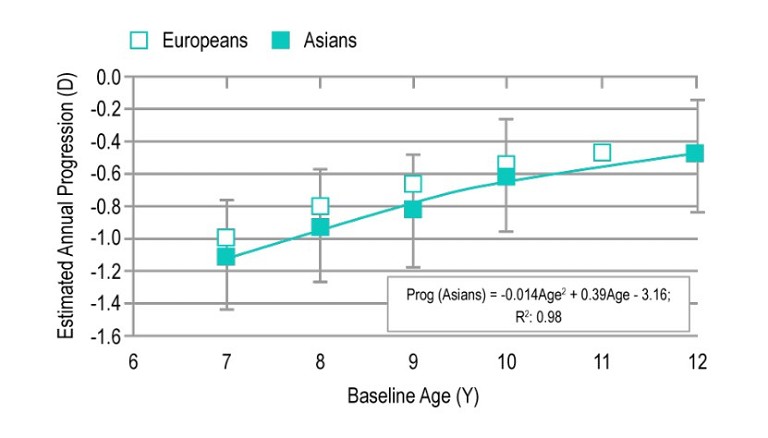
Figure 3. Cumulative progression of myopia, based on age of onset (adapted from Mayer, 2001).13 (adapted from Donovan et al., 2012).6
• Ethnicity plays a role in myopia development, with Asian people being at higher risk.6In one study, the mean cumulative progression over three years is about 35% higher for Asians than for Caucasians.7
• Children of myopic parents have an increased risk of becoming myopic themselves: The prevalence in children with two myopic parents (35–60%) is higher than in children with one myopic parent (25–40%) and much higher than in children with emmetropic parents (5–15%).8
• Lifestyle and visual health, in other words time spent in close work and time spent outside, play a major role in myopia development.9,10
According to Australia’s Professor Ian Morgan, “There has been speculation about the role of education in relation to myopia for at least several hundred years. The association between education and myopia can be seen at a number of levels and has been extensively reviewed.”11 Huang Hsiu-Mei et al. did a systemic review of the research of the association of near work and myopia and made the following deductions:12
• “Environmental influences related to prolonged reading or near work as well as fewer hours spent outdoors are associated with a higher prevalence of myopia.”
• “A systematic review and meta-analysis to identify the association between time spent outdoors and myopia indicated a 2% reduced odds of myopia per additional hour of time spent outdoors per week after adjustment for covariates.”
• “If a child has four hours per day of near work (33cm) in tutorial classes after school during weekdays (Monday to Friday), then he would most likely have 120% of additional odds of myopia.”
• “The association between near work and myopia indicated a 2% increased odds of myopia per additional diopter-hour of time spent on near work per week.”
MONITORING A CHILD’S DEVELOPMENT
Having the ability to identify those at risk allows practitioners to monitor and advise on visual hygiene.
The development of a child’s eye is highly complex. The key to detecting the onset of myopia is to monitor the process of emmetropisation and the deviations that may occur during this process. Due to its characteristics, the eye at birth is hyperopic, developing towards slight hyperopic stabilisation around the age of six or seven as a result of eye growth. Having curves of normal emmetropisation, such as seen in Figure 2, helps practitioners to monitor the emmetropisation process.
Several apps are available that allow for monitoring and forecasting of myopia, one of which is available on Rodenstock CNXT. CNXT is a platform that has dispensing modules to help discuss various lens choices with patients and this now includes a myopia control program. Patient details, such as gender, number of myopic parents, outdoor hours, near vision work hours, biometry (if available), and script are entered. The program then generates a forecast of myopia evolution and, if biometry is available, axial length evolution. The risks involved of higher amounts of close work and reduced amounts of time outside can be demonstrated to patients and parents to encourage good visual hygiene. Finally, the program can be used to track the subsequent evolution.
Programs such as this are based on the data of various scientific studies looking at the development of myopia in children and young adults, and are intended as a rough guide only. Even so, they form a valuable tool in the education of parents and children who are developing myopia.
The progression rate of myopia varies according to the aetiology and age of the onset, as shown in Figure 3. With an onset of myopia around the age of six, the progression rate is approximately one dioptre per year, dropping to about 0.5 dioptres per year with an onset at age 10.14 This supports the argument that the first lens prescribed for childhood myopia should be a lens that slows the rate of progression.
PAST TREATMENT OPTIONS
Until recently, the most common lens used to correct myopia has been a standard minus single vision lens. These lenses create a divergence of light, forming a sharp image on the centre of the retina.
However, correcting myopia with single vision lenses projects light in the periphery behind the retina.15 Tabernero et al (2009) measured the peripheral refractions of nine myopic eyes, both with and without their regular single vision spectacles. They found that all subjects became more hyperopic in the periphery when measured with their spectacle corrections versus without correction. They also found that there was a large variability in the amount of relative hyperopia in the periphery.15
For some children, this peripheral hyperopia causes their eyes to try to adapt and grow even longer, which causes the myopia to progress further (Figures 4A and B). Because of this, normal single vision lenses are not designed to control myopia progression.
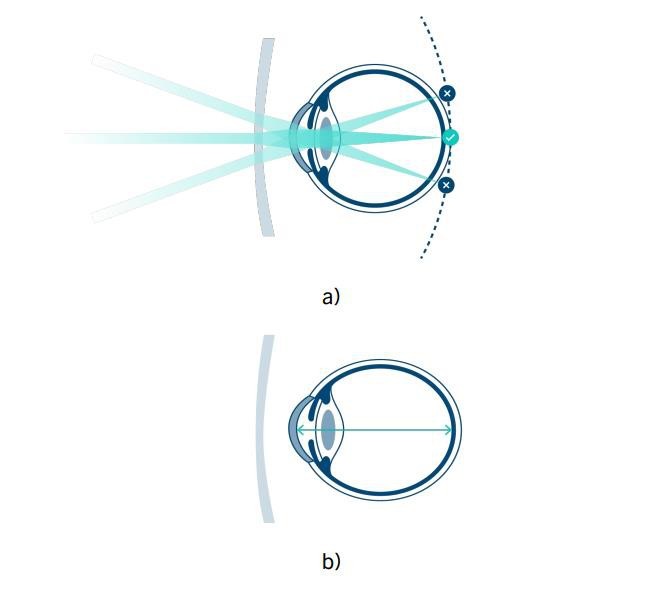
Figure 4. (A) Myopia correction with standard lenses. (B) Axial elongation of a myopic eye.
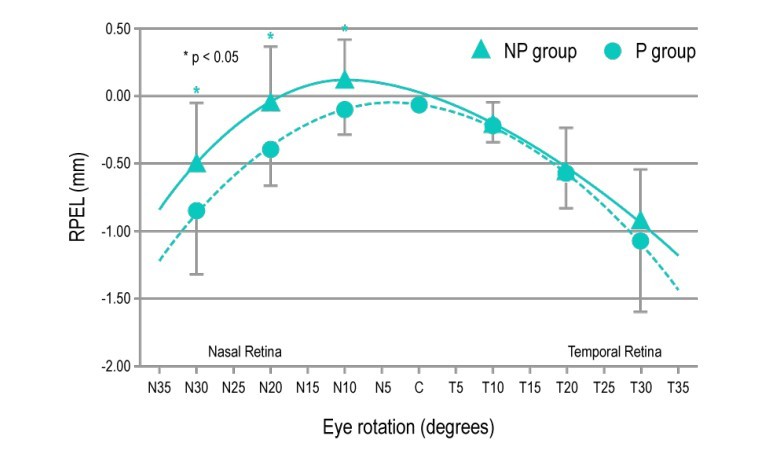
Figure 5. Differences between peripheral axial length in myopic eyes in experimental groups of progressing myopes (P) and non-progressing myopes (NP). Adapted from Faria-Ribeiro et al., 2013.21
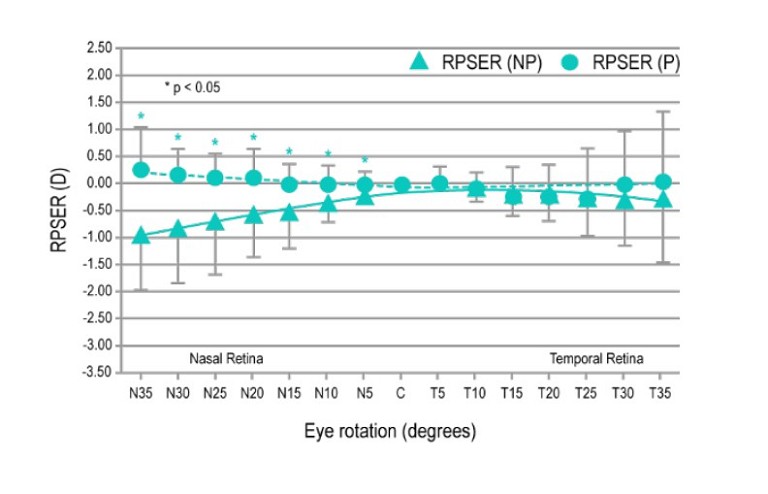
Figure 6. RPSER (Relative peripheral spherical equivalent refraction) as a function of the eye rotation angle for the non-progressing (NP) and progressing (P) myopes (*p < 0.05). Adapted from Tabernero et al., 2009.15
Consequently, lenses are needed that aim to slow eye elongation and thus, control myopia progression in children. These lenses need to refract light in the periphery to hit in front of the retina while ensuring sharp central vision.
PERIPHERAL RETINAL ASYMMETRY
For nearly a century there has been research into the peripheral shape and peripheral refraction of the retina. A 1932 paper16 found a considerable difference in the peripheral refraction between the nasal and temporal halves of the field. Further examples of this include Millodot in 198117 and Mutti et al. in 2000.18 Both concluded that myopes are more hyperopic in the retinal periphery than hyperopes and emmetropes.
A 2002 study by Seidemann et al.19 confirmed that myopic eyes are relatively more hyperopic (or less myopic) in the periphery and suggested, “It could even be that myopia in the periphery is a trick of nature to produce a constant inhibitory signal to prevent too much eye growth”. Dr Anne Seidemann is currently a senior member of Rodenstock’s research and development department.
Aitchison et al.20 found that length, height, and width of eyes increase as myopia increases in the approximate ratio of 3:2:1. He stated that, “The relative difference in the increase of these dimensions meant that as the degree of myopia increased, the retinal shape decreased in oblateness… few myopic eyes were prolate.”
This paper also includes a possible framework for the development of myopia:
If light is incident from an off axis point on an emmetropic eye with a relatively flat shape, the light will focus in front of the retina (relative myopia), compared to an emmetropic eye with a steeper curve where light will focus behind the retina (relative hyperopia). In the case of the light focussing behind the retina, it is possible that the eye will respond to the peripheral relative hyperopia by elongating.20
In 2013, Faria-Ribeiro et al.21 studied two groups of myopes. One group contained non-progressing myopes (NP group) while the other group had progressing myopes (P group). The results show significant differences in peripheral axial length and relative peripheral spherical equivalent refraction in the nasal retinal hemifield between both groups.
“ As practitioners we need to be able to identify those children most at risk and monitor and advise accordingly ”
• There was significant nasal / temporal asymmetry in the relative peripheral eye length in the non-progressing group with a longer nasal shape than temporal. The progressing group displayed more symmetry nasal to temporal. They therefore concluded that nasal-temporal asymmetry in peripheral axial length may be linked to less myopia progression (NP group in the graph, Figure 5).
• When considering the relative peripheral spherical equivalent refraction, the progressing group had a slightly more hyperopic peripheral refraction in the nasal hemifield, while the non-progressing group had a more myopic peripheral refraction (Figure 6).21
The differences between nasal and temporal retina are not limited to peripheral refraction and length. In 1990, Curcio et al.22,23 showed there is an anatomical asymmetry in the retina in the nasal and temporal regions. The nasal retina has a greater density of ganglion cells and greater numbers of cones. Curcio implied that this suggested a neurofunctional dominance of the nasal retina.
OPTIONS FOR MYOPIA MANAGEMENT
There are various options available for managing myopia that slow the rate of progression. These options may be pharmaceutical or optical solutions and complement the lifestyle and visual behavioural factors previously mentioned.
Low dose atropine is one method that has proven highly effective but low doses are necessary to reduce possible side effects such as blurred vision, accommodative disorders, photophobia etc. There is also the possibility of a rebound effect upon discontinuing treatment.
Contact lenses, both soft multifocals and orthokeratology (OK), again show high efficacy in children. The use of contact lenses for myopia necessitates compliance with safety and hygiene protocols, as they can cause corneal complications if the lenses are handled improperly or carelessly. However, the risk of microbial keratitis in children wearing OK has been found to be around one to two cases per 2,000 wearers, per year.24
Spectacle lenses, if effective, are non-invasive and easy to use. From all the research quoted, it is apparent that a lens to control myopia should cause light to focus in front of the retina in the periphery while giving clear and sharp central vision.
The study by Tabernero et al in 2009,15 as well as measuring peripheral refractions both with and without normal spectacles, also measured the peripheral refractions of eyes using radial refractive gradient lenses (RRG). These lenses were designed to optimise two optical features: first, clear foveal vision in the optical centre and second, a steady increase of positive power in all radial directions. The increase in spherical equivalent refractive power was about one dioptre for every 10° to the periphery in the visual field, with a central clear area with a diameter of 6mm – about the diameter of the pupils of the young subjects under mesopic conditions. They reported that while conventional spectacle correction induced a variable amount of hyperopia, in contrast RRG lenses generally induced relative peripheral myopia as expected from their theoretical design. While RRG lenses produced the desired effect of focussing light in front of the retina, they had the disadvantage of optical distortions induced by the refractive gradient.
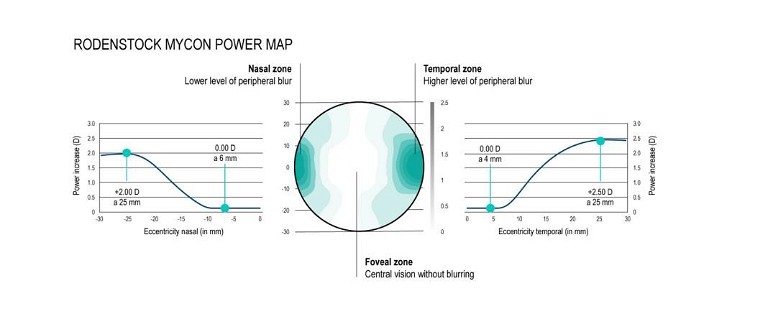
Figure 7. Schematic illustration of the power distribution of the MyCon lens.
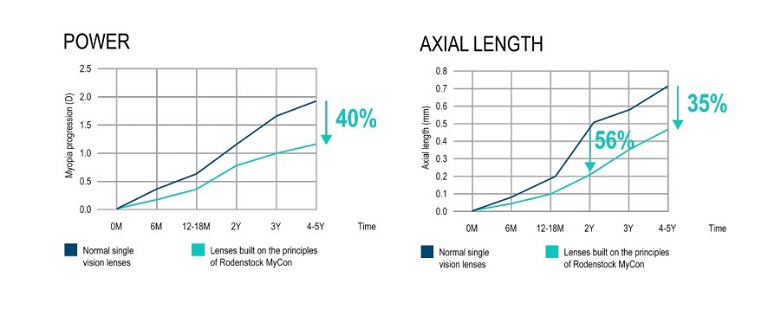
Figure 8. Results of the clinical study carried out with lenses, on which technological principles the MyCon lens is based. In blue, the control group’s development; in mint, the experimental group’s development. Adapted from Tarutta et al., 2019.26
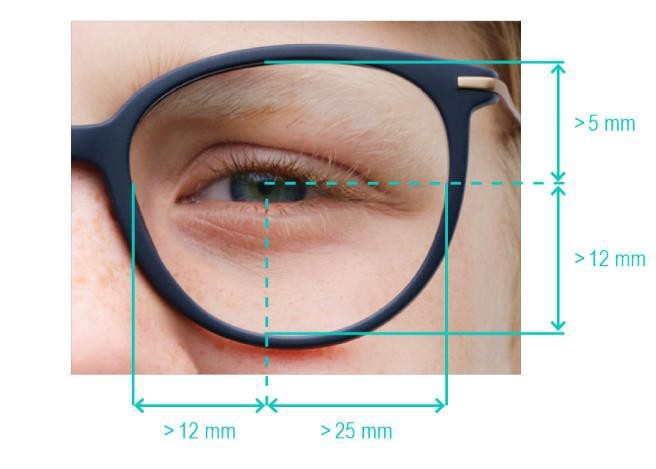
Figure 9. Recommended minimum fitting dimensions.
Testing of the comfort and wearability of RRG lenses25 showed head movement patterns were clearly affected by the imposed peripheral defocus that was generated by the lens. Head movement patterns were severely altered during near vision tasks as the subjects needed to bend forward to use the clear area.
RODENSTOCK MYCON DESIGN
MyCon is a peripheral defocus lens with a horizontally asymmetrical design. It has a central vision zone, which provides stable refraction around the optical centre, while the outer areas create a peripheral progression along the horizontal meridian (Figure 7).
The lens has three distinct zones:
• A central zone, where the optical power corresponds to the wearer’s nominal refraction,
• A temporal zone of progressively increasing power up to 2.5D, and
• A nasal zone of progressively increasing power up to 2.0D.
The asymmetry of the nasal and temporal power increase allows for the higher relative peripheral spherical equivalent refraction present nasally in progressing myopes. As such, in contrast to standard lenses, the MyCon lens refracts light from the periphery to be focussed in front of the retina to reduce myopia progression.
As the design is aimed purely at the horizontal median, this allows for easier adaptation and ease of use for close work.
EFFICIENCY
A lens on which technological principles the MyCon lens is based has been clinically tested in an independent study conducted over five years with Caucasian children. This long-term study has shown that myopia control lenses, such as MyCon, reduce the progression of myopia by 40% in comparison to single vision lenses. 26
The study monitored the myopia progression of a group of 146 Caucasian boys and girls, with myopia varying between -1.00 and -6.00D. The participants were divided into two groups with the same average age of 10.5 years.
The first experimental group consisted of 94 participants (aged seven to 14 years) who used lenses based on the same principles as MyCon lenses, while the second control group consisted of 52 participants (aged eight to 14 years) who used normal single vision lenses.
The study was conducted by the Helmholtz National Medical Research Centre for Eye Diseases of the Russian Ministry of Health.
During the study, myopia progression (mean power and axial length) was assessed after six months, 12–18 months, two years, three years, and four to five years from the start of lens wear.
The results of the study (Figure 8) show that the lens, on which technological principles the MyCon lens is based, slowed myopia progression by 40% when compared with the control group. Furthermore, axial elongation was reduced by up to 56% after two years and 35% after four to five years.
USING MYCON
The advantages of MyCon include:
• It is a non-invasive system for the treatment of myopia, which improves the wearer’s compliance.
• Axial length measurements show effectiveness in slowing down myopia progression up to 56% after two years. The reduction of myopia progression still exists after four to five years with lenses on which technological principles of the MyCon lens is based. The effect is about 35% for eye length or 40% in terms of refraction.
• The asymmetrical distribution of the horizontal defocus is controlling the eye length elongation26 while optimising the wearer’s comfort. This progressive defocus is achieved by a seamless power transition from the focus area to the progressive control area, thus avoiding image jumps.
• As the design is based on free-form technology, it is easy to produce in a wide range of indexes including 1.5, 1.6, 1.67 and 1.74, and either hard coated or antireflection coated (depending on index). As high index materials are available, the power range is considerable, -14.00D (+6.00D cyl combined).
As with most of the lenses used in myopia control, the MyCon lens should be fitted according to the requirement of eye rotation like aspherical lenses. This means fitted for zero gaze direction and vertical frame plane. This can be achieved with the patient looking straight ahead and dropping the ordered height by 1mm for every 2° of pantoscopic tilt.
To make use of the horizontal progressions, a minimum frame size is necessary (Figure 9). The maximum back vertex distance on the dispensed frame should not exceed 14mm.
The adaptation period is approximately two weeks, during which the wearer’s habits may change to properly adapt to the new geometry of the lenses. In particular, due to the peripheral defocus and potential blurry vision that may occur when looking outside of the optical axis, it is recommended to closely monitor the wearer during the first two weeks of adjustment. While it is recommended that the MyCon lens be worn full-time, this would obviously exclude extreme sports where clear peripheral vision is important.
The MyCon lens is specially designed to slow the progression of myopia in children. In addition to glasses, behaviours such as spending more time in daylight or taking regular breaks from near work can help slow the progression of myopia.
According to the guidelines set out by the International Myopia Institute (IMI),27 the best practice for myopia management includes full correction of myopic refractive errors, education on and treatment of risk factors, as well as visual health.
To earn your CPD hours from this article, visit mieducation.com/finding-focus-with-a-myopiamanagement-strategy.
Material source: Rodenstock White Paper 11/01/2023. Mycon by Rodenstock.
“ The MyCon lens is specially designed to slow the progression of myopia in children ”
References
1. Holden, B.A., Fricke, T.R., Wilson, D.A., et al., Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016; 123:1036–42.
2. The Australia and New Zealand Child Myopia Working Group, The Australia and New Zealand Child Myopia Report 2022/23 – Reducing the Risk to Vision, Adjunct Report, Nov 2022, available at: optometry.org.au/ wp-content/uploads/National_news_images/2022/ November/Reducing-the-Risk-to-Vision_Myopia- Report-202223.pdf [accessed 13 June 2023].
3. Bullimore, M.A., Brennan, N.A., Myopia Control: Why each diopter matters. Optom Vis Sci. 2019 Jun;96(6):463–465.
4. Flitcroft, D.I., The complex interactions of retinal, optical and environmental factors in myopia aetiology. Progress in Retinal and Eye Research Volume 31, Issue 6, November 2012, 622–660.
5. Haarman, et al., The complications of myopia: A review and meta-analysis. Investigative Ophthalmology & Visual Science April 2020, Vol.61, 49.
6. Donovan, L., Sankaridurg, P., Ho, A., et al., Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012.
7. Sankaridurg, P., IMI Impact of Myopia. Investigative Ophthalmology & Visual Science April 2021, Vol.62, 2.
8. Wu, M., Edwards, M.H., (1999), The effect of having myopic parents: An analysis of myopia in three generations. Optometry and Vision Science, 76(6), 387–392. doi.org/10.1097/00006324-199906000-00018.
9. Tang, S.M., Kam, K.W., French, A.N., et al., Independent influence of parental myopia on childhood myopia in a dose-related manner in 2,055 trios: The Hong Kong Children Eye Study. American Journal of Ophthalmology, 218, 199–207. doi.org/10.1016/j.ajo.2020.05.026.
10. Mutti, D.O., Mitchell, G.L., Moeschberger, M.L., et al., (2002). Parental myopia, near work, school achievement, and children’s refractive error. Investigative Ophthalmology & Visual Science, 43(12), 3633–3640.
11. Morgan, I. et al., Risk factors for myopia, Investigative Ophthalmology & Visual Science April 2021, Vol.62, 3.
12. Huang, H-M., D Chang, DS-T., Wu, P-C., The association between near work activities and myopia in children—A systematic review and meta-analysis. PLoS ONE 10(10): e0140419. doi.org/10.1371/journal. pone.0140419
13. Mayer, D.L., Hansen, R.M., Moore, B.D. et al., Cycloplegic refractions in healthy children aged 1 Through 48 Months. Arch Ophthalmol. 2001;119(11): 1625–1628.
14. Donovan, l., et al., Myopia progression rates in urban children wearing single vision spectacles. Optom Vis Sci. 2012 January; 89(1): 27–32.
15. Tabernero, J., Vazquez, D., Seidemann, A., et al., (2009). Effects of myopic spectacle correction and radial refractive gradient spectacles on peripheral refraction. Vision Research, 49(17), 2176–2186.
16. Ferree, C.E., Rand, G., Hardy, C., Refractive asymmetry in the temporal and nasal halves of the visual field. American Journal of Ophthalmology Volume 15, Issue 6, June 1932, 513–522.
17. Millodot, M., The effect of ametropia on peripheral refraction, American Academy of Optometry, 1981.
18. Mutti, D.O., et al., Peripheral refraction and ocular shape in children. Investigative Ophthalmology & Visual Science April 2000, Vol.41, 1022–1030.
19. Seidemann, A., Schaeffel, F., Guirao, A., et al., (2002). Peripheral refractive errors in myopic, emmetropic, and hyperopic young subjects. Journal of the Optical Society of America A, 19(12), 2363.
20. Aitchison, D.A., Pritchard, N., Schmid, K.L., et al., Shape of the retinal surface in emmetropia and myopia. Investigative Ophthalmology & Visual Science, August 2005, Vol. 46, No. 8.
21. Faria-Ribeiro, M., Queirós, A., Lopes-Ferreira, D., et al., Peripheral refraction and retinal contour in stable and progressive myopia. Optom Vis Sci. 2013.
22. Curcio C.A, Allen K.A. Topography of ganglion cells in human retina. J Comp Neurol. 1990 Oct 1;300(1):5-25. doi: 10.1002/cne.903000103. PMID: 2229487.
23. Curcio, C.A., Sloan, K.R., Kalina, R.E. and Hendrickson, A.E. (1990), Human photoreceptor topography. J. Comp. Neurol., 292: 497-523. doi.org/10.1002/cne.902920402.
24. Myopia Profile, Optimizing safety in orthokeratology, 6 September 2022. Available at myopiaprofile.com/optimizing-safety-in-orthokeratology/ [accessed 14 June 2023].
25. Vazquez, D., Seidemann, A., Altheimer, H., et al., Optical tracking of head movement patterns when wearing spectacle lenses with different radial power profiles. Investigative Ophthalmology & Visual Science April 2009, Vol.50, 3981.
26. Tarutta, E.P., Proskurina, O.V., Tarasova, N.A., et al., (2019). Long-term results of perifocal defocus spectacle lens correction in children with progressive myopia. Vestnik Oftal’mologii, 135(5), 46.
27. IMI Clinical Management Guidelines Report available at: myopiainstitute.org/imi-whitepaper/clinicalmanagement-myopia-guidelines-report/ [accessed 14 June 2023].

Nicola Peaper qualified as an optometrist in the UK in 1985 and practised in private and corporate practice in the UK for 20 years. In 2001–02 she was employed as Ophthalmic Advisor to Kensington, Chelsea & Westminster Health Authority.
Since moving to Australia in 2005, she has worked in fitting laboratories, advising on procedures and quality. In roles as state and national training manager she has gained extensive experience in presenting the technology behind, and the prescribing and fitting of ophthalmic lenses.
Nicola Peaper is currently Professional Services Manager for Rodenstock Australia.