mieducation
Making Dry Eye Management Stick
How often do patients say they have tried lubricating eye drops and they feel short-term relief from dry eye disease (DED), but are searching for something more long lasting?
In this article, Helen Gleave talks to Dr Jacqueline Tan-Showyin, from the Eye Research Group at the University of New South Wales (UNSW Sydney), to discover more about her team’s research on the use of different lubricating eye drops in the management of DED.
WRITER Helen Gleave
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Understand the importance of the tear film in maintaining the integrity of the ocular surface,
2. Realise the link between dry eye disease and health-related quality of life markers, and
3. Be aware of the role of hyaluronic acid in commercial eye drops, and why retention and efficacy varies.
Dry eye disease affects hundreds of millions of people globally and is one of the most common reasons why patients visit eye care practitioners. 1 Dry eye is more prevalent in women, in those of Asian ethnicity, and with increasing age, 2 and significantly impacts people’s ability to perform their normal daily activities, thereby negatively affecting quality of life.” 1
In a 2023 literature review of randomised controlled trials comparing the efficacy of artificial tears in patients with dry eye, the authors concluded that combination formulations were more effective than single active ingredient artificial tears.3
The same literature review noted that artificial tears are the mainstay of dry eye disease management, but also have a role in corneal abrasion and wound healing, as well as pain and inflammation management.3
Dry eye is an area of research that has interested Dr Jacqueline Tan-Showyin, a Senior Research Fellow and Director of the Eye Research Group at the School of Optometry and Vision Science, UNSW Sydney. The group was established to foster collaborations with industry.
“I am very fortunate to conduct well-designed clinical trials to develop, and therefore be the first to evaluate, new treatments for dry eye,” said Dr Tan-Showyin, “as well as conducting research studies to assess the efficacy of existing treatments to provide evidence for best practices.”
Dr Tan-Showyin highlighted the importance of continued research into dry eye management. “The tear film is vital in maintaining the integrity of the ocular surface, including immunological protection, hydration, oxygenation, nourishment, and maintenance of a smooth optical surface,” she explained.4
IMPACT ON QUALITY OF LIFE
There’s also a proven link between dry eye and health-related quality of life (HR-QoL). In a large cross- sectional population-based study, 5 HR-QoL was measured using the 36item short form survey (SF36) questionnaire, which aggregates scores of different functions (such as physical functioning and social functioning) into two summary scores: the Physical Component Summary and the Mental Component Summary.
Compared with other common systemic and chronic disorders, DED was distinctive by having a substantial reduction in both the Physical Component Summary and the Mental Component Summary. While the other chronic conditions primarily affected either mental or physical quality of life, highly symptomatic dry eye stands out by substantially reducing both physical and mental quality of life. This risk remained significant after correction for comorbidities (P < 0.0005).5
Other key findings were also incredibly insightful. Increasing DED symptom frequency was associated with decreasing HR-QoL, but interestingly, subjects with undiagnosed DED had a significantly increased risk of low mental HR-QoL with increasing dry eye symptoms compared with diagnosed subjects (P < 0.0005).5 To underline the impact dry eye has on quality of life, compared with other eye conditions such as allergic conjunctivitis, glaucoma, macular degeneration, and retinal detachment, DED showed the highest risk of low HR-QoL. 5
The risk of low Physical Component Summary with DED is similar to that of chronic obstructive pulmonary disease (COPD) and irritable bowel syndrome (IBS). Younger age and male sex were associated with a greater impact of highly symptomatic dry eye on physical quality of life.55Significantly, the risk of a low Mental Component Summary was higher for dry eye than for all other chronic conditions, except for depression. This is the first study to demonstrate conclusively that dry eye is associated with reduced mental HR-QoL by using validated questionnaires, and certainly serves to highlight the importance of proactive identification and management. 5
“Currently, the Tear Film and Ocular Surface Society (TFOS), a world leader in eye health education, has defined dry eye in the Dry Eye Workshop II report as ‘a multifactorial disease of the ocular surface characterised by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neuro-sensory abnormalities play etiological roles’,”6 Dr Tan-Showyin continued.
“Dry eye is a significant and complex, functional disorder, that has been classified into two broad categories – evaporative, which is more common, and aqueousdeficient – but these exist as a continuum, and as dry eye disease progresses, a mix of both becomes more frequent.6 Proper diagnosis, recognising the major cause of patients’ dry eye condition, is essential to enable the selection of the most appropriate treatment that targets one or more layers of the tear film. However, current evidence regarding the relative benefits of different management options is limited. 7
“The mainstay of dry eye therapy is ocular lubricants designed to supplement the natural tear film. To enhance lubrication and prolong retention time on the ocular surface, a variety of viscosityenhancing agents are incorporated. These include carboxymethylcellulose (CMC), hydroxypropyl methylcellulose (HPMC), hyaluronic acid (HA), hydroxypropyl-guar (HP-guar), polyethylene glycol, and different combinations of these.7
“However, the sheer number of different tear supplement formulations available can be incredibly confusing to both patients and practitioners alike. This has also been exacerbated by the increasing availability of preservative-free formulations and unpreserved multidose dispensers with unilateral valves, designed to avoid issues associated with chronic exposure of the ocular surface to preservatives.7
“Therefore, well designed studies and good quality research are important to understand how different formulations assist in managing different types of dry eye, to support their selection and use.”
RETENTION TIME
One area of research Dr Tan-Showyin and her team are investigating is the difference in retention time of various lubricating eye drops on the eye after instillation. What is the importance of this research?
“A healthy tear film is vital for maintaining the integrity of the ocular surface” explained Dr Tan-Showyin. “Therefore, in dry eye, promoting tear retention at the ocular surface is important for increasing tear film thickness, protecting the ocular surface from desiccation, and relieving symptoms of discomfort.7
“ This is the first study to demonstrate conclusively that dry eye is associated with reduced mental HR-QoL5 ”
“However, paradoxically, instillation of topical tear supplements generally initiates reflex tears and reflex blinking, all of which act to remove the instilled solution from the ocular surface. Measurable effects on clinical properties of the tear film after eye drop instillation have been shown to dissipate after as little as 15 minutes.4
“Increasing retention time of lubricating eye drops on the ocular surface is important, particularly given the inconvenience of having to instill eye drops multiple times daily. In other cases, it is simply impractical or impossible to administer drops frequently, such as in the example of a friend who is a surgeon and suffers terribly from dry eye. Instillation of eye drops is simply not possible during hours-long surgical procedures, and the associated discomfort and visual disturbance that arises affects his ability to perform his critical job.
“Eye drops with high viscosity can increase retention time on the ocular surface but may also cause transient visual disturbances and result in unwanted debris on the eyelids and lashes.7 Therefore, the highest viscosity eye drops are typically recommended for nighttime use only. During the day, it is a balance to try to maximise the retention time on the ocular surface for lubrication and health benefits versus inducing unwelcome side effects.
“Retention time of eye drops can be measured by simply evaluating ocular signs and symptoms at set timepoints following administration of treatment, or other more sophisticated techniques such as fluorophotometry can be used,” Dr Tan-Showyin said.
Fluorophotometry describes a method whereby a fluorescently labelled macromolecule (70,000 molecular weight FITC dextran) is admixed with the ophthalmic formulation. When used in modest amounts, the fluorescent tracer does not measurably alter formulation viscosity or penetrate corneal tissue. This technique allows characterisation of the retention time of formulations to be measured on eye and has been used to successfully differentiate between the residence time of polyethylene glycol, carboxymethylcellulose, and hydroxypropyl methylcellulose based artificial tears in dry eye subjects.8
“The aforementioned study concluded that precorneal residence time is influenced by factors other than simple viscosity and recommended that the interplay of other characteristics should be examined to determine the effects on formulation retention,” said Dr Tan-Showyin.
“The fluorophotometer has been used to examine the retention time of saline versus various artificial tear formulations, but no
“ the viscosity of commercial eye drops differs considerably due to the use of hyaluronic acid in a broad range of molecular weights9 ”
studies to date have evaluated the retention time on the ocular surface of lubricating eye drops containing various concentrations of hyaluronic acid,” Dr Tan-Showyin said.
HYALURONIC ACID
Dr Tan-Showyin said hyaluronic acid (HA), also known as hyaluron and sodium hyaluronate, is of interest to eye care professionals because, as a naturally occurring glycosaminoglycan, it is found in the tear fluid, lacrimal glands, conjunctiva and corneal epithelium, and plays a structural role in the interior, anterior, and posterior segments of the eye. 9
“It is produced by corneal epithelial cells and keratocytes in the eye and is known to be one of the factors that promotes healing of corneal injuries.10 Its concentration increases in response to ocular damage and in vitro, hyaluronate promotes cell migration and ocular surface epithelial repair. 11
“In fact, hyaluronic acid has been shown to promote corneal epithelial healing in patients with dry eye after 28 days of treatment.12,13 However, the concentration of hyaluronic acid in tears of patients with dry eye is not significantly changed,” 9 she said.
“Hyaluronic acid has water retentive properties, and in vitro, has been shown to retard water loss in a dose dependent manner, which is expected to improve corneal wettability.14 The biological functions of hyaluronic acid are molecular weight dependent, where high molecular weight hyaluronic acid is involved in anti-inflammatory processes and wound regeneration, whereas fragmented hyaluronic acid triggers inflammatory processes.” 9
Dr Tan-Showyin said the physicochemical properties of formulations containing hyaluronic acid are influenced by concentration, molecular weight, and chemical structure.
“The viscoelastic properties affect the residence time on the eye, and therefore the efficiency. However, the viscosity of commercial eye drops differs considerably due to the use of hyaluronic acid in a broad range of molecular weights. Furthermore, other ingredients in the formulation may change the viscosity, including osmotic pressure regulators, salts, and pH, and therefore, it is difficult to predict the efficacy based on physicochemical properties.9
“Additionally, high viscosity at rest and low tear viscosity during blinking are required to prevent excessive shear stress on the ocular epithelium.9 Hyaluronic acid exhibits non-Newtonian shear-thinning properties, where viscosity decreases with increasing shear rate,” 7 Dr Tan-Showyin explained.
She said the demonstrated clinical benefits of hyaluronic acid include increased tear breakup time and reduced symptoms of ocular irritation associated with dry eye.15
“The use of eye drops containing hyaluronic acid is gaining more attention given its wound healing properties, ability to bind to the ocular surface, and efficacy for alleviating dry eye symptoms and promoting tear film stability. Furthermore, eye drops combining hyaluronic acid and other polymers may provide synergistic benefits in enhancing ocular surface hydration and reducing friction.”
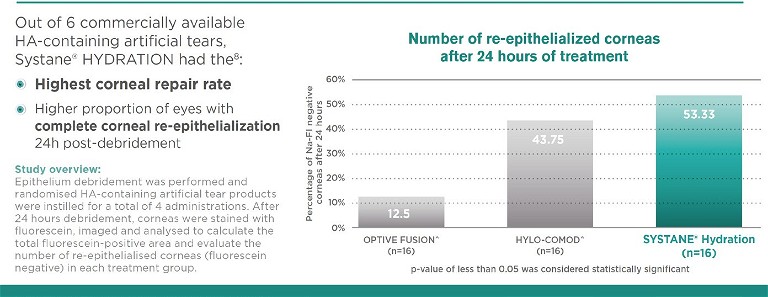
Figure 1. Systane Hydration showed faster ocular re-epithelialisation compared with other HA-containing drops.
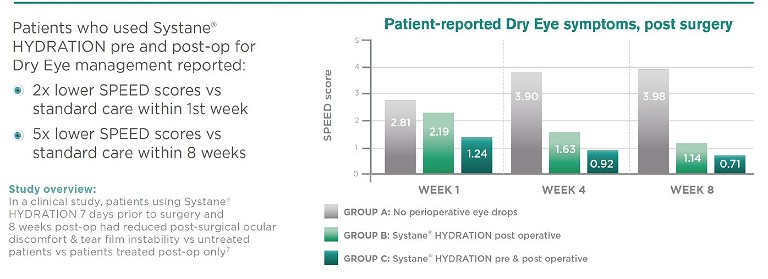
Figure 2. Systane Hydration reduces patient-reported dry eye symptoms post-surgery.
“ The use of eye drops containing hyaluronic acid is gaining more attention given its wound healing properties... ”
EFFECT ON RE-EPITHELIALISATION
Systane Hydration lubricant eye drops combine HA* with Alcon’s unique formulation of HP-guar and borate to increase retention of the active ingredients on the eye for longlasting dry eye relief (Figure 3). 16-18
Systane Hydration has been investigated in numerous studies: it has been shown to support healing of the damaged ocular surface, assisting cell viability, and regeneration.16,19 The combination of HA and HP-guar /borate resulted in greater and faster wound healing (measured in reepithelialisation) compared with HA alone in a laboratory study. 19 The investigators looked at the effect on re-epithelialisation of a corneal debridement wound following topical ocular administration of six different lubricating eye drops in mice. Following debridement, test solutions were administered every two hours for a total of four administrations. To evaluate the number of re-epithelialised corneas in each treatment group, the corneas were stained with sodium fluorescein 24 hours after debridement. The stained corneas were imaged and analysed to calculate the total damaged area still visible. The percentage of eyes displaying negative staining was significantly higher with Systane Hydration versus the other drops, including drops containing HA alone (Figure 1). 19
USE AFTER SURGERY
Dry eye is a significant factor in patient satisfaction and outcomes following ocular surgery. Approximately 82% of patients experience moderate-to-severe dry eye symptoms following cataract surgery 20 and 50% of patients experience dry eye post laser-assisted in situ keratomileusis (LASIK). 21 Peri-operative management of existing dry eye can reduce post-operative dry eye symptoms and may influence post-operative outcomes. 22,23
The effect of Systane Hydration in perioperative management plans for dry eye sufferers was investigated by Favuzza et al., across 17 centres in Italy.22
The data of 419 patients not previously affected by DED, who had undergone cataract surgery in one eye, was reviewed retrospectively. The patients were included in three different groups according to their use of ocular lubricants pre- and post- surgery. Group A consisted of patients who had instilled the HP-guar/HA solution (Systane Hydration) three times per day for one week pre-operatively and for two months postoperatively. Group B instilled HP-guar/HA (Systane Hydration) for two months postoperatively only. Group C did not instil any artificial tears pre- or post-surgery.
All patients followed the same antibiotic and anti-inflammatory post-operative topical regimen. Dry eye was evaluated through tear break-up time and corneal fluorescein staining, and the Standardised Patient Evaluation of Eye Dryness (SPEED) questionnaire. The SPEED questionnaire is comprised of eight questions to evaluate both the frequency and severity of symptoms. The patient grades the severity of symptoms on a scale of zero to four, with zero being no symptoms and four being intolerable symptoms. The numeric value for each answer is added with scores ranging from zero to 28. The tests were performed at the pre-operative visit and then post-operatively at weeks one, four, and eight.22
Tear break-up time and corneal staining were significantly lower in Groups A and B compared with Group C in the post-operative period. With the use of lubricating eye drops both before and after surgery, Group A showed significantly lower SPEED scores even compared with Group B at both one week postoperatively and one month post-operatively. The study concluded that the use of the HPguar/HA solution was effective at reducing post-cataract surgery ocular discomfort and tear instability, particularly if also instilled in the preoperative period22 (Figure 2).
Therefore, with its support of the natural healing process, Systane Hydration can be recommended to patients with moderate-tosevere dry eye symptoms# and also who are pre- and post-ocular surgery. 22
WATCH THIS SPACE
The Systane Hydration formulation has been available as preservative-free in single dose vials in Australia and New Zealand for some time. In September 2023 it was launched in the PureFlow multi-dose preservative-free bottle used in Systane Complete Preservative-Free and Systane Ultra Preservative-Free. The bottle has a one-way valve to ensure no contaminated liquid can be re-introduced into the container and a fine silicone membrane to filter returned air.24 The bottle has a low squeeze force for easy dispensing of the drops and features a blue tip to aid targeting of the eye for ease of installation (Figure 4). 24
Figure 3. Hyaluronic acid and hydroxypropyl-guar (HP-guar).

Figure 4. Eye drop instillation.
As there had been no studies to date evaluating the retention time on the ocular surface of lubricating eye drops containing various concentrations of hyaluronic acid, Dr Tan-Showyin conducted research in this area, and the results are planned to be published in late 2023.
“My research team conducted a randomised, double-masked comparison of three eye drops containing different concentrations of hyaluronic acid, to compare retention times on the ocular surface using a fluorophotometer.
“In brief, the fluorophotometer consists of a high-resolution camera attached to a slitlamp biomicroscope, with custom excitation and emission filters. By obtaining repeated scans of the ocular surface following eye drop instillation, characterisation of the retention time of various lubricating eye drop formulations can be evaluated.
“Adult participants with symptomatic dry eye (Ocular Surface Disease Index score >12)25 were required to attend three separate visits at approximately the same time of day, on three separate days separated by a minimum of two and a maximum of seven days.
“Following measurement of baseline fluorescence of the eye, a controlled volume of the randomly allocated eye drop admixed with the fluorescent tracer was instilled in the eye. Fluorophotometry scans were taken every 30 seconds for the first eight minutes, followed by measurements every two minutes until the fluorescence values had returned to baseline levels. Participants were instructed not to instill any other eye drops within 24 hours of each study visit and all participants were required to undergo evaluation with all of the three study eye drops.
“The eye drop formulations evaluated in the study included 0.15% sodium hyaluronate / 0.175% HP-guar, 0.2% sodium hyaluronate and 0.1% sodium hyaluronate. Significant differences were found in the retention time of the eye drops, which were related to the concentration of sodium hyaluronate in the formulation.
“But,” Dr Tan-Showyin said, “you’ll need to watch this space to find out which formulation outperformed the others.”
*Systane Hydration lubricant eye drops contain sodium hyaluronate, the salt form of hyaluronic acid.
#Recommendation based upon expected on-eye viscosity.
Disclosure: This article was sponsored by Alcon Laboratories Pty Ltd. Helen Gleave is employed by Alcon. ANZ-SYY-2300056
To earn your CPD hours visit mieducation.com/making-dry-eye-management-stick.
References
1. Craig, J.P., et al., TFOS DEWS II report executive summary. Ocul Surf, 2017. 15(4): p. 802–812.
2. Stapleton, F., et al., TFOS DEWS II epidemiology report. Ocul Surf, 2017. 15(3): p. 334–365.
3. Semp, D.A., Beeson, D., Sheppard, A.L., et al., Artificial tears: A systematic review. Clin Optom (Auckl). 2023 Jan 10;15:9–27.
4. Markoulli, M., et al., The effect of optive and optive advanced artificial tears on the healthy tear film. Curr Eye Res, 2018. 43(5): p. 588–594.
5. Morthen, M.K., Magno, M.S., Uthiem, T.P., et al. The physical and mental burden of dry eye disease: A large population-based study investigating the relationship with health-related quality of life and its determinants. Ocul Surf 2021; 21: 107–117.
6. Craig, J.P., et al., TFOS DEWS II definition and classification report. Ocul Surf, 2017. 15(3): p. 276–283.
7. Jones, L., et al., TFOS DEWS II management and therapy report. Ocul Surf, 2017. 15(3): p. 575–628.
8. Paugh, J.R., et al., Precorneal residence time of artificial tears measured in dry eye subjects. Optom Vis Sci, 2008. 85(8): p. 725–31.
9. Huerta-Angeles, G., Nesporova, K., Hyaluronan and its derivatives for ophthalmology: Recent advances and future perspectives. Carbohydr Polym, 2021. 259: p. 117697.
10. Toshida, H., et al., The effects of vitamin A compounds on hyaluronic acid released from cultured rabbit corneal epithelial cells and keratocytes. J Nutr Sci Vitaminol (Tokyo), 2012. 58(4): p. 223–9.
11. Aragona, P., et al., Long term treatment with sodium hyaluronate-containing artificial tears reduces ocular surface damage in patients with dry eye. Br J Ophthalmol, 2002. 86(2): p. 181–4.
12. Papa, V., et al., Comparison of hypotonic and isotonic solutions containing sodium hyaluronate on the symptomatic treatment of dry eye patients. Ophthalmologica, 2001. 215(2): p. 124–7.
13. Condon, P.I., et al., Double blind, randomised, placebo controlled, crossover, multicentre study to determine the efficacy of a 0.1% (w/v) sodium hyaluronate solution (Fermavisc) in the treatment of dry eye syndrome. Br J Ophthalmol, 1999. 83(10): p. 1121–4.
14. Nakamura, M., et al., Characterization of water retentive properties of hyaluronan. Cornea, 1993. 12(5): p. 433–6.14.
15. Johnson, M.E., Murphy, P.J., Boulton, M., Effectiveness of sodium hyaluronate eyedrops in the treatment of dry eye. Graefes Arch Clin Exp Ophthalmol, 2006. 244(1): p. 109–12.
16. Rangarajan, R., Kraybill, B., Ogundele, A., Ketelson, H., Effects of a hyaluronic acid/hydroxypropyl guar artificial tear solution on protection, recovery, and lubricity in models of corneal epithelium. J Ocul Pharmacol Ther. 2015;31(8):491–497.
17. Davitt, W.F., Bloomenstein, M., Christensen, M., Martin, A.E., Efficacy in patients with dry eye after treatment with a new lubricant eye drop formulation. J Ocul Pharmacol Ther. 2010;26(4):347–353.
18. Rolando, M., Autori, S., Badino, F., Barabino, S., Protecting the ocular surface and improving the quality of life of dry eye patients: a study of the efficacy of an HP-guar containing ocular lubricant in a population of dry eye patients. J Ocul Pharmacol Ther. 2009 Jun;25(3):271–8. doi: 10.1089/jop.2008.0026. PMID: 19366323.
19. Carlson, E., Kao, W.W.Y., Ogundele, A., Impact of hyaluronic acid-containing artificial tear products on reepithelialization in an in vivo corneal wound model. J Ocul Pharmacol Ther. 2018;34(4)360–364.
20. Jayshree, M. et al. A prospective study of dry eye after small incision cataract surgery in rural population of Bagalkot. J Clin Res Ophthalmol 2017;4(2):25–29.
21. Toda, I., Dry eye after LASIK. Invest Ophthalmol Vis Sci. 2018;59(14):DES109-DES115. doi:10.1167/iovs.17-23538.
22. Favuzza, E., Cennamo, M., Vicchio, L., et al., Protecting the ocular surface in cataract surgery: The efficacy of the perioperative use of a hydroxypropyl guar and hyaluronic acid ophthalmic solution. Clin Ophthalmol 2020 Jun 26;14:1769–1775.
23. Chuang, J. et al., Preoperative optimization of ocular surface disease before cataract surgery. J Cataract Refract Surg 2017;43(12):1596–607.
24. Nemera Novelia Product Leaflet, 2015. Available at nemera.net/wp-content/uploads/2014/06/Brochure_ Ophthalmic.pdf [Accessed 23 Jul 2021]. 25. Miller, K.L., et al., Minimal clinically important difference for the ocular surface disease index. Arch Ophthalmol, 2010. 128(1): p. 94–101.

Helen Gleave BScOpt (Hons) MCOptom is the Senior Professional Education and Development Manager at Alcon. She is responsible for training and education programs in contact lenses, contact lens care, and dry eye, including Alcon Dry Eye Academy and Dry Eye Academy Online. She has delivered education to a broad range of audiences, and spoken at numerous optometry conferences, educational events and webinars across Australia and New Zealand.