miophthalmology
Myopia: The Continuing Pathology
WRITER Dr Craig Donaldson AM
Far from being just a condition impacting children, myopia is a complex common condition that has many associated pathologies that can progress throughout a person’s life. In this article, Dr Craig Donaldson provides a comprehensive review.

“ It is established that myopia is linked with environmental factors as well as a person’s genetic background ”
Ocular pathology associated with myopia can take many forms and can continue to develop throughout a person’s life. The global incidence of myopia has increased dramatically over the past 20 years and children appear to be developing myopia at an earlier age.1-5 The incidence of myopia varies depending on age, sex, race, existence of parental myopia, and geographical location.6-10 Not only has this been recorded in children, but in contrast to the perception that myopia stabilises around age 15, myopia can also arise and worsen in young1 and middle-aged adults.7 A landmark paper in the 1960s11 observed that myopia can develop after the teenage years. Numerous studies have documented progression of existing myopia as well as the development of new myopia in adulthood.12-16 A recent prospective single centre study reported a myopic shift of 0.5D in at least one eye in 37.8% of 20-yearolds studied over an eight-year period.1 The reasons behind this increase are thought to include time spent indoors, use of electronic devices, change in diet, obesity, onset of puberty, and sedentary lifestyles.16-26
It is established that myopia is linked with environmental factors as well as a person’s genetic background.27-31 Thus far more than 200 genes have been linked to myopia. High myopia has been inherited in Mendelian patterns including autosomal dominant, autosomal recessive, and X-linked (Figure 1). Numerous conditions, including Stickler syndrome, Marfan syndrome, Ehlers-Danlos, and ocular albinism are associated with myopia and high myopia.
Although the prevalence of myopia is presently relatively low in middle-aged Australian adults,13 this is expected to rise significantly as the younger generations age. With the increasing prevalence of myopia beyond childhood, an increase in myopia induced ocular pathology may be expected. This is important because of both the burden associated with refractive error and the various and significant ocular pathologies known to be associated with myopia. These include – but are not limited to – amblyopia, strabismus, glaucoma, cataract, retinal tear and detachment, myopic macular degeneration and choroidal neovascular membrane formation, and staphyloma.
It is important to differentiate between high myopia and pathologic myopia. These two entities are often confused. High myopia, by definition, is a myopic refraction of greater than or equal to six dioptres and/or an axial length of 26.5 mm or more. Pathologic myopia can be defined as axial elongation of the globe associated with degenerative structural changes to the globe. These changes include posterior staphyloma, myopic maculopathy, and high myopia-associated optic neuropathy. Pathologic myopia affects approximately 1% of the Caucasian and 3% of the Asian population.32 Pathologic myopia is a major cause of low vision in adult populations around the world.33-37

Figure 1: Twin sisters with myopia.
Critically, pathologic myopia is not limited to patients with high myopia and indeed can be found in lower levels. However, the likelihood of developing pathologic myopia increases with decreasing spherical equivalent. Although pathologic myopia can still occur with low to moderate myopia up to three dioptres, the prevalence is 50–70% in high myopes38-39 and patients with more than 7.00D of myopia are at a very much greater risk.40 The higher the prevalence of myopia in a population, the higher the prevalence of high myopia.41 With an increasing prevalence of myopia, it can be expected that the prevalence of high myopia and thus the incidence of pathologic myopia will increase in the future. Not only will this provide a greater disease burden but also a financial burden on the individual and society. It was estimated in 2015 that the global financial burden of myopia through loss of productivity alone was US$250 billion.42
It is becoming increasingly apparent that myopia is a major public health concern and that educating the population that myopia management does not stop in childhood should be given priority. Indeed, it is essential to educate patients and health professionals that ongoing review and comprehensive care continues throughout life.
PATHOLOGIES ASSOCIATED WITH MYOPIA AND HIGH MYOPIA
High myopia in childhood is less frequent and more commonly associated with secondary and genetic causes (Figures 2 and 3). As a result of this there is a need to consider the possibility of systemic conditions. Additionally in very young children, the presence of myopia and even high myopia may not be obvious, and the diagnosis only made when the child gets older. Sometimes the first notion a child has difficulty seeing is by them not engaging normally with people and their surroundings. In essence they may become ‘visually isolated’ as they are unable to engage with people and their environment due to the inability to perceive faces, others’ emotions, and everyday objects.

Figure 2: A child with high myopia.
Figure 3. A teenager with high myopia.
Amblyopia
Refractive amblyopia can arise from hypermetropia, astigmatism, and myopia. The global prevalence of amblyopia has been cited to be around 1.75%43 with anisometropia the most common cause. The Gutenberg Health Study from Germany, that included 15,010 participants aged between 35 and 74 years of age with five years follow-up, found that in cases of low vision, amblyopia was present in 44.1%, high myopia in 14.7%, and genetic diseases in 5.9%.44
Amblyopia can occur with 5.0–6.0D or more of bilateral myopia and anisomyopia of approximately 3.0–4.0D.45 Some children present with marked myopic anisometropia without any apparent underlying cause. Unilateral cases are usually diagnosed later as there are often no obvious visual clues that the child cannot see normally from each eye, and the child may accept the reduced vison in one eye as normal.
It is important to rule out underlying pathology and this should include assessment for corneal and lens pathology as well as intraocular pressure, assessment of the optic discs, axial length measurement, and B scan for posterior staphyloma. Glaucoma in children under the age of approximately two years can cause axial lengthening and progressive myopia. Importantly, in those children the intraocular pressure may ‘measure’ as normal while the globe and the optic disc cup are enlarging in order to accommodate the ocular hypertension. Myopic maculopathy does occur in children and retinal optical coherence tomography (OCT) is indicated. Children under 18 years of age with high myopia have a relatively high risk of maculopathy, most often in the form of diffuse atrophy. Ongoing monitoring is essential. One study found progression of myopic maculopathy in 12% of 548 paediatric high myopes followed over four years.46
“ … children with intermittent exotropia are much more likely to become myopic with one study finding a 90% chance of myopia occurring by 20 years of age ”
The management of amblyopia associated with myopia includes refractive correction and in unilateral cases, penalisation of the better eye. High levels of anisomyopic amblyopia are often more difficult to treat, perhaps owing to later diagnosis and other factors such as the child resisting spectacle wear. Contact lenses can be beneficial and kept in mind for the appropriate child.
Strabismus
Myopia is associated with many different forms of strabismus. High myopia has an increased risk of esotropia and vertical tropias.
Intermittent Exotropia
The Sydney Myopia Study found that 25% of children with myopia had strabismus compared to 1.9% of emmetropes and 4.3% of hyperopes. Most of these cases among the myopic children were intermittent exotropia and the risk increased with early onset of refractive error.47
Additionally, from another perspective, children with intermittent exotropia are much more likely to become myopic, with one study finding a 90% chance of myopia occurring by 20 years of age.48 The exact relationship between myopia and intermittent exotropia is not clear. Traditionally, the increased incidence of intermittent exotropia among myopes has been thought to result from the reduced need for accommodation and thus convergence.
More recently the question has once again been raised as to whether the practice of overminusing therapy for intermittent exotropia is associated with a greater risk of myopia. Previous studies have not shown any increased risk of myopic progression,49-50 but more recent research has shown that over-minusing increases the risk of myopic shift.51-52
Heavy Eye and Sagging Eye Syndrome
Two conditions deserve special mention because they are intrinsically linked to myopia. With progressive axial elongation, strabismus may arise due to disruption of the normal mechanics of ocular motility. Heavy eye syndrome (myopic strabismus fixus) occurs in high myopia when the axial length of the globe is so long that there is superolateral dislocation of the globe between the superior and lateral recti muscles and displacement of these muscles medially and inferiorly respectively. Typically, there is a progressive esotropia and hypotropia with limited abduction and supraduction. Normalisation of eye movements can be achieved by posterior suture anastomosis of the superior and lateral rectus ( Yokoyama suture).53-54
Sagging eye syndrome has less displacement of the lateral rectus and superior rectus and affected patients typically display an esotropia for distance with often a small vertical component. Importantly, abduction is intact and can be treated with conventional resection/ recession surgery. Magnetic resonance imaging (MRI) of the orbits and ocular muscles is very useful in differentiating these two entities (Figure 4).
MYOPIA OF PREMATURITY
Myopia of prematurity (MOP) is linked to retinopathy of prematurity and its treatment but can also occur without retinopathy. Myopia of prematurity is not generally associated with an increased axial length but rather, patients with MOP display abnormal anterior segments with increased corneal curvature and lenticular thickening.55 The exact mechanism of MOP remains unknown, however the chance of myopia and high myopia increases with worsening retinopathy and the modality of therapy. The BEAT-ROP study that compared laser with intravitreal bevacizumab (IVB) showed an increased risk of myopia (79% /43%) and high myopia (50%/22%) after 2.5 years follow-up.56 The risk of developing myopia increased with the number of laser shots applied. Furthermore, cryotherapy results in a higher incidence of MOP than laser.57
Prematurely born children need to be monitored for refractive error and amblyopia. The greatest myopic shift tends to happen in the first year of life but can continue for several years.58
SYNDROMES
Numerous systemic syndromes are associated with myopia and high myopia. Genetic testing is available for Stickler syndrome, a multiorgan disorder that is usually inherited as an autosomal dominant condition secondary to collagen gene mutation and abnormal connective tissue formation. It is relatively common with a prevalence of approximately 1:5,000 births and it is thought to be highly underdiagnosed.59 The ocular findings include high myopia, cataract, retinal detachment, giant retinal tear, and proliferative vitreoretinopathy. It is a significant cause of retinal blindness in children and this risk of retinal pathology continues into adulthood. Systemic associations are variable and include cleft palate, malar hypoplasia, flat nasal bridge, small jaw, hearing loss, joint and skeletal abnormalities, and mitral valve prolapse.
Eye care health professionals should be aware of this syndrome and give consideration to it when encountering young patients with severe myopia. Affected patients require lifelong surveillance due to the increased risk of ocular abnormalities and a thorough annual assessment with dilated fundal examination is recommended.
Marfan syndrome (MFS) is another multisystem genetic disorder due to an inherited abnormality of the fibrillin-1 (FBN1) gene. Genetic testing is available for MFS. About 75% of cases are autosomal dominant and 25% due to new mutation. The prevalence is also estimated to be around 1:5,000 and, like Stickler syndrome, it is not rare. Affected individuals are most likely to have the ocular, skeletal, and cardiovascular systems affected.
Typically, people with MFS are of above average height, have long slender limbs and digits, and have joint hypermobility. Scoliosis of the spine is common. Approximately 60% of cases have lens subluxation due to zonular weakness and myopia and high myopia with axial lengthening is common. Other ocular associations include cataract, glaucoma, and retinal detachment. Affected patients are prone to serious cardiovascular disorders such as abdominal aortic aneurysm, aortic dissection, and valvular degeneration.
Myopia in a child may be the first sign of MFS as the other associations may not become apparent until later years.60 Just under half of MFS patients may be diagnosed following ocular complaints.61 It is important to consider the possibility of MFS, especially with a family history, as there is a substantial risk of ocular and systemic morbidity. Careful dilated examination for lens subluxation is critical. Early cardiac screening in affected patients is essential. Lifelong annual review with dilation is reasonable.
GLAUCOMA
Numerous studies have established that myopia carries an increased risk of developing glaucoma.62-66 The Blue Mountains Eye Study, a cross-sectional population-based study of 3,654 Australians aged between 49 and 97 years of age demonstrated a strong relationship between myopia and glaucoma.62 In this study glaucoma was found to be almost 2.3–3.3 times more likely to occur in patients with any form of myopia. There is evidence to suggest that with increasing axial length, the risk of glaucoma increases. A meta-analysis of 24 studies found an overall approximate 20% increase in glaucoma risk for each 1D increase in myopia.67
Of interest, there is also evidence that intraocular pressure (IOP) in children may be higher in myopic than non-myopic eyes.68-69
The reason for the increased risk of glaucoma in myopia is incompletely understood. Theories include peripapillary anatomic changes, retinal ganglion cell mechanical stretching, and possibly optic nerve damage during eye movements with an elongated globe.
In myopia, the optic disc can appear atypical and visual field defects can occur that simulate glaucoma (Figure 5). This can lead to a diagnostic dilemma, particularly differentiating myopia from normal tension glaucoma.70 Both conditions can co-exist, and normal tension glaucoma is more common in high myopia.71 Regular ongoing review of the patient with myopia is essential. Baseline optic nerve and macular optical coherence tomography (OCT) and visual field assessments are strongly recommended.
RETINAL DETACHMENT
Myopia raises the risk of rhegmatogenous retinal detachment (RRD). All levels of short sightedness have a greater risk of RRD compared with emmetropes and this increases with increasing myopia. In approximate terms of spherical equivalent (SE), -1.00D to3.00D have a four times risk, and less than -3.00D a 10 times risk, and -5.00D or less a 20 times increased risk of RRD.72-73 Additionally, the risk of RRD after cataract surgery rises in relationship to spherical equivalence (SE) and axial length.
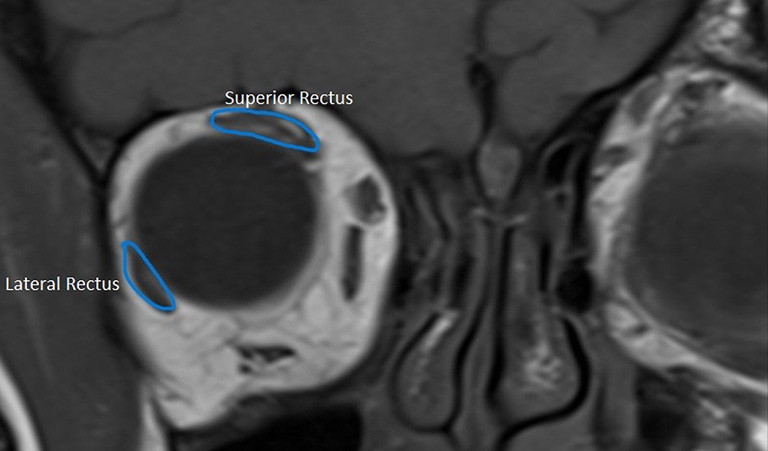
Figure 4. Heavy eye muscle displacement as shown on MRI. Image courtesy Dr Lionel Kowal.
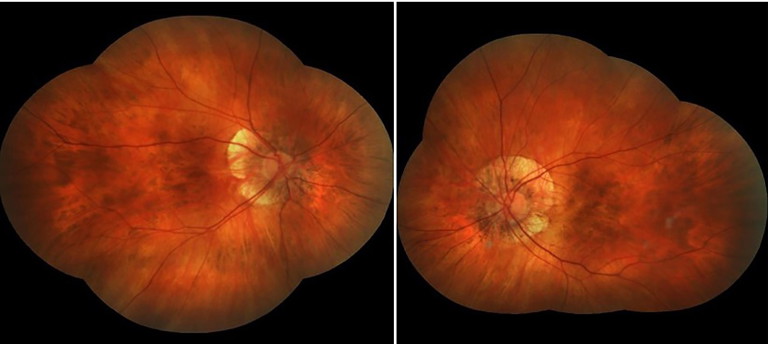
Figure 5. Myopic fundi atypical discs.
The reasons behind this increase in RRD are considered to include retinal thinning with increased axial length, vitreous liquefaction with posterior detachment happening at an earlier age in myopes,74 as well as an increased incidence of peripheral retinal pathology and posterior staphylomata. An increase in RRD incidence has been recorded over the past two decades and this would appear to correlate with an increasing prevalence and severity of myopia.75-78
Myopic patients need to be educated regarding the symptoms of retinal tears and detachment and the need for urgent review if these should occur. Additionally, retinal detachments can occur in children, especially those with high myopia and they may not convey changes to their vision. Annual retinal review of myopic patients of all ages, particularly highly myopic patients, is recommended.
MYOPIC MACULOPATHY
High myopia (> -6.00DS) and less commonly, less severe myopia,40,79 can result in structural changes at the macula. These changes include staphyloma, macular atrophy, lacquer cracks, posterior pole retinal detachment, and choroidal neovascularisation (CNV ), which can lead to disciform scar (Fuchs spot). A tessellated fundus (Figure 6) results from thinning of the retinal pigment epithelium and prominence of the choroidal vasculature. With progressive atrophy, yellowish/white areas appear around the optic disc and macular, and there is an associated risk of CNV. Lacquer cracks that appear to be due to stretching of layers of the globe signify breaks of the retinal pigment epithelium, Bruch’s membrane, and choriocapillaris complex. They are also linked with a greater risk of myopic neovascularisation (Figure 7). About 10% of patients with myopic maculopathy will develop
CNV over 10 years.80 Patients with myopic CNV in one eye have a high risk of the fellow eye being affected. One study put the risk at 35% over an eight-year period.80 Depending on the severity of findings, patients displaying any level of maculopathy require six to 12 monthly retinal review with OCT imaging and possible ophthalmic review. Patients should self-monitor with an Amsler grid and receive education regarding the need for urgent review with visual alteration such as metamorphopsia.
Treatment firstly includes prevention of high myopia through arrest of myopia progression. It has been estimated that slowing the progression of myopia by 1.00D will reduce the likelihood of myopic maculopathy by 37%.81
Anti-vascular endothelial growth factor (antiVEGF) agents are used as first line therapy in the management of CNV and have been shown to improve vision in affected patients although macular atrophy remains a problem. A recent meta-analysis of 34 studies82 found that intravitreal anti-VEGF on a one plus as needed (1+prn) treatment regimen was effective in improving visual outcomes. In contrast to age-related macular degeneration, fewer injections are generally needed.
CATARACT
Myopia is an established risk factor for cataract formation,83-84 especially nuclear sclerosis and posterior subcapsular types. The Singapore Malay Eye Study of 3,280 adults of Malay ethnicity aged between 40 and 80 years found that myopia, rather than axial length, was linked to nuclear cataract formation. This may however reflect myopia secondary to cataract formation.83 Regardless, highly myopic eyes develop cataract about 10 years younger than normal eyes.85-86 Onset of myopia before the age of 20 may be a strong and independent risk factor of posterior subcapsular cataract formation.87 Possible explanations for development of cataracts in myopia include genetic predisposition, environmental factors, oxidative stress secondary to early vitreous liquefaction, and enrichment of growth factors (e.g. transforming growth factor-beta 1).88
Cataract surgery in highly myopic eyes has been shown to have an increased rate of complications. These include retinal detachment, IOP rise, posterior capsule rupture, capsule contraction syndrome, and progression of maculopathy.89-90 Third generation intraocular lens power measurement formulas have resulted in less frequent post-operative refractive surprises.
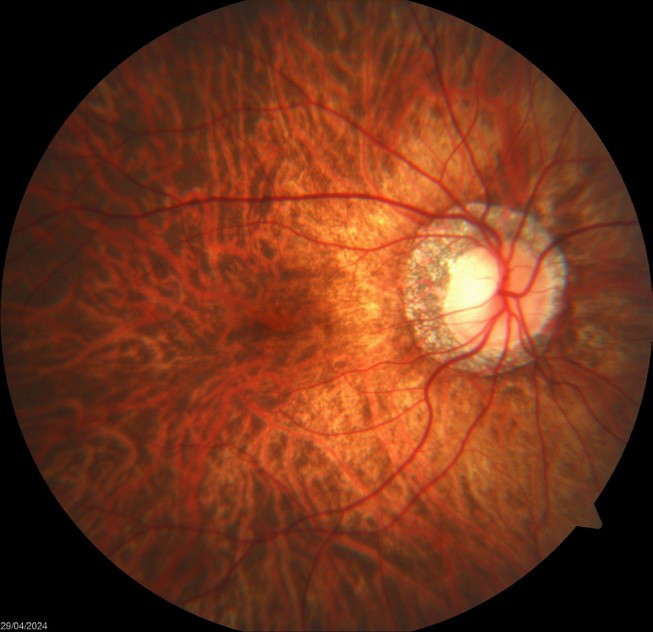
Figure 6. Tesselated fundus and atypical disc.

Figure 7. Patchy chorioretinal atrophy and lacquer cracks.
ARTIFICIAL INTELLIGENCE
Artificial intelligence (AI) is being developed as a mode of detecting those patients at risk of myopia and high myopia.91-93 Primarily this utilises OCT and fundus images. As well, AI algorithms have been found to help in both the diagnosis and risk of development of pathologic myopia and related complications.94 Furthermore, a recent meta-analysis in 2024, comprising 11 studies including 165,787 eyes,95 found that AI-based diagnostic tools using colour fundus photographs are a highly specific and sensitive (pooled 96.5% and 95.9% respectively) modality for the detection of pathologic myopia. It is most likely that in the future, AI will become important in the tailoring of myopia management therapy.
SUMMARY
Numerous ocular pathologies, as outlined above, are associated with myopia. In contrast to the former belief that myopia is a condition that occurs in young people running an inexorable course, we now know better. New treatment modalities are available and continue to be refined. Myopia is a complex common condition that has many associated pathologies that can progress throughout a person’s life. These pathologies are visually debilitating and remain a common cause of reduced vision and morbidity.
Eye care health professionals must be aware of these pathologies and the need for regular routine review. Public education should become a fundamental practice to propagate the general awareness of the possibility of myopia therapy and the need for regular review throughout life, especially for those at risk of pathological changes.
To earn your CPD hours from this article, visit mieducation.com/myopia-the-continuing-pathology.
Dr Craig Donaldson AM MB BS FRANZCO FRACS is Head of the Strabismus (ocular misalignment) and Paediatric Ophthalmology Unit at Sydney Eye Hospital and is a Visiting Medical Officer at Sydney Children’s Hospital and a senior staff specialist at The Children’s Hospital at Westmead. He operates privately at Epping Surgery Centre in Sydney.
Dr Donaldson has an interest in general ophthalmology with particular expertise in the management of cataract, strabismus, and paediatric eye disease. He has authored many papers and presented at numerous Australian and overseas conferences to ophthalmologists, orthoptists, optometrists, and ophthalmic nurses.
In 2019 he was recognised for his services to medicine and ophthalmology in Australia and overseas by receiving a Member of the Order of Australia.
References available at mieducation.com