mitechnology
SPONSORED CONTENT
Intravitreal Injections: Building Sustainability into Disease Treatment
WRITER Dr Sam Evans
Cross-sectional illustration of an intravitreal injection using the SP. Eye.
The SP.Eye’s intravitreal injection device reduces the carbon footprint of intravitreal injections and improves models of ophthalmic care in remote regions, writes inventor, Dr Sam Evans.
Intravitreal injections are a vital treatment for various sight-threatening conditions, such as age-related macular degeneration (AMD) and diabetic retinopathy. Around 900,000 intravitreal injections are delivered in Australia/New Zealand each year, a number that continues to grow.1
The carbon footprint of traditional intravitreal injections is approaching 12,300 tonnes/ year (equivalent to driving a petrol-powered car over 50 million kilometres).2 Ninety-five per cent of this footprint is due to patients travelling to appointments (76%) and the disposable intravitreal pack (18.5%).2
The SP.Eye is a relatively new intravitreal injecting device in Australia and New Zealand that can significantly improve this footprint, both by reducing or even removing the need for a disposable pack, and by enabling intravitreal injections to be delivered by nonspecialists outside the clinic. This will reduce the need for patient travel, particularly in regional and remote areas where the barriers to treatment are further compounded by a shortage of treating ophthalmologists.
REDUCING THE IMPACT OF TRANSPORTATION
Traditional intravitreal packs include many single use items: callipers, gallipots, Rampley forceps, a speculum etc., each of which adds carbon in manufacture and transportation.
Injectors using SP.Eye do not need a drape, speculum or calliper. Some injectors prepare the area simply by holding a sterile gauze soaked in Betadine, and using topical anaesthesia and Betadine to prepare the globe and adnexa without using Rampley forceps. Using this approach, there is no need for any intravitreal pack whatsoever.
This significantly reduces the carbon footprint associated with transportation of injection-related items to healthcare facilities. If SP.Eye injecting was adopted across Australia and New Zealand, from calculations based on published rates, it could achieve a saving of 2,300 tonnes per year of CO2 .2
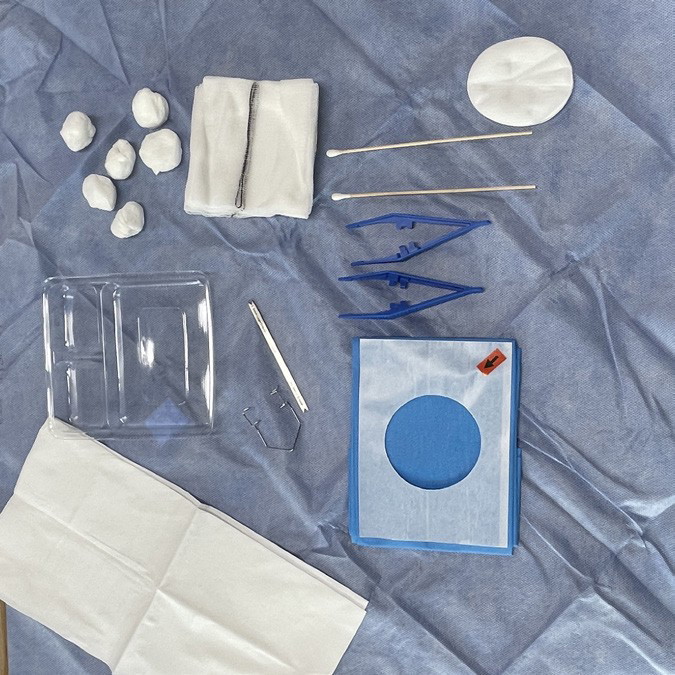
Contents of a traditional intravitreal pack.

Contents of the SP.Eye intravitreal injection pack.
EXPANDING THE TREATMENT SERVICE
SP.Eye was designed to enable non-experts to deliver intravitreal injections. By controlling the needle and ensuring a perfect placement with each injection, the incidence of adverse events such as lens strike and retinal detachment is essentially zero.3
Additionally, as it controls the injection so effectively, it gives inexperienced injectors confidence as they learn. In the United Kingdom, several centres use SP.Eye exclusively for their nurse-delivered intravitreal services. In Australia and New Zealand, the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) has stated that it “sees benefit in partnering with the Australian College of Rural and Remote Medicine (ACRRM), the Royal Australasian College of General Practice (RACP), and the Australasian College of Emergency Medicine (ACEM), to ensure ophthalmic medical services, such as the management of conditions requiring the delivery of intravitreal injections, including the delivery of these injections by appropriately upskilled doctors”.4
Optometrists in Australia and New Zealand are not currently being considered as potential injectors. In Australia, Optometry Australia has said that the association is instead “focussed on how better use of optometrists in the pathway to treatment via IVI (intravitreal injections) can support better access to treatment for patients”.5
Never-the-less, the ability for non-specialists to be upskilled to inject using SP.Eye would potentially bolster the workforce, enabling intravitreal injections to be taken out to the community, rather than relying on patients to travel to clinics. In doing so, the carbon footprint associated with injecting is further reduced.
As mentioned earlier, this would also enable more effective delivery of intravitreal therapy in remote communities, that are currently under-serviced by health professionals and disproportionately affected by blinding macular disease, especially diabetic maculopathy.6
Increasing the number of injectors in these communities would inevitably reduce sight loss through delayed or missed treatment. Patient feedback after injections with SP.Eye is very compelling; over 95% of patients prefer it to the traditional (carbon intensive) technique.7 Furthermore, SP.Eye is sharps safe, and simplifies the management of sharps waste after injection. It can be locked shut very easily, in situations where no sharps disposal is available.
CONCLUSION
The SP.Eye intravitreal device is a proven safe, effective and well tolerated solution to improve the quality, safety, and efficacy of intravitreal injections.3 It has been in use in the United Kingdom and Europe for around 10 years and has an excellent safety record and unparalleled patient feedback.8
By using this innovative product to deliver intravitreal therapy, Australian and New Zealand ophthalmologists can significantly reduce the carbon footprint of their services and consider improvements to the provision of care in remote areas.
“ By using this innovative product to deliver intravitreal therapy, Australian and New Zealand ophthalmologists can significantly reduce the carbon footprint of their services ”

Dr Sam Evans MBS BSc is a consultant eye surgeon from the United Kingdom. He specialises in high volume cataract surgery, oculoplastics, and glaucoma. Dr Evans is particularly interested in innovative approaches to delivering high quality eye care and runs several businesses which aim to improve the access to, and delivery of, efficient services. Dr Evans invented the SP.Eye.
References
1. S.P.Eye estimate based on information available at medicarestatistics.humanservices.gov.au/statistics/do.jsp.
2. Power B., Brady R., Connell P., Analyzing the carbon footprint of an intravitreal injection. J Ophthalmic Vis Res. 2021 Jul 29;16(3):367–376. DOI: 10.18502/jovr.v16i3.9433.
3. Baxter, J., Guerin, E., Evans, K., Running a high-volume nurse led intravitreal service using the SP.Eye device – the Stanley Eye Unit experience. Eye News February/March 2024, Vol 30 No. 5. Available at www.eyenews.uk.com.
4. The Royal Australian and New Zealand College of Ophthalmology, RANZCO’s vision for Australia’s eye healthcare to 2030 and beyond. Available at ranzco.edu/wp-content/uploads/2023/06/RANZCO-Vision-2030-and-beyond-v2.pdf [accessed May 2024].
5. Kell, M., Expanding the scope of optometry in Australia, mivision 2023 Feb;(185):36–38.
6. Estevez J.J., Howard N.J., Craig J.E., Brown A., Working towards eye health equity for Indigenous Australians with diabetes. Int J Environ Res Public Health. 2019 Dec 12;16(24):5060. DOI: 10.3390/ijerph16245060.
7. Patient feedback following injection by SP Eye (n=61). Collected by Dr Sam Evans April 2024.
8. Greenaway, J., SP.eye innovation: How the SP.Eye intravitreal delivery guide and sharp safe system makes intravitreal injections safer, more precise, and more efficient [article sponsored by Salar Surgical]. The Ophthalmologist. 2023 May. Available at: theophthalmologist.com/subspecialties/eye-speye-innovation [accessed May 2024].