minews
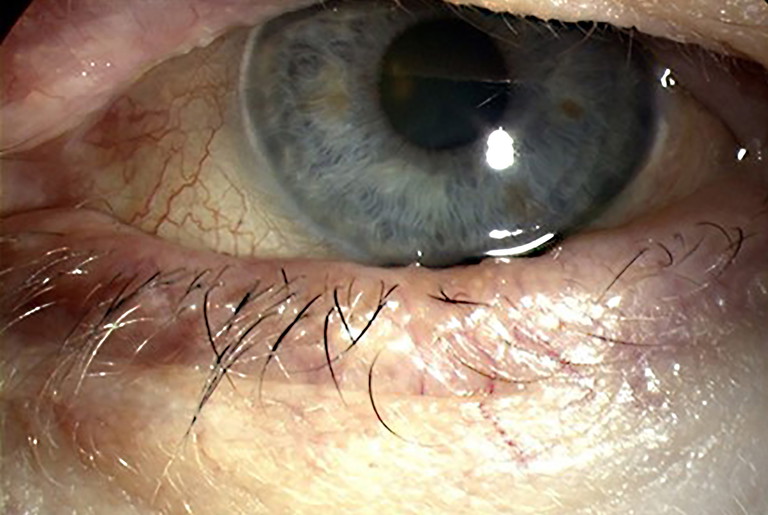
Inflammation of the eyelids and ocular surface in a patient with dry eye disease.
Effect of Topical Ciclosporin Reviewed
“The results… suggested a greater treatment effect with CsA 0.05% at the dosing of twice daily drops, alongside AT for DED”
Australian researchers have found that topical ciclosporin (CsA) may be more effective in relieving the symptoms and inflammatory impact on the cornea and conjunctiva in ocular surface disease than vehicle, artificial tears (AT) or other frequently used topical therapeutics.
But they also concluded that there’s a need for robust, well-planned, and larger clinical trials on the drug, designed to minimise bias, to better assess efficacy of topical ciclosporin on long-term dry eye-modifying effects.
The analysis of published literature on the use of topical ciclosporin for ocular surface disease (OSD) comes as a result of a collaboration of experts in the field, led by Professor Stephanie L. Watson OAM FARVO from the Corneal Research Group at the University of Sydney.
The team identified 583 randomised clinical trial (RCT) publication titles, of which 48 OSD RCTs were included. Of these, 30 trials found significantly better efficacy with ciclosporin, irrespective of dose or concentration for OSD.
The effect of ciclosporin was comparable to AT, vehicle, fluorometholone 0.1%, tacrolimus 0.03%, or diquafosol 3% only, in 13 trials.
Improved outcomes with ciclosporin for symptoms (RCTs comprising 1,107 patients) and clinical signs, including in ocular surface staining (2,505 patients) and the average number of goblet cells (138 patients) were found.
The investigators said 10 trials were judged to be at high risk of bias. The certainty of evidence was judged to be low to moderate, downgraded mostly for imprecision and risk of bias.
“Topical CsA treatment has been studied extensively in the treatment of DED (dry eye disease) and minimally in other ocular surface diseases,” the researchers wrote.1
“The majority of the trials in DED found CsA to be effective and with higher responder rates compared to other topical treatment alternatives. This effect was not dependent on CsA dose nor concentration.
“Consistency in treatment effect on the primary outcome measures, ocular surface symptoms, and staining for this review suggested that CsA may be better than vehicle or AT alone for symptoms and common clinical signs of ocular surface disease. The results from this current review of the literature suggested a greater treatment effect with CsA 0.05% at the dosing of twice daily drops, alongside AT for DED.”
They noted that ciclosporin was associated with a greater likelihood of discontinuations due to treatment-related adverse events.
The review concluded future clinical trials should give consideration to using “validated biomarker outcome measures, such as ocular surface staining and goblet cell density to better assess the efficacy of CsA on long-term dry eye-modifying effects”.
Reference
1. Chidi-Egboka NC, Fan L, Watson SL, et al. Evidence on the use of topical ciclosporin for ocular surface disease: A systematic review and meta-analysis. Clin Exp Ophthalmol. 2025 March 8; doi: 10.1111/ceo.14514.