mieducation
Optic Nerve Swelling? Keep Calm and Follow a Simple Set of Guidelines
It doesn’t seem to matter if you examine adults or children in your practice, the one clinical finding that tends to make any eye care professional slightly nervous is optic disc swelling.
And rightly so. We know that this clinical sign may be synonymous with serious neurological pathology. Consequently, we need to act fast, or we may mismanage the patient sitting before us. This mismanagement is two-fold: it may mean that we fail to recognise possible neurological involvement or that we over investigate the patients when we did not need to.
So how do we make this distinction? If only there was a universal protocol that we could follow.
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Understand what a papilloedema and a pseudo-papilloedema are,
2. Identify the common symptoms of raised intracranial pressure,
3. Identify the common clinical signs of advanced papilloedema, and
4. Know who to refer to, when papilloedema is confirmed.
WRITER Dr Christolyn Raj
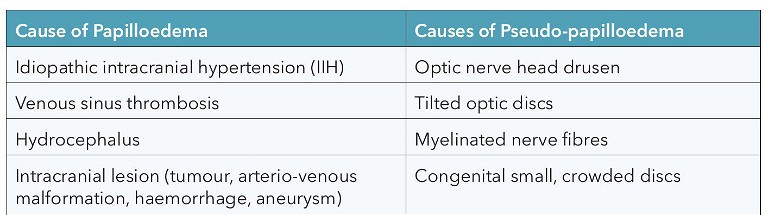
Table 1. Common causes of papilloedema and pseudo-papilloedema.
Diagnosing true optic disc swelling is actually quite straightforward. The mistake that all of us are guilty of making is that we tend to focus solely on the disc appearance itself and this may not provide all the answers we are looking for. Much like in assessing a patient with suspect primary open angle glaucoma, we need to look at the entire clinical picture. In the case of a glaucoma suspect, we use a myriad of tests – vision, refraction, intraocular pressure (IOP), optical coherence tomography (OCT) analysis, and visual fields (VF) – before formulating a diagnosis. Diagnosing optic disc swelling is much the same. Employing these guidelines in your day-to-day practice when seeing these patients can keep you on the right track in deciding whether to refer immediately, or organise a routine review at a later stage. Furthermore, these guidelines need not be altered, whether we are assessing children or adults.
For the purposes of this article, we will focus on bilateral true optic disc swelling caused by raised intracranial pressure (ICP) (clinically referred to as papilloedema) and anomalous optic disc swelling (clinically referred to as pseudo-papilloedema).
THE VALUE OF A GOOD HISTORY
There are many causes of papilloedema and pseudo-papilloedema. The main causes have been summarised in Table 1.
In the case of papilloedema, as mentioned, all the causes are related to an increase in ICP.11Being aware of the specific symptoms of raised ICP can help to refine our history taking with the aim of identifying critical symptoms that are in keeping with this presentation. Headache is a commonly reported symptom, however a headache that is pathognomonic of raised ICP has typical features such as: worse on moving from a supine to standing position, variability with motion, not particularly exacerbated by near or distant tasks, not relieved by analgesia, and often associated with other symptoms such as episodes of nausea or vomiting and tinnitus in one or both ears.
In contrast in pseudo-papilloedema, while a headache may be present, it typically does not have these features and in many cases the headache may be related to other factors such as uncorrected refractive error, de-focus, accommodative changes or even dehydration.
THE SECRET TO A THOROUGH OPTIC DISC ASSESSMENT
Ophthalmoscopy holds the ultimate key to making a diagnosis, however with the advent of OCT we can use both these modalities to our advantage.
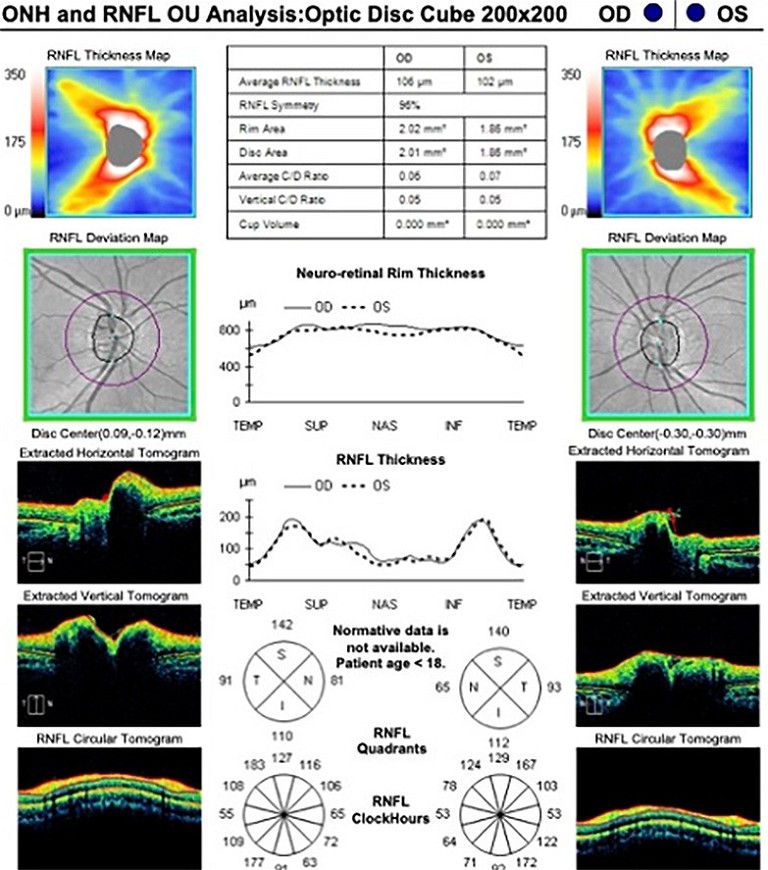
Ophthalmoscopy, preferably with a 60D fundus or similar high-magnification lens, is ideal to assess the optic disc margin and surface. In a younger child, indirect ophthalmoscopy will suffice. OCT will provide us with an accurate analysis of the peri-papillary retinal nerve fibre layer (RNFL) thickness as well as optic nerve head height and volume. This is demonstrated by the circles in Figure 1.2
There are a few aspects of analysing the disc contour that we should focus on. In almost all cases of papilloedema the disc margin should appear smooth though occasionally, with the presence of oedema, this can be a challenge to appreciate. Conversely in pseudopapilloedema, the disc margin contour can be variable from ‘irregular, lumpy, bumpy’, common in optic disc drusen (demonstrated by the arrow in Figure 1A), to asymmetrical and incomplete (tilted discs, myelinated nerve fibres), to difficult to visualise (crowded, hypoplastic discs).
OCT analyses of the RNFL in patients with papilloedema have reported that RNFL thickness is significantly greater in these patients compared with those with pseudopapilloedema of any type. In fact, in cases of pseudo-papilloedema, RNFL thickness tends to be normal in all four quadrants, albeit in this case slightly increased, as shown in Figure 1A when compared with normal optic discs (Figure 1B).3,43,4While not essential, many clinicians find it useful to use a radial RASTA analysis overlying the optic disc shown in Figure 1 to more accurately analyse the RNFL.
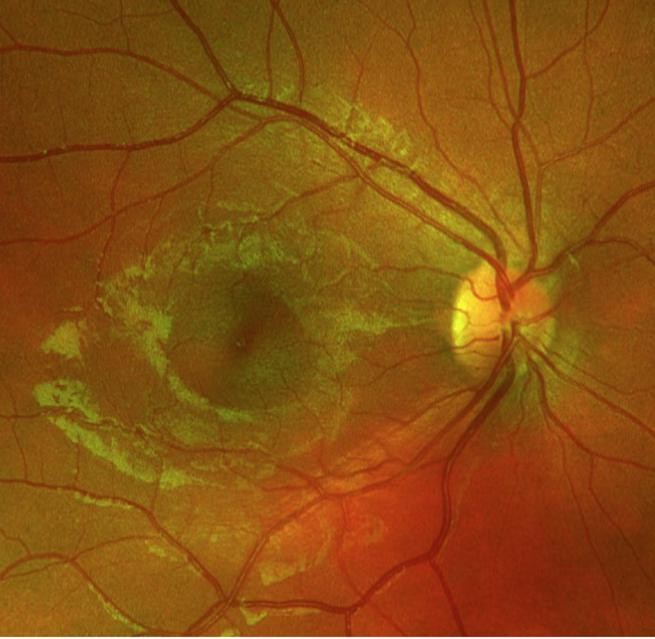
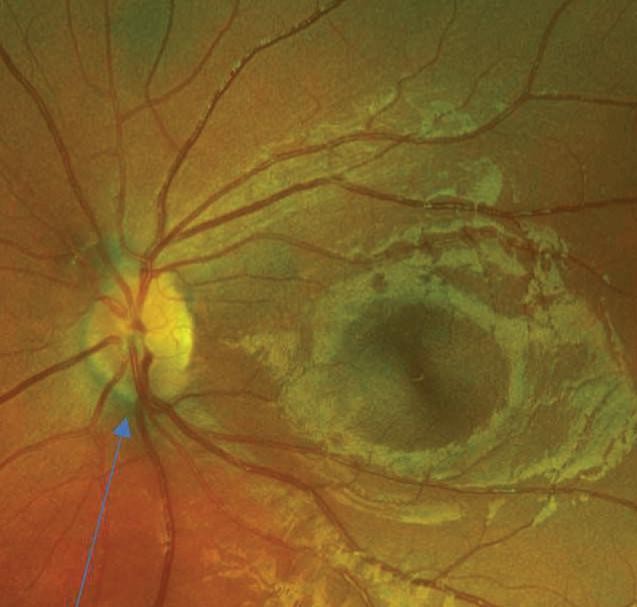
Figure 1. OCT analysis of RNFL in a patient with A) pseudo-papilloedema and B) normal disc appearance for comparison.
C) Pseudo-papilloedema: The optic discs show subtle buried optic disc drusen. In the corresponding OCT analysis, the arrow shows irregular inferior margin contour.

D) A similar OCT analysis for normal optic nerve head appearance.
WHAT ABOUT CHANGES ADJACENT TO THE OPTIC DISC?
When making the distinction of papilloedema from pseudo-papilloedema, assessment for peripapillary changes is critical to making the diagnosis. Swelling in the peripapillary RNFL has been demonstrated in several studies to be a highly specific clinical sign of true papilloedema. 55This swelling will often result in obscuration of the normal disc margin and of the major blood vessels leaving the disc. Additionally, as a result of oedema in the peripapillary region, axoplasmic stasis affects the smaller blood vessels in the region, resulting in signs such as RNFL haemorrhages and cotton wool patches (Figure 2).
Other signs that may be observed include choroidal folds, referred to as Paton’s lines, however these are not always present even in severe cases of papilloedema, with one study reporting only a 20% correlation.6
The combination of optic disc and peripapillary changes has led to an internationally recognised grading system, the modified Frisen scale. The salient features are summarised in Table 2.7 While this is a good grading system to qualitatively assess severity of papilloedema, it can be difficult to ascertain mild cases. On the other hand, OCT offers an objective and continuous scale for measurement of disc oedema and has been shown to be helpful to confirm the presence of oedema together with signs on ophthalmoscopy in mild cases. 8,98,9This reiterates the importance of using all modalities available to us to make an accurate diagnosis.
Most importantly, both the Frisen grading scale and OCT analysis become even more important in assessing improvement of optic disc swelling in patients with papilloedema. For many of us, this will be fairly straightforward with the use of fundus imaging and OCT per visit analysis display.
WHAT EXTRA TESTING IS NEEDED?
VF testing is as important as ophthalmoscopy and OCT analysis in patients presenting with disc swelling. An attempt at a baseline VF test on the patient’s first visit should always be considered. Common VF defects in papilloedema are variable depending on severity, however in general, follow a pattern similar to glaucomatous optic neuropathy and include arcuate scotomas with or without an enlarged bind spot. 10 Clinically this is understandable as the pathology results in RNFL bundle loss (Figure 3). In comparison, pseudo-papilloedema will often also present with VF defects. These are most commonly nasal scattered defects that do not follow a particular pattern, though this can be quite variable. 11
TO WHOM DO YOU REFER?
While these guidelines are detailed and comprehensive, it certainly won’t be enough in all clinical cases. There is still the possibility that we may doubt our findings or the fact that not all of the symptoms and signs will fit the clinical presentation. In these cases referral is sometimes necessary, but to whom or where should you refer these patients?
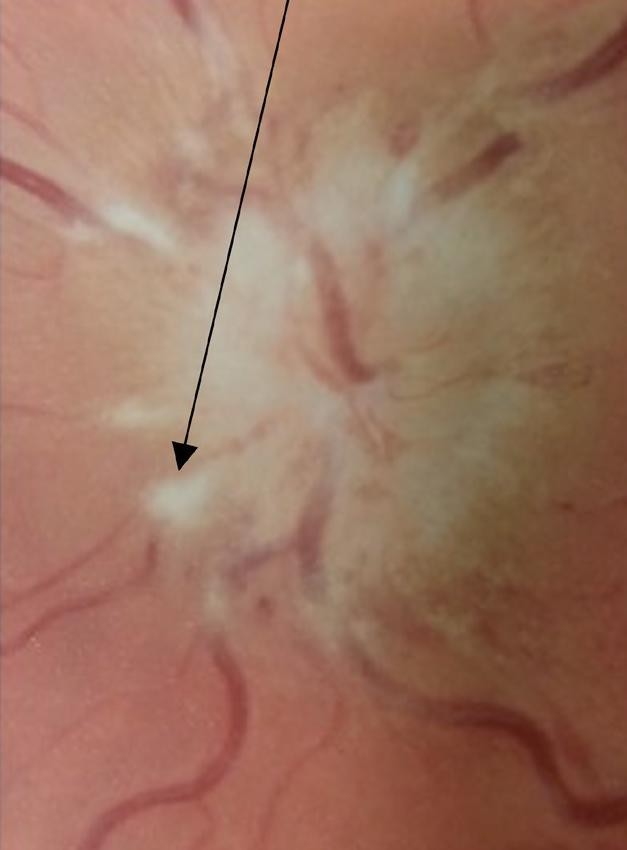
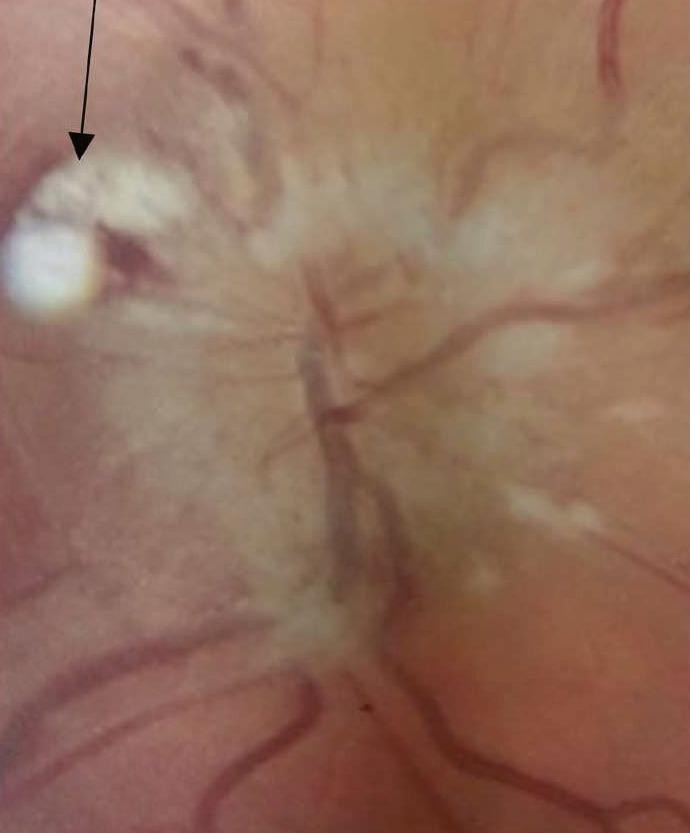
Figure 2. Papilloedema, Frisen Grade 5. Note the evidence of elevation of the entire disc and complete obscuration of the disc margin and all major blood vessels leaving the disc. Photo also depicts peri-papillary changes including haemorrhages and cotton wool patches (arrows).
The answer depends on what your particular concern is. If you are concerned that disc oedema is present, then a second opinion from a colleague is probably all that is needed prior to subsequent follow up investigations. If the concern is about uncertainty of an aspect of the optic disc assessment discussed above, then a referral to an ophthalmologist is likely to reassure you. However, if there is concern that papilloedema seems likely, then urgent referral to a hospital – not an ophthalmologist’s private clinic – is required. This will ensure that there is no delay in the required investigations that will often include neuroimaging followed by ultrasound guided lumbar puncture and review by a multidisciplinary team (neurology, neurosurgery, and ophthalmology).
LOOKING AHEAD
It is said that in any task that requires talent and dedication, “practice makes perfect”.
This could not be more true than in assessing patients with optic disc swelling. To become an ‘expert’ at assessing the swollen optic disc, we need to appreciate the features of plenty of healthy discs. This is not so easy to do as with experience, we are instinctively drawn to pathology but casually gloss over the ‘normal appearance’.
Taking the time to use these guidelines in your patients who do not have anomalous discs will allow you to detect the subtleties in a swollen optic disc with much more confidence and accuracy.
To earn your CPD hours from this article, visit mieducation.com/optic-nerve-swelling-keep-calmand-follow-a-simple-set-of-guidelines.
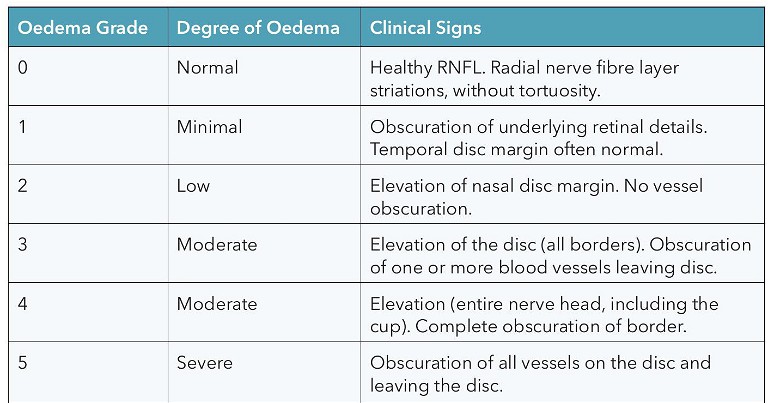
Table 2. Modified Frisen grading scale of optic disc swelling.7
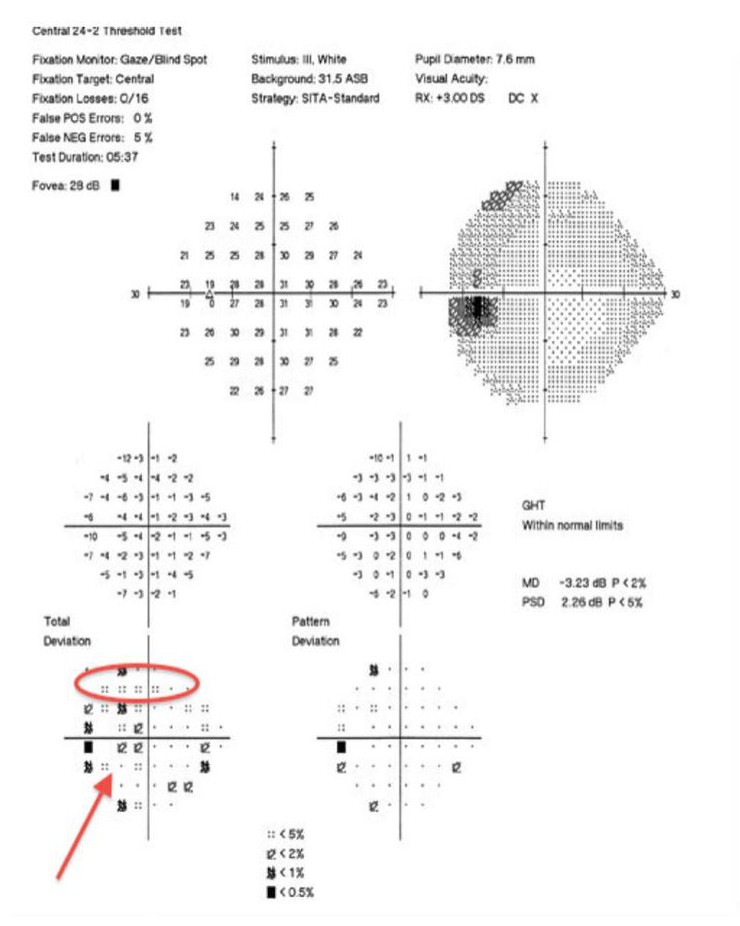
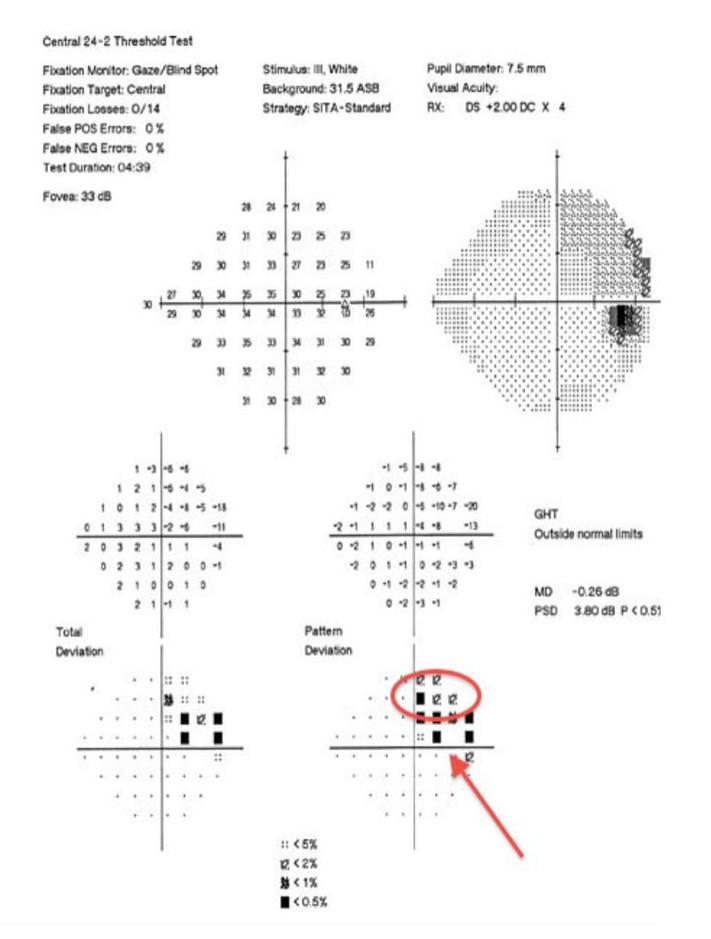
Figure 3. VF test for patient with optic disc appearance shown in Figure 2. VF shows superior arcuate defects in each eye that are continuous with an enlarged blind spot (arrows).

Dr Christolyn Raj MBBS (Hons) MMED MPH FRANZCO is a Melbourne-based ophthalmologist with a special interest in retinal disease. She is a published author and peer reviewer of several scientific journals. Dr Raj heads a retinal injection clinic at Camberwell, Blackburn and Coburg, and is responsible for the surgical management of patients with cataract and co-morbid retinal disease. She is currently undertaking active research projects in affiliation with her retinal clinics and the University of Melbourne, in surgical management of patients presenting with cataract in the context of diabetic eye disease.
References
1. Wakerley, B., Tan, M., Ting, Y., Idiopathic intracranial hypertension. Cephalalgia. 2015;35(3):248–61.
2. Skau, M., Yri, H., Sander, B., et al., Diagnostic value of optical coherence tomography for intracranial pressure in idiopathic intracranial hypertension. Graefes Arch Clin Exp Ophthalmol. 2013;251(2):567–74.
3. Heidary, G., Rizzo, J., Use of optical coherence tomography to evaluate papilledema and pseudopapilledema. Semin Ophthalmol. 2010;25 (5–6):198–205.
4. Malmqvist, L., Sibony, P.A., Fraser, C.L., et al., Optic Disc Drusen Studies Consortium. Peripapillary ovoid hyperreflectivity in optic disc edema and pseudopapilledema. Ophthalmology. 2018 Oct;125(10):1662–1664.
5. Bassi, S., Mohana, K., Optical coherence tomography in papilledema and pseudopapilledema with and without optic nerve head drusen. Indian J Ophthalmol. 2014;62(12):1146–51.
6. Carta, A., Favilla, S., Prato, M., et al. Accuracy of funduscopy to identify true edema versus pseudoedema of the optic disc. Invest Ophthalmol Vis Sci. 2012;53(1):1–6.
7. Scott, C., Kardon, R., Lee, A., et al., Diagnosis and grading of papilledema in patients with raised intracranial pressure using optical coherence tomography vs clinical expert assessment using a clinical staging scale. Arch Ophthalmol. 2010;128(6):705–11.
8. Lynne, D., Walker, E., Pezzimenti, J., The swollen optic disc: Is this an emergency?, Review of Optometry, Sept 2015.
9. Auinger, P., Durbin, M., Feldon, S., et al., Baseline OCT measurements in the idiopathic intracranial hypertension treatment trial, part II: correlations and relationship to clinical features. Invest Ophthalmol Vis Sci. 2014;55(12):8173–9.
10. Keltner, J., Johnson, C., Cello, K., et al., Baseline visual field findings in the Idiopathic Intracranial Hypertension Treatment Trial (IIHTT). Invest Ophthalmol Vis Sci. 2014;55(5):3200–7.
11. Traber, G.L., Weber, K.P., Sabah, M., et al., Enhanced depth imaging optical coherence tomography of optic nerve head drusen: A comparison of cases with and without visual field loss. Ophthalmology. 2017 Jan;124(1):66–73.