mipatient
Measuring Modern Myopia Management
WRITER Dr Margaret Lam
Getting into myopia for the first time or expanding your scope of practice? Dr Margaret Lam takes a look at the tools that will deliver the most value to your patients and your practice.
As myopia management evolves – with enhanced tools and a growing evidence base – clinicians are shifting from reactive prescription updates to proactive, evidencebased care. Central to this transformation is technology, which plays an increasingly vital role in diagnosis and management.
But with expanding diagnostic capabilities promising ever better detection and monitoring of myopia-related changes, clinicians are asking: Which tools deliver the most clinical value? And which instruments offer broader utility beyond myopia, to support comprehensive care across the practice?
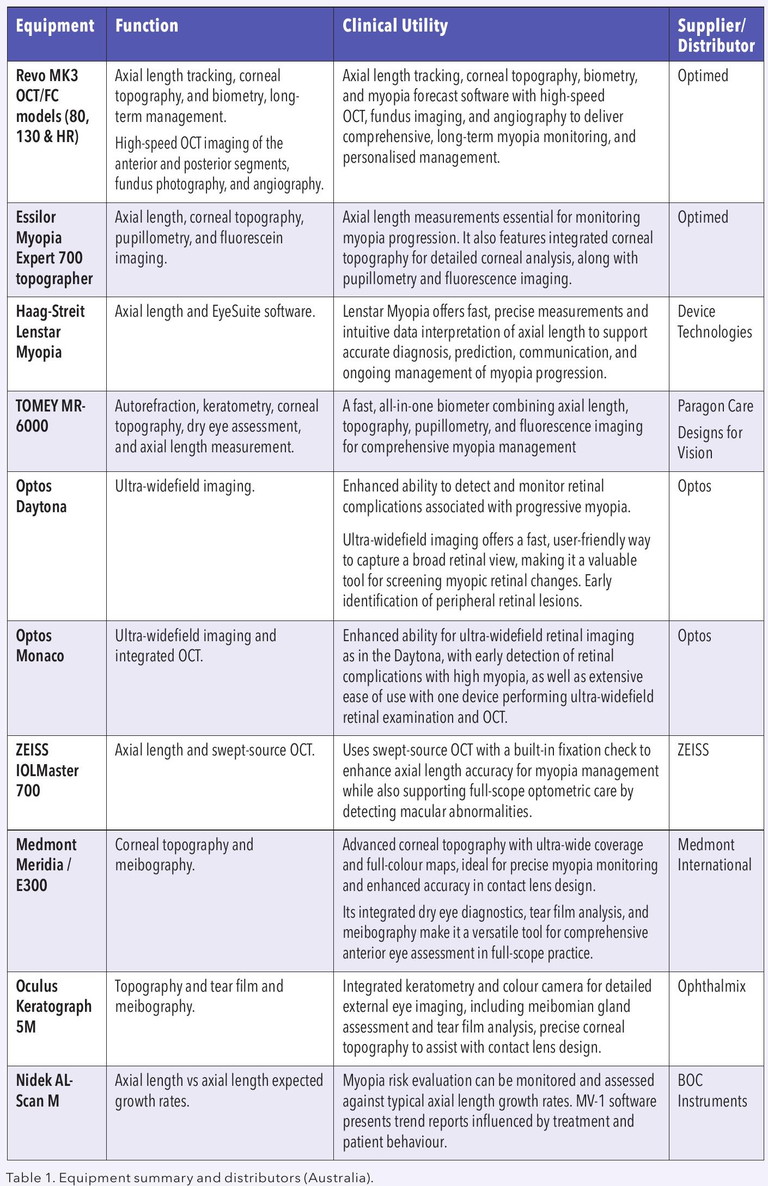
Without crowning a ‘best in show’, this article sets out the strengths and real-world applications of key technologies available in Australia – from ultra-widefield imaging to corneal topography and axial length measurement. All increasingly helpful tools that can meaningfully elevate the standard of care we provide.
AXIAL LENGTH MEASUREMENT: THE NEW FRONTIER
Device: Haag-Streit Lenstar Myopia / Lenstar 900
Distributor: Device Technologies Axial length measurement is becoming essential in structured myopia care. The Lenstar 900 is known for its reliability, and the Lenstar Myopia platform adds EyeSuite Myopia software, offering intuitive graphical tracking and age-matched normative comparisons. It enhances communication with patients and families, and suits practices that might already be familiar with Haag-Streit’s workflow.
Device: Oculus Myopia Master
Distributor: Ophthalmix The Myopia Master combines axial length, corneal topography, and auto-refraction in one platform. Tailored for myopia, it simplifies data presentation for families and aligns with Brien Holden Vision Institute monitoring protocols. Its patient education tools and user-friendly interface make it ideal for paediatric myopia clinics.
Device: ZEISS IOLMaster 700
Distributor: ZEISS Using swept-source optical coherence tomography (OCT), the IOLMaster 700 ensures highly precise axial length measurement with integrated fixation checks. It’s suitable for full-scope practices and aids in early detection of macular abnormalities – critical for managing high myopia risk.
WIDEFIELD IMAGING: BEYOND THE POSTERIOR POLE
Device: Optos Monaco and Optos Daytona
Distributor: Optos The Optos Monaco provides ultra-widefield imaging with integrated OCT – a standout for practices managing both high and progressive myopia. In my own clinic, the value of detecting early peripheral retinal changes, such as lattice degeneration or subtle tractional signs, cannot be overstated – especially when these are often missed with conventional fundus cameras, direct ophthalmoscopy, or even fundoscopy in uncooperative children or adults.
Both the Optos Daytona and Optos Monaco are helpful for full scope practice but are particularly useful when managing paediatric and pathological myopia cases, thanks to their speed as well as ease of non-mydriatic capture, and high patient compliance. The Monaco and Daytona also facilitate interprofessional referrals, thanks to highresolution documentation.
The Monaco’s combination of 200° fundus imaging and OCT enables impressive retinal peripheral imaging. If the Monaco is outside the budget of smaller practices, the Daytona provides a more affordable version for those who already have an OCT and want ultrawidefield imaging only.
Device: ZEISS Clarus 500
Distributor: ZEISS An alternative widefield option, the Clarus 500 offers true-colour imaging with an ultra-widefield of up to 133°, which can be extended through montaging. It doesn’t include OCT like the Monaco, but its superior colour fidelity offers excellent visibility of chorioretinal changes – a particularly useful asset when monitoring for lacquer cracks, staphylomas or myopic choroidal neovascularisation risk.

“early intervention, personalised care, and clear communication – underpinned by the appropriate imaging technologies – can deliver lasting impact”
CORNEAL TOPOGRAPHY AND ANTERIOR IMAGING
Device: Medmont Meridia / E300
Distributor: Medmont International Corneal topography is central to orthokeratology (OK) and other myopia interventions. The Medmont E300 remains a top-tier topographer, while the Meridia adds anterior segment imaging and meibography, which is ideal for practices managing OK and dry eye. Integration with Medmont’s lens design software is impressive and enhances accuracy in custom contact lens fitting.
Device: Oculus Keratograph 5M
Distributor: Ophthalmix The K5M offers detailed topography, noninvasive tear film analysis, and meibography. It supports pre-fit OK screening and is useful in dry eye management, especially when dryness affects lens tolerance. Its visualisation tools, including ‘traffic light’ tear film indicators, aid patient education and engagement.
CASE STUDY – CALLUM BROWN*
The following case study demonstrates the value of OK and ultra-widefield imaging in preventing retinal changes.
I first met 14-year-old Callum Brown in February 2015. Both of his parents were affected by high myopia – his mother was approximately -7.00D and she had a history of retinal detachment. Callum was already showing signs of fast myopic progression; his risk for progressive myopia and retinal complications was significant. Early adoption of OK, guided by clinical advice and a committed family decision, became the turning point in his visual development.
Callum was prescribed custom Contex OK lenses:
• Right Eye: 45.00 /-3.25 (0.45E), 8.23, 10.6, +1.00
• Left Eye: 44.50 /-3.50 (0.45E), 8.39, 10.6, +0.75
We’ve followed Callum’s care from early high school through to finishing his bachelor’s degree, his master’s, studying at some of Australia and England’s finest tertiary institutions, and commencing his early graduate career. A dedicated student and avid reader, he had every risk factor to become a high myope, yet over the past decade, he has shown no meaningful progression.
Throughout this time, we’ve supported his care with evolving imaging technology – from Oculus Keratograph and Medmont Meridia for corneal health and topography, to ZEISS and Nidek OCT for macular and retinal monitoring. Additionally, the Optos Daytona has helped to monitor Callum’s peripheral retina, given his family history of high myopia and retinal detachments. This has also proven to be an excellent communication and management tool to show Callum’s retinal health. Widefield views have allowed Callum and his mother to easily visualise the impact of his myopia being stable, and have offered an added layer of reassurance for peace of mind – both clinically, and for the patient and his family.
This case serves as a strong reminder that early intervention, personalised care, and clear communication – underpinned by the appropriate imaging technologies – can deliver lasting impact. A decade on, Callum’s myopia remains stable, with no signs of the high myopia or retinal complications that affected his parents, reinforcing the value of evidence-based myopia management with orthokeratology and ongoing monitoring. The use of advanced diagnostic tools has also played a key role in supporting clear, effective communication with both Callum and his family.
FINAL THOUGHTS
Investing in diagnostic equipment isn’t about buying the flashiest tools – it’s about choosing those that enhance clinical decision making, support efficient workflow, and foster strong patient relationships. Whether your focus is orthokeratology, atropine therapy, or dry eye, consider how each device can serve both specialty care and general practice.
These tools are more than diagnostics – they’re enablers of preventive care and platforms for patient engagement. That’s what elevates our role as primary eye care providers in the modern era of myopia management.
*Patient name changed for anonymity.
Dr Margaret Lam BOptom UNSW Post Grad OcTherapy practises optometry at 1001 Optometry in Bondi Junction in Sydney and teaches at the School of Optometry at the University of New South Wales (UNSW) as an Adjunct Senior Lecturer. She is the immediate past National President of Optometry Australia.