mieducation
Keeping the Pressure Off: A Holistic Approach to Proactive Glaucoma Care
‘An ounce of prevention is worth a pound of cure’ or, in the case of glaucoma, potentially multiple mmHg of intraocular pressure (IOP) control. Glaucoma touches over 200,000 Australians,1and costs us AU$4.3 billion per year.2 However, despite the high prevalence and cost burden, glaucoma management often begins only after measurable disease progression, and often remains focussed on IOP control alone. Drs Daniel Liu and Brian Ang present an alternate, proactive model of glaucoma care.
WRITERS Dr Zhengyang (Daniel) Liu and Dr Brian Ang
LEARNING OBJECTIVES
On completion of this CPD activity, participants should:
1. Understand the association between physical activity and eye health in glaucoma,
2. Be aware of how psychological stress can influence intraocular pressure control,
3. Realise the impact of diet, sleep, and nutrition on glaucoma progression, and
4. Be aware of the extra health benefits that nutraceuticals can provide patients.
Many areas of medicine frequently adopt proactive means of disease management. Patients with impaired glucose tolerance are counselled on strategies to prevent the onset of diabetes. Patients with macular drusen are encouraged to stop smoking, wear 100% UV protection sunglasses, and live a healthy lifestyle to minimise the chance of choroidal neovascularisation. These instances exemplify secondary prevention, aiming to mitigate disease progression before irreversible damage occurs.
Yet, in the case of glaucoma suspects, the typical approach involves observational monitoring until the onset of definitive glaucomatous damage, at which point tertiary prevention becomes the primary objective. At this point also, important opportunities for early intervention may have been missed. Furthermore, even after a glaucoma diagnosis is made, it is crucial to adopt treatment strategies that address factors beyond IOP alone, as disease progression can occur despite well-controlled IOP.3
Here, we present a proactive, preventive model for glaucoma care, which focusses on five key lifestyle and non-pharmacological pillars: physical activity, psychological stress reduction, sleep, diet and nutrition, and neuroprotection.
FIVE PILLARS OF PROACTIVE GLAUCOMA CARE
Pillar 1: Physical Activity
Physical activity is well recognised for its systemic health benefits, including its effects on cardiovascular disease risk, metabolic health, mental health, cognitive function, and ultimately a longer life span.4 Emerging evidence supports an association between physical activity and eye health in glaucoma through modulation of IOP, ocular perfusion, and neuroprotection.5
With the exception of patients with pigment dispersion, aerobic exercise has consistently been associated with a temporary reduction in IOP. IOP reduction of 1–5 mmHg occurs within as early as three minutes of walking, jogging, or cycling, and may be sustainable for up to 30 minutes, with greater effects observed in sedentary compared to active populations.5,6 However, it is unlikely that the transient IOP reduction from exercise provides significant neuroprotective benefits in glaucoma.7-10
Instead, the neuroprotective effect of exercise has been attributed to increased ocular perfusion pressure and the upregulation of neurotrophins such as brain-derived neurotrophic factor, improving mitochondrial function, and reducing inflammation.11-13 These factors contribute to the potential of exercise to slow visual field loss and glaucoma progression. Indeed, walking an additional 5,000 steps every day, or 2.6 hours extra of non-sedentary physical activity per week, have been associated with a 10% reduction in average rate of long-term visual field decline over two decades.14
However, clinicians should take several precautions when recommending physical activity to patients at risk of glaucoma. First, the isometric contraction in strength training has been associated with IOP rises of up to 10 mmHg when bench pressing: to reduce the IOP spike, one should exhale slowly during exertion instead of holding the breath in.15,16
Second, while swimming is an excellent form of non-weight bearing aerobic exercise, swimming goggles, especially the smaller and tighter ones, have been associated with significant IOP elevation of up to 17 mmHg.17,18 The Lions Eye Institute in Perth has recommended that children, in particular, should only wear swimming goggles with an internal horizontal width greater than 55 mm.17
Third, although yoga is a form of exercise that is well known to improve blood circulation, core strength, and general wellbeing, head-down yoga positions have been associated with transient IOP increases of up to 15 mmHg.19,20 Cases of glaucoma progression have been reported in daily practitioners of head-down yoga positions.21,22
PHYSICAL ACTIVITY
• Aim for at least 5,000 steps or 30 minutes of aerobic activity daily.
• Avoid IOP spikes from strength training by exhaling during exertion.
• Downward head positions and small swimming goggles can also cause IOP spikes.
Pillar 2: Stress Management
Psychological stress is increasingly recognised as an influential factor in IOP control, likely mediated through blood pressure and hormonal changes. Researchers from Brazil recently reported a mean increase of 4 mmHg in IOP among glaucoma patients following the application of a standardised psychological stress test.23 Additionally, in our clinical practice, we have observed that glaucoma patients experiencing chronic mental stress or anxiety are less likely to respond effectively to selective laser trabeculoplasty treatments. However, it is not just the impact on IOP; long-term mental stress can also disrupt vascular regulation in the microcirculation of the eye and brain, potentially compounding the risk of glaucoma progression.24
It is, therefore, essential for any IOP-lowering strategy to include stress management as part of a holistic approach. Mindfulness meditation was first reported to reduce IOP in 2018 – along with improved stress biomarkers, IOP reduced by 6 mmHg after 60 minutes of daily meditation for 21 days.25 Putative mechanisms for these effects centre around mental stress reduction through lowered cortisol (and in turn, lowered IOP and improved vascular function), improved brain oxygenation, increased neurotrophin levels, ameliorated parasympathetic activity, as well as reduced oxidative stress, glutamate excitotoxicity, and proinflammatory processes.26-29 Similarly, 365 breathing techniques – deep breathing with six breaths per minute for five minutes, three times a day – were shown to reduce IOP and serum cortisol, and improve autonomic dysfunction.30
Managing stress through mindfulness meditation or 365 breathing is safe, noninvasive, easy to implement, and highly effective. These techniques address a critical yet often overlooked factor in glaucoma progression, providing patients with a natural way to lower eye pressure while mitigating the effects of psychological stress on their overall health.
STRESS MANAGEMENT
• Psychological stress can increase IOP.
• Stress management techniques, such as meditation and 365 breathing, are effective in reducing IOP.
Pillar 3: Sleep Right
Quality sleep is crucial for restoring bodily function, and eye health is no exception.
Snoring, daytime sleepiness, insomnia, long sleep duration (over nine hours) and short sleep duration (under seven hours) are associated with an increased hazard of glaucoma of 11–13%.31 Obstructive sleep apnoea, in particular, is a significant risk factor for glaucoma, with an increased pooled adjusted odds of glaucoma of 266% in large meta-analyses including over four million patients.32 In these instances, visual field deterioration and retinal nerve fibre layer thinning potentially stem from intermittent nocturnal hypoxia despite IOP reduction during apnoeic episodes.33 Thus, sleep hygiene and treatment for obstructive sleep apnoea are recommended as part of a comprehensive glaucoma management plan for affected individuals.
When it comes to sleep, the position also matters, as it can significantly influence IOP. Nocturnal IOP tends to decrease when sleeping positions elevate the eye and head above the rest of the body.34 Lateral decubitus (side-lying) positions resulted in a 1–2 mmHg higher IOP in the dependent eye compared to the elevated eye and the supine position. Additionally, prone posturing was associated with IOP elevations of 2–3 mmHg compared to the supine position.35 Even light eyebedding contact may be associated with up to 10 mmHg elevations in IOP.36 For patients with asymmetric or unilateral glaucoma, adopting a supine or lateral decubitus sleeping position with the affected eye elevated may help limit overnight increases in IOP.
SLEEP
• Obstructive sleep apnoea is a significant risk factor for glaucoma.
• Aim for seven to nine hours of good quality sleep every night.
• Raising the affected eye(s) may reduce IOP elevations associated with specific sleeping positions.
Pillar 4: Diet and Nutrition
Diet and nutrition are key factors in maintaining eye health, particularly for those at risk of glaucoma. Specific nutrients have been linked to a reduced risk of glaucoma onset and progression, while a diet high in antioxidants and low in processed foods may help protect the optic nerve from damage.
Incorporating a variety of colourful fruits and vegetables into your daily diet provides essential vitamins – A, B, C, and E – that support general health and may reduce the odds of glaucoma by up to 63%.37,38 Fatty fish including salmon, mackerel, sardines, and anchovies are excellent sources of omega-3fatty acids, which have also been associated with up to 94% reduction in odds of glaucoma.39 On the other hand, ultraprocessed foods high in refined sugar, salt, and saturated fats may increase the risk of glaucoma by up to 80%.40,41
Multiple beverages have been studied in relation to glaucoma. Daily consumption of hot tea was associated with 74% lower odds of having glaucoma, but consuming decaffeinated tea, iced tea, coffee, or soft drinks at any level showed no similar benefit.42 Tea, rich in phytochemicals and flavonoids, may protect against glaucoma through antioxidant, anti-inflammatory, and neuroprotective effects.43,44 Caffeinated teas have been found to have greater antioxidant properties than decaffeinated teas, while instant iced teas have been found to contain significantly less flavonoids compared to brewed hot tea.45,46 Coffee, on the other hand, may increase IOP and glaucoma risk, especially in those who are genetically predisposed.47,48 Research suggests that those who are genetically at risk are 3.9 times more likely to have glaucoma if they drink more than two cups of coffee daily, compared to those who do not.47
A recent meta-analysis reported a potentially harmful association between alcohol intake and glaucoma, which was subsequently corroborated in a large population-based study of UK Biobank participants.49,50 Alcohol consumption was found to be consistently and adversely associated with glaucoma, even at intake levels below the United Kingdom (11.2 standard drinks/week) and United States (women, < 9.8 standard drinks/week; men, < 19.6 standard drinks/week) guidelines. While causality was not definitively established, the broader impact of alcohol on general health means that alcohol reduction or cessation is advisable for those with glaucoma.
DIET AND NUTRITION
• Eat a diet rich in vitamins (A, B, C, and E), antioxidants and omega-3fatty acids.
• A daily cup of hot tea may reduce glaucoma risk.
• Coffee and alcohol, even at intake levels below the standard guidelines, may increase glaucoma risk.
Pillar 5: Neuroprotection – Reinforcing the Optic Nerve
Nutraceuticals are products made from food or natural ingredients that offer extra health benefits beyond basic nutrition. These can include supplements, vitamins, or herbal extracts designed to support specific aspects of health.
There are several nutraceuticals that hold promise for slowing glaucoma progression by addressing IOP as well as non-IOP mechanisms that contribute to optic nerve damage in glaucoma. These non-IOP mechanisms, which may contribute to glaucoma progression even with optimal IOP control, can be broadly categorised into external stress, vascular factors, and cellular factors.
But we’ll start with IOP, the most important risk factor for glaucoma. Multiple preliminary clinical trials have reported that nutraceuticals such as saffron, blackcurrant, a combination of bilberry and maritime pine bark, and palmitoylethanolamide demonstrate modest ocular hypotensive effects, reducing IOP by up to 3 mmHg.51-53 The ocular antihypertensive effects of saffron are likely due to its potent antioxidant properties and its ability to alleviate psychological stress through carotenoid derivatives such as crocin and crocetin. These compounds may also offer additional optic nerve protection via direct antioxidant mechanisms.51,54 Similarly, the IOP-lowering effects of blackcurrant, bilberry, and French maritime pine bark are attributed to the antioxidative actions of anthocyanins and procyanidins, as well as their ability to reduce sympathetic tone and lower blood pressure.52 Palmitoylethanolamide (PEA) is a natural fatty compound produced by the body to help regulate inflammation, immune responses, and pain. A meta-analysis has shown that PEA can achieve IOP reduction of 0.6–3 mmHg after one month of use, most likely through its interactions with the endocannabinoid system.53,55
Closely interrelated with IOP is external psychological stress. Psychological stress contributes not only to elevated IOP, as noted earlier, but also to increased blood pressure and a heightened risk of cardiovascular issues. In addition to mindfulness meditation and 365 breathing, nutraceutical supplements have been shown to help alleviate psychological stress and support the body’s stress response. Key examples include saffron, lutein, and zeaxanthin, which act by modulating autonomic activity, improving heart rate variability, balancing cortisol levels, and influencing serotonergic and cholinergic neurochemical pathways.56-58
As for vascular factors, the two main mechanisms are impaired blood flow regulation and endothelial dysfunction. Endothelial dysfunction, often driven by elevated homocysteine levels, reduces the ability of blood vessels to deliver adequate oxygen and nutrients to the optic nerve. Homocysteine, a by-product of amino acid metabolism, rises when folate and vitamin B12 levels are low – a condition that becomes more common with age due to reduced absorption of these nutrients. This not only impairs microcirculation but also contributes to pseudoexfoliation syndrome and pseudoexfoliation glaucoma.59
Effectively addressing elevated homocysteine requires supplementation with activated forms of these vitamins, such as methylfolate (active folate) and methylcobalamin (active vitamin B12), which are more bioavailable and readily used by the body. These nutrients help restore endothelial function, improving blood flow to the optic nerve, and potentially reducing pseudoexfoliation risk.60
In addition to targeting homocysteine, nutraceuticals such as ginkgo biloba, bilberry, and French maritime pine bark have shown benefits for ocular blood flow. Ginkgo biloba, for instance, reduces blood viscosity and improves perfusion through key structures, including the retinal capillaries and ophthalmic artery, offering long-term stabilisation of visual field damage over the long term, particularly in normal tension glaucoma.61-63
Cellular factors represent the final category of non-IOP mechanisms central to glaucoma progression, with multiple interconnected processes driving optic nerve damage and visual loss. Among these, mitochondrial dysfunction plays a pivotal role by accelerating the death of retinal ganglion cells. A randomised controlled trial demonstrated that nicotinamide (vitamin B3) helps stabilise mitochondrial function, enhance resilience of the retinal ganglion cells, and improve inner retinal performance in glaucoma patients, with ongoing studies investigating its longterm neuroprotective effects.64
Oxidative stress and chronic inflammation further increase neuronal susceptibility to damage, creating an ocular environment less conducive to neuroprotection.
Botanical extracts such as saffron, bilberry, ginkgo biloba, and grape seed exhibit potent antioxidant and anti-inflammatory properties, helping to mitigate these harmful processes and support retinal ganglion cell and optic nerve health.63,65-69
Macular pigment deficiency, although traditionally associated with age-related macular degeneration, is now recognised as an important risk factor in glaucoma. Macular pigment optical density (MPOD) has been shown to be lower in individuals with glaucoma compared to controls, with subsequent studies correlating lower MPOD to the extent of foveal ganglion cell complex loss and central 10° visual field defects.70 This evidence suggests that depleted levels of the macular carotenoids lutein and zeaxanthin, contributing to central field defects, may be more prevalent in glaucoma than previously realised. Supplementing with these carotenoids significantly increased MPOD and improved mesopic contrast sensitivity under glare conditions when taken over 18 months.63,65
Finally, impaired axonal function and disrupted neural conduction in the visual pathways contribute to the progressive vision loss observed in glaucoma. Supplementation with vitamin B12 and citicoline has shown potential in improving neurophysiological retinal performance and enhancing post-retinal signal transmission, offering measurable benefits in visual field parameters and overall visual function.71 In particular, vitamin B12 in the form of methylcobalamin plays a critical role in preserving the myelin sheath around neurons, maintaining nerve cell membrane stability, and synthesising neurotransmitters – all vital for axonal function. Supplementing with methylcobalamin 1.5 mg daily has been shown to reduce the progression of visual field loss in normal tension glaucoma over the long term.72
“There is currently no medical consensus or one-size-fits-all approach to neuroprotection and lifestyle modification in glaucoma”
By addressing these non-IOP mechanisms – including psychological stress, vascular factors, and cellular dysfunction – targeted nutraceutical interventions serve as a vital, evidence-based complement to traditional IOP-lowering therapies.
NEUROPROTECTION
• Nutraceuticals can target the non-IOP mechanisms of glaucoma progression, including psychological stress, vascular factors, and cellular factors.
• Botanical extracts, such as saffron, bilberry, ginkgo biloba and lutein, reduce the impact of psychological stress, promote blood microcirculation, protect against oxidative damage, and restore macular pigment density.
• B-vitamins, such as methylcobalamin, methylfolate, and nicotinamide, reduce homocysteine levels, restore mitochondrial metabolism, increase retinal ganglion cell resilience, and support axonal function.
A Clinical Approach
There is currently no medical consensus or one-size-fits-all approach to neuroprotection and lifestyle modification in glaucoma. As the evidence base continues to evolve, transparent and honest communication is essential to empower patients to understand both the potential benefits and limitations of these complementary approaches within their overall glaucoma risk management.
In our clinical practice, we prioritise discussing all five key pillars of proactive glaucoma care with our patients, as addressing non-IOP mechanisms is fundamental to achieving truly comprehensive glaucoma neuroprotection. This approach includes exploring the role of individual nutraceutical supplements or combination formulations, such as the Nutravision formula, to support a holistic strategy for managing glaucoma effectively.
A case study follows, illustrating the potential benefits of the proactive glaucoma care approach, including showcasing patient progress before and after its use.
Case Study in Proactive Glaucoma Care
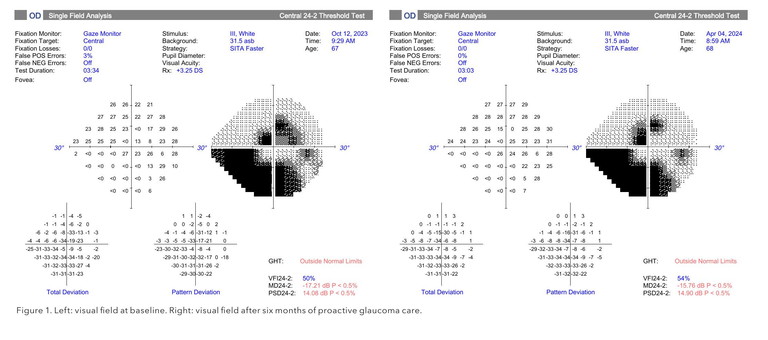
Alice Diller* is a 67-year-old female with advanced normal tension glaucoma who had previously undergone cataract surgery combined with trans-trabecular stent implantation in her right eye. Her fellow eye has poor vision due to amblyopia. At baseline, her right vision was 6/7.5 corrected, IOP 13 mmHg on no therapy, MD -17.21, PSD 14.08, and VFI 50% (Figure 1; left).
Ms Diller was very keen to proactively manage her glaucoma risk through lifestyle measures because her ‘good’ right eye had already suffered significant vision loss. As per the five key pillars of proactive glaucoma care, she made adjustments to her exercise routine, sleeping habits and diet, and also started taking the Nutravision supplement (containing bilberry, ginkgo biloba, grape seed, saffron, lutein, zeaxanthin, nicotinamide, methylcobalamin, methylfolate, and nicotinamide).
Six months later, her right vision was 6/7.5 corrected, IOP 12 mmHg on no eye drops, with a slight improvement in her visual field (MD -15.76, PSD 14.90, and VFI 54%, Figure 1; right). Ms Diller also experienced significant relief from her dry eye symptoms, no longer requiring daily lubricant eye drops. Most importantly, she felt less stressed from work and had noticed a meaningful improvement in her overall wellbeing.
It is important to emphasise that these five pillars are not a replacement for prescribed glaucoma treatments or regular eye examinations but serve as an adjunct to enhance the effectiveness of a comprehensive care strategy, aiming to preserve vision and improve patient outcomes.
Additionally, the primary goal of neuroprotection is to reduce the risk of progression and stabilise the condition, rather than achieving significant improvements in visual field indices. While improvements in visual fields may be observed, the key measure of success remains a slowed rate of progression.
All of our patients undergoing such interventions continue to be closely monitored.


Dr Zhengyang (Daniel) Liu BBiomed MD (Distinct) MBiostat GStat is aNSWbased unaccredited ophthalmology registrar and clinician researcher with over 30 peer-reviewed publications. A top graduate of the University of Melbourne's Biomedicine, Medicine, and Biostatistics programmes, Dr Liu’s research focusses on glaucoma, inherited retinal diseases, and advanced statistical methods for improving clinical evidence, with the aim of enhancing patient care and outcomes.
Dr Brian Ang MBChB FRCSEd (Ophth) FRCOphth FRANZCO is a Melbournebased glaucoma specialist, clinical researcher, and co-founder of Nutravision (nutravision.com.au). He has over 70 peer reviewed publications, with research interests in novel surgical treatments and neuroprotection for glaucoma. Dr Ang is a keen advocate of ‘proactive glaucoma care’ – the proactive management of risk for glaucoma and glaucoma suspect patients through natural lifestyle measures and nutrition.
CONCLUSION
Proactive glaucoma care represents a transformative shift, combining physical activity, stress management, quality sleep, nutrition, and neuroprotection to slow or even prevent disease progression. This patient-centred approach preserves vision and enhances quality of life, and may also help reduce the long-term burden on healthcare systems.
By addressing disease progression before irreversible damage occurs, the five key pillars equip clinicians to take a leading role in improving outcomes for this complex condition. Acting in our patients’ best interests means leveraging the evidence available today to educate and support them in adopting these strategies, setting a new standard for holistic glaucoma management.
*Patient name changed for anonymity.
To earn your CPD hours from this article visit mieducation.com/keeping-the-pressure-off-aholistic-approach-to-proactive-glaucoma-care.
References available at mieducation.com.