miophthalmology
Cataract in Optometry Practices: Enhancing Patient Management
WRITER Associate Professor Smita Agarwal
As global life expectancy rises and patient expectations evolve, demand for cataract surgery and premium visual outcomes continues to grow. As Associate Professor Smita Agarwal notes, with many patients presenting initially in optometric practice, the optometrist’s role has never been more critical.
Today’s cataract management model places the optometrist at the front line, not only for detection and referral but also for patient education, expectation management, and long-term postoperative care.
In an increasingly refractive-driven model of cataract surgery, patients are often less concerned with the diagnosis itself, and more invested in the visual quality they can expect after surgery. With this shift, the optometrist’s clinical insights and communication skills are instrumental in preparing patients for a successful outcome.
Optometrists must play a comprehensive role in cataract care, from preoperative evaluation and intraocular lens (IOL) education to postoperative co-management, along with long-term care of ocular health.
CATARACT PREVALENCE: THE OPTOMETRIST’S ROLE
Cataracts are an almost inevitable consequence of ageing. As the lens proteins degrade over time and the optical media become increasingly opaque, the resultant impact on vision can range from mild blur and glare sensitivity to severe functional blindness. With an ageing population in Australia and globally, optometrists are seeing a steady increase in the number of patients with clinically significant cataracts. These patients often present with gradually declining best-corrected visual acuity, difficulty with night driving, haloes, or trouble performing near tasks, all of which are frequently identified during routine consultations.
As primary eye care providers, optometrists are ideally positioned to make the initial diagnosis through comprehensive assessments that include slit lamp bio-microscopy, visual acuity (VA) testing, and dilated fundus examinations. Optical coherence tomography (OCT) and other imaging modalities now play a key role in assessing concurrent pathology that may influence surgical outcomes. While referral to an ophthalmologist remains necessary for the surgical intervention itself, it is the optometrist who often is responsible for first identifying when cataract surgery is appropriate and for laying the groundwork for what the patient can expect from their surgery.
CHANGING PATIENT EXPECTATIONS
Today’s cataract patients are more informed and more visually demanding than ever before. Gone are the days when patients were simply grateful to have their vision restored to a basic functional level. Many patients now present with a desire for spectacle independence, particularly for intermediate and distance tasks such as driving, using digital devices, and performing household activities. In the era of smartphones, laptops, and digital workspaces, intermediate visual clarity is no longer a luxury; it’s a necessity.
Patients are often influenced by anecdotal reports from friends or family members who have had successful experiences with multifocal or extended depth of focus (EDOF) IOLs. As such, they arrive with high expectations for postoperative vision, often anticipating full restoration of sight across all distances. Some seek complete freedom from glasses, while others are comfortable with limited use, such as reading spectacles, provided their primary daily activities are not hindered.
Understanding patient expectations is just one piece of the preoperative puzzle. Optometrists play an essential role in aligning their patients’ expectations with reality. By discussing the benefits and limitations of various IOL options, and the likelihood of visual phenomena such as glare or haloes, the optometrist can temper unrealistic assumptions and prepare patients for informed decision making. This expectation management forms a cornerstone of the modern cataract journey and is fundamental in preventing postoperative dissatisfaction.
EDUCATING ON IOL OPTIONS AND OUTCOMES
Perhaps one of the most significant roles an optometrist plays in cataract management is the explanation of intraocular lens choices. By the time a patient meets their ophthalmic surgeon, they should already have a working understanding of the primary lens options available to them. This enables more productive discussions during surgical consultations and allows for more time to be spent on surgical planning rather than basic education.

“In an increasingly refractive-driven model of cataract surgery, patients are often less concerned with the diagnosis itself, and more invested in the visual quality they can expect after surgery”
Monofocal lenses remain the most used IOLs, particularly within public systems and for patients with significant ocular comorbidities. These lenses provide high-quality vision at a single focal point, usually set for distance. Patients with monofocal lenses typically require spectacles for near or intermediate tasks. Many patients are content with this arrangement, especially those who are already accustomed to wearing bifocal or multifocal glasses and are not seeking significant changes to their visual routine. However, patients interested in monovision correction – where one eye is corrected for near and the other for distance – must be carefully counselled. While this option can provide a degree of spectacle independence, not all patients tolerate the induced anisometropia or the associated reduction in binocular function. A trial with contact lenses prior to surgery can help assess monovision suitability.
EDOF lenses can be designed on spherical aberration (SA) modulation, chromatic aberration (CA) modulation, or wavefront shaping technology (it’s almost difficult to remember all the current available options). Besides the choice overload, they all offer an attractive middle ground between monofocal and multifocal IOLs. They work by extending the range of focus, improving intermediate and some near vision, while minimising the dysphotopsias commonly associated with multifocal IOLs. These lenses are especially beneficial for patients who prioritise functional vision for tasks such as driving, computer work, and navigating environments but are not necessarily seeking full reading independence. Enhanced monofocal designs also provide improved intermediate vision while maintaining high image quality and contrast, making them suitable for patients with early ocular comorbidities or lifestyle demands that fall between traditional lens categories.
Multifocal IOLs, especially trifocal designs, divide incoming light into multiple focal points (typically distance, intermediate, and near). This allows for a high degree of spectacle independence, but at a cost. These lenses can reduce contrast sensitivity and are prone to glare and haloes, particularly under low-light conditions. Dysphotopsias are an expected outcome, and while many patients adapt over time, not all find the visual quality acceptable. Therefore, careful patient selection and preoperative counselling are paramount. Patients who read extensively, perform detailed near work, or drive frequently at night must be cautioned about these potential limitations. Rigorous management of the ocular surface is crucial in patients undergoing cataract surgery, especially with multifocal IOLs, for accurate preoperative measurements and reliable postoperative outcomes.
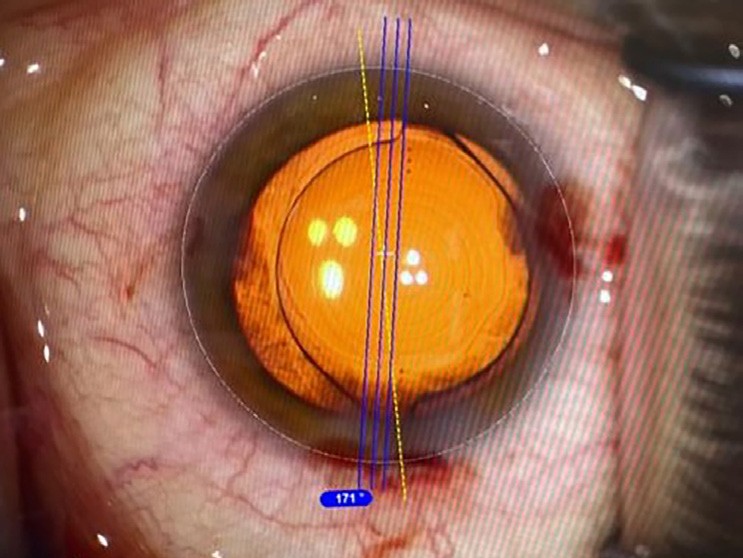
Figure 1. Toric multifocal IOL in cataract surgery with image guidance.
MANAGING ASTIGMATISM
Astigmatism correction has evolved dramatically with the availability of toric IOLs (Figure 1).1 These lenses offer excellent refractive results for patients with regular astigmatism, especially in the 1.0D and above range, with some newer lenses able to correct as low as 0.75D.1 However, toric multifocal and EDOF lenses require high precision in alignment and centration, making them less suitable for eyes with irregular astigmatism, keratoconus, or unstable corneas (Figure 2). In mild, forme fruste keratoconus, or post-crosslinking cases, monofocal toric lenses remain the safest and most effective solution. Assessment of corneal health for opacities, signs of dystrophy, keratoconus indicators such as Vogt’s Striae, or scissoring on retinoscopy, will help to establish the need for toric IOLs in a patient. Where available, topography/tomography imaging will improve IOL selection based on the amount of higher order aberration observed. This will also improve the image guided alignment chosen intraoperatively.2,3
When available, toric IOLs result in better patient satisfaction and uncorrected visual acuity; the stability of newer advanced toric IOLs limits postoperative rotation and predictable visual outcomes. With a study showing that between 47.2–62.7% of Australians over 70 have clinically significant astigmatism (≥1.00D), the demand for toric IOLs is already quite high and expected to increase.4
To refine accurate alignment of these lenses intraoperatively, image guidance is available (Verion from Alcon and Callisto from ZEISS), which can be used with most modern microscopes. Manual marking was used in the past but accurate alignment of toric IOLS – more so with multifocal toric IOLS – is crucial to avoid residual error and dissatisfied patients. Currently, routine accuracy of IOL placement is reported at within 5° of the target.5 Due to the increments of correction typically being in 0.5D or 0.75D steps, it is unlikely that patients will result in precisely zero remaining astigmatism, however with accurate biometry and surgical technique, approximately 90% of patients will be within 0.5D of their target.6
MANAGING PATIENTS WITH DIABETES
Diabetic patients pose a multifaceted challenge in the cataract surgery journey. While many patients with diabetes can undergo routine cataract extraction with excellent outcomes, the presence of diabetic retinopathy (DR), diabetic macular oedema (DMO), and systemic instability increases the risk of postoperative complications and poor visual recovery, particularly when premium IOLs are being considered.7 For optometrists, this patient group requires heightened vigilance, thorough preoperative screening, and careful expectation management.
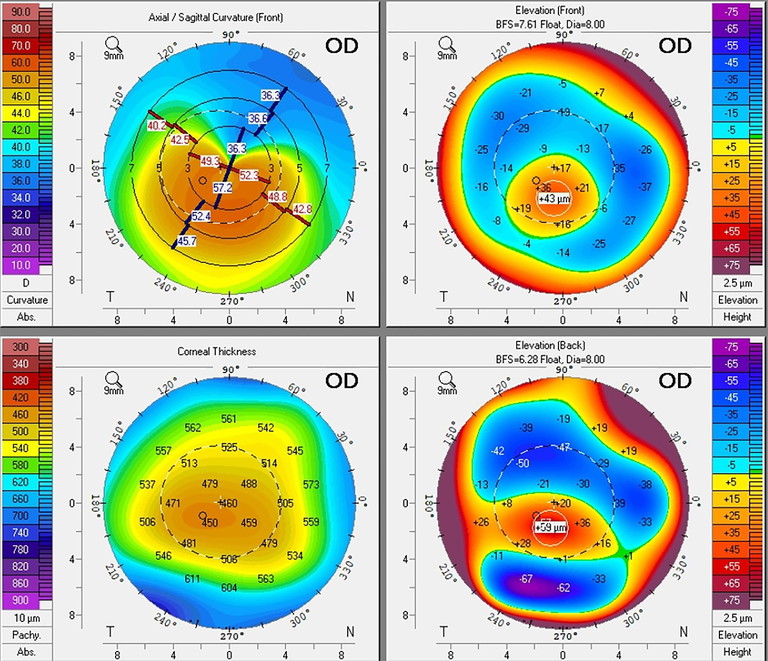
Figure 2. Topography of an eye with keratoconus.
Importantly, when referring diabetic patients for cataract surgery, optometrists should always confirm whether any signs of DR are present and advise that this pathology be managed and stabilised prior to surgery.8 Where macular oedema is evident, referral for treatment (such as intravitreal anti-VEGF, grid laser photocoagulation, or steroid therapy) may be indicated before cataract extraction is pursued.9 In these cases, the urgency of visual restoration must be weighed carefully against the risk of exacerbating retinopathy by operating through an untreated or unstable macular environment.
When it comes to IOL selection, diabetic patients with existing retinopathy or maculopathy are generally not ideal candidates for premium lenses, especially trifocal designs. These lenses rely on splitting incoming light into multiple foci to provide a range of vision, which inherently reduces contrast sensitivity. In the presence of macular thickening, retinal ischemia, or even mild epiretinal membrane traction, the quality of the retinal image is already compromised, thus implanting a diffractive lens in this context often leads to disappointing results and further compounds the risk of patient dissatisfaction and visual morbidity.7 Therefore, trifocal IOLs are often avoided in diabetic patients with any degree of maculopathy or active DR, even if the condition is mild or asymptomatic. An additional consideration is the need for future retinal visualisation and treatment. Material selection is also important; hydrophilic lenses are generally avoided in diabetic eyes as they carry a higher risk of opacification and calcification, which is exacerbated in diabetic patients who typically have elevated serum or aqueous phosphate levels.
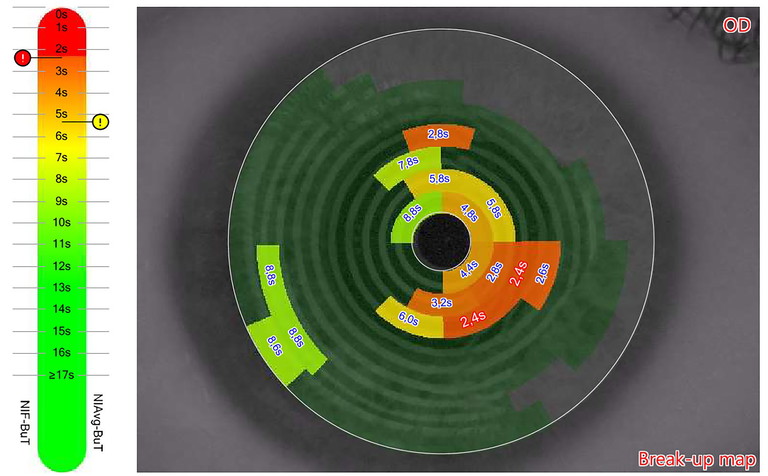
Figure 3. Tear break-up time (MS-39) .
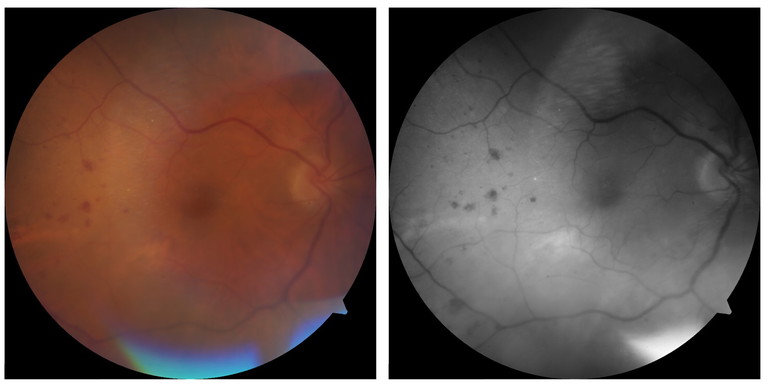
Figure 4. Diabetic retinopathy.
In low-risk diabetic patients, without evidence of retinopathy or macular changes, enhanced monofocal or non-diffractive EDOF lenses may still be suitable.7 These lenses offer extended depth of focus with minimal compromise to contrast sensitivity and do not split light in the same way as multifocal IOLs, reducing the risk of dysphotopsia and making them better tolerated in eyes with borderline pathology. However, even these lenses must be used with caution. The use of these premium IOLs in diabetic asymptomatic patients is considered controversial by some as they make laser therapy more difficult should it be required later in life.10 Expectation management remains paramount as patients must be made aware that even with non-diffractive designs, spectacle independence is not guaranteed, and close follow-up will be required.
A holistic view of the patient is essential. Optometrists must consider not only the ocular findings but the systemic nature of diabetes when educating patients. Poorly controlled blood glucose levels increase the risk of infection, delay healing and inflammatory response, and if poorly controlled, patients who previously received a premium IOL can start to develop visual complications and dysphotopsia symptoms.7,8
Studies have revealed that 54% of diabetic patients usually have symptomatic and/or asymptomatic dry corneas.11 The prevalence increases with increasing age and in women.12 The incidence for dry eye is correlated with the level of glycated haemoglobin. Hyperglycaemia affects the neuronal fibres, corneal epithelium, tear film osmolarity, and/or inflammatory changes, which can impact tear film, causing dry eyes and making it difficult for these premium lenses to function and provide optimum visual improvement. This, of course, results in unhappy patients (Figure 3).12
Diabetic patients must be counselled comprehensively. The prognosis for visual recovery may be good, but it is almost always guarded in the presence of maculopathy or retinopathy. Expectations surrounding EDOF or multifocal IOLs should be tempered with the advantages of achieving clear and stable distance vision, with the likelihood of reading glasses being required.
Cataract Surgery and GLP-1 Agonists
Recently, quite a few GLP-1 agonists have been approved for control of blood sugar levels and/or weight reduction. They stimulate insulin production by the pancreas and reduce glucagon secretion, causing reduced gastric emptying and reduced appetite with improved glycaemic control and weight loss.13
In Australia, three drugs – Ozempic (semaglutide), Trulicity (dulaglutide) and Victoza (liraglutide) – are approved for the management of adults with diabetes. Mounjaro (tirzepatide) is approved for both diabetes and chronic weight management. Wegovy (semaglutide) and Saxenda (liraglutide) are approved for weight loss. While they have been a game changer for many diabetic patients, recent studies also point to them as having the greatest risk of worsening diabetic retinopathy (Figure 4).13 It is crucial to take history and assess these patients prior to cataract surgery for stabilisation of DR and blood glucose levels. Rapid blood glucose fluctuation can also cause refractive error shift and blurred vision due to lens thickness changes.
The Australian and New Zealand College of Anaesthetists (ANZCA) released consensus guidelines recommending that patients going for elective cataract surgery do not have to stop any of these drugs. They have to have clear fluids 24 hours before their procedure followed by usual six-hour nil by mouth fasting before their procedure to avoid aspiration with reduced gastric emptying.14
MANAGING GLAUCOMA PATIENTS
Cataract surgery for patients with glaucoma can present unique challenges to surgeons (Figure 5). While cataract surgery alone may benefit certain glaucoma patients by improving visual function and potentially lowering intraocular pressure (IOP), the presence of glaucomatous optic neuropathy significantly complicates IOL selection and the current management of patient IOP may impact the timing of the surgery if uncontrolled or unstable.15 For optometrists involved in co-management, it is vital to assess not only the degree of glaucoma but also the visual quality demands of each patient when discussing IOL options and referring for surgical planning.
Glaucoma, particularly in its chronic or advanced forms, has a well-documented impact on contrast sensitivity.16 Given this background, multifocal IOLs, which inherently reduce contrast sensitivity, are generally not considered suitable in patients with moderate to severe glaucoma. Even in early disease or among glaucoma suspects, extreme caution is advised. Multifocal IOLs tend to exacerbate the contrast sensitivity deficit already present in these patients, particularly under mesopic conditions. Moreover, patient satisfaction following multifocal IOL implantation in the setting of glaucoma is significantly lower than in non-glaucomatous populations, largely due to these optical compromises.16
Patients with pseudo-exfoliation syndrome (PXF) often exhibit poor pharmacologic dilation and zonular weakness, which can increase the risk of IOL instability.17,18 This can complicate the use of toric IOLs (better to avoid toric multifocal IOLs) in patients with corneal astigmatism as these patients are at greater risk of IOL tilt, rotation, or decentration.18 Patients with PXF and a significant amount of astigmatism should receive explanations about the possibility of continued use of glasses postoperatively if significant zonular instability is encountered intraoperatively. Capsular tension rings (CTRs) can help stabilise the bag and implantation of toric IOLS if zonular instability is focal and mild. If zonular instability is more than 3–4 clock hours, modified CTRs or capsular tension segments are needed, and it is better to avoid toric IOLS if the bag is still not looking stable.
In glaucoma patients with advanced field loss or central field involvement, visual prognosis remains guarded, regardless of IOL selection. These patients require careful counselling preoperatively about the likely visual outcome, which is often limited by optic nerve damage rather than optical clarity. Avoiding false hope around spectacle independence or ‘high definition’ vision is key to maintaining patient satisfaction. Optometrists should remain vigilant during the initial assessment and could educate patients on the status of the optic nerve, IOP control, presence of PXF, and any current or previous glaucoma medications. This information is critical to surgical planning, particularly where intraoperative risks or refractive expectations may be influenced by pre-existing disease.
EXPECTATIONS POST-REFRACTIVE SURGERY
Post-refractive surgery patients present unique challenges with primary hurdles being accurate calculation of IOL power and dry eyes, as prior refractive surgery alters corneal curvature, affecting measurements and IOL power calculation. It is usually getting better with advanced diagnostic means and better IOL calculation formulae. Studies report that <70% of eyes achieve refractive outcomes within ±0.5D of target, compared to >80% of eyes that undergo surgery in virgin corneas.19 It is imperative to do detailed preoperative evaluation including corneal irregularity, planning of refractive target, and then choosing the appropriate IOL based on IOL calculations and spherical aberration profile of the cornea. It goes without saying that pre-op dry eye management in optometry practice will help enhance measurements and post-op outcomes. Appropriate counselling for refractive surprise, the possible need for laser touch up, and/ or the need for spectacles is essential. These patients may not be suitable for trifocal IOLS due to corneal aberrations and the high risk of possible refractive surprise.
THE JUGGLE WITH SMALL PUPILS
Small pupils make cataract surgery more challenging for surgeons, due to limited visualisation increasing the risk of intraoperative complications (Figure 6, see also video at mieducation.com/cataract-in-optometry-practices-enhancing-patient-management). Various methods can be used to enlarge the pupil, including pharmacological mydriasis and/or enlarging devices such as iris hooks or pupil expanders. Inadequate dilation might result in iris trauma and photophobia.20 Operating with small pupils also increases the risk of intraoperative complications, such as loss of vitreous due to posterior capsular tear, anterior capsular tear, increased inflammation, irregular pupil shape, and/or retained lens material warranting another visit to the theatre. It might be prudent to assess and plan surgery appropriately, and avoid pupil dependent IOLS in these patients. Counselling by optometrists goes a long way in these patients who may need longer follow-up if there is underlying increased inflammation and or complication.
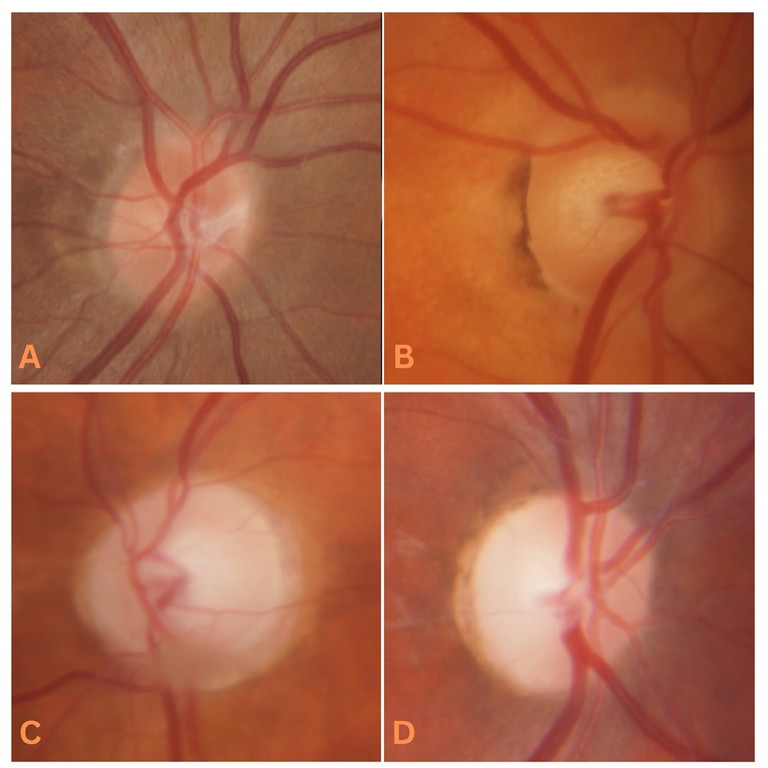
Figure 5. A) Healthy optic nerve head. B) Glaucoma suspect optic nerve head. C) Glaucomatous optic nerve head. D) Optic neuritis.
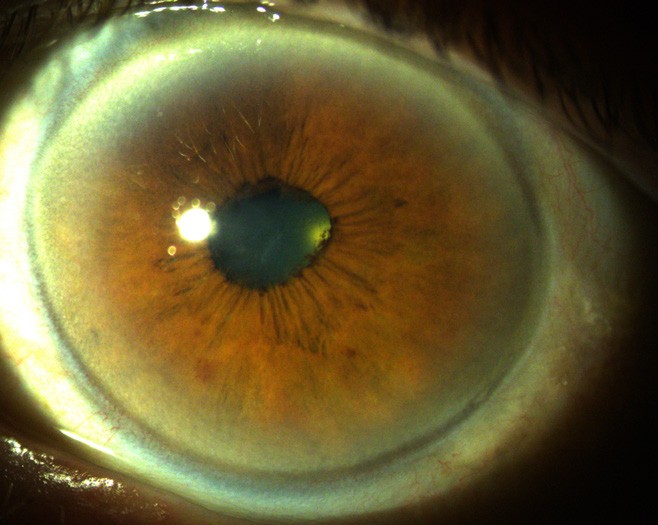
Figure 6. Cataract and small pupil with posterior synechiae.
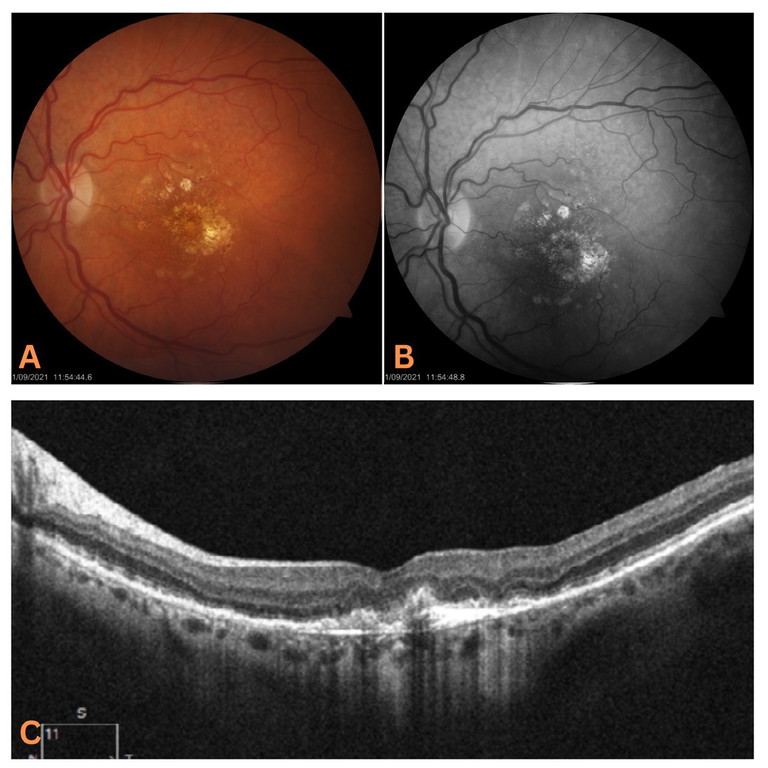
Figure 7. Fundus imaging of a patient with neovascular AMD and early geographic atrophy. A) Fundus photo. B) Red-free fundus photo. C) OCT cross section.
Intraoperative floppy iris syndrome (IFIS) was described by Chang and Campbell in 2005 and is associated with systemic use of alpha-1a receptor antagonist Tamsulosin (Flomax) for prostate hypertrophy.21 It causes atrophy of the iris dilator muscle and reduction of iris tissue rigidity. If appropriate precautions are not taken intra-operatively, complication rates can be up to 12.5% in these patients.21
OTHER CONTRAINDICATIONS
Not every patient is a suitable candidate for premium IOLs. Optometrists, being the first contact of patients, undertake a thorough screening process to assess the ocular health and visual potential of each eye prior to surgical referral. One of the key responsibilities in this process is identifying contraindications to multifocal or EDOF lens implantation.
Retinal history and examination are crucial. Patients with prior retinal tears, detachments, or laser treatment must be carefully evaluated. These individuals are at increased risk for future retinal complications and benefit from IOLs that allow optimal visualisation of the peripheral retina. Premium IOLs, particularly multifocal IOLs, can limit the surgeon’s view and complicate both diagnosis and treatment of posterior segment disease postoperatively. Multifocal IOLs with hydrophilic material are generally avoided in patients with moderate to advanced age-related macular degeneration (AMD) (Figure 7), diabetic macular oedema, retinopathy, pathologies that may require vitreoretinal surgery, or patients at risk of developing these conditions. This is in part due to the higher rates of dissatisfaction patients tend to demonstrate with these IOLs, but also due to the increased difficulty they can present for a surgeon during 22, 23 pars plana vitrectomy or epiretinal peeling.
Corneal health cannot be neglected in IOL selection. Scarring, opacities, and endothelial compromise reduce visual clarity and increase the risk of photic phenomena with multifocal optics. Patients with Fuchs’ endothelial dystrophy (FED), even in its subclinical stages, are often excluded from receiving premium lenses. However, some studies have found that patients with low grade FED were able to tolerate the increased photic phenomenon without significant impact on daily activities.24 In such cases, a monofocal IOL may offer more stable outcomes with happier satisfied patients. Again, it is essential to avoid hydrophilic material in patients who may need corneal graft at a later date.
COMPREHENSIVE PREOPERATIVE ASSESSMENT
Optometrists also conduct a thorough clinical examination to detect subtle contraindications and may provide detailed referrals along with patient education to assist with surgical planning. Slit lamp biomicroscopy allows for the assessment of cataract morphology, the presence of pseudoexfoliation, and the identification of lens instability. Fundus examinations and OCT imaging are essential for assessing macular health, optic nerve integrity, and detecting any early signs of comorbidity that may limit postoperative satisfaction. OCT imaging becomes indispensable as cataracts progress, and the fundus cannot be visualised with accuracy.
A well-documented VA history, combined with current refraction, offers valuable insight into the refractive stability and potential visual outcome following surgery. If a patient’s VA is deteriorating despite a relatively early cataract, this should prompt investigation into other causes, such as maculopathy or optic neuropathy. Patients should be made aware that cataracts are progressive and, if neglected, can lead to increased surgical complexity. More advanced cataracts are associated with greater variability in biometry, a higher risk of complications such as nucleus drop, slower recovery, and an elevated likelihood of cystoid macular oedema (CMO) and corneal oedema.25
POSTOPERATIVE MANAGEMENT AND LONG-TERM CARE
The conclusion of surgery is not the conclusion of care. Optometrists continue to play a central role in the patient’s postoperative journey. Many patients, if not all, return to their optometrists for follow-up assessments, particularly within the first month after surgery. During these visits, optometrists assess visual acuity, refraction, anterior segment health, and IOL positioning. Monitoring for inflammation, infection, and posterior capsular opacification (PCO) is essential during this period. Not all patients are immediately happy post-surgery, and optometrists play a key role in providing reassurance by managing ocular surface disease, residual refractive error, neuroadaptation, and/or photic phenomenon with multifocal IOLS.
In the longer term, optometrists remain responsible for the detection and management of new or progressive ocular conditions, including glaucoma, AMD, and diabetic retinopathy. Even patients with premium IOLs and good vision should continue to receive regular reviews. In many cases, patients may eventually require low-powered reading spectacles or fine-tuning of distance vision; and understanding the IOL type used is crucial for managing residual refractive errors.
“The contemporary cataract journey places the optometrist at its foundation”
Additionally, optometrists must be prepared to identify and manage any other issues that may arise, such as any retinal complications including tears/ vascular occlusions, progression of diabetic retinopathy and/ or AMD, CMO, and posterior capsular opacification (PCO). Recognising the signs of visual axis clouding, or unexplained visual decline, ensures timely referral for YAG capsulotomy or further evaluation.
CONCLUSION
The contemporary cataract journey places the optometrist at its foundation. From early diagnosis and patient education to detailed screening and long-term care, optometrists are essential to successful outcomes. As the options for IOL technology expand and patients become increasingly invested in achieving spectacle independence, the need for clear, accurate, and empathetic guidance grows.
By carefully evaluating ocular health, understanding individual visual needs, and managing expectations with honesty and insight, optometrists can help significantly improve both surgical outcomes and patient satisfaction. In doing so, they not only enhance the quality of vision, but also quality of life for cataract patients across the spectrum of care provided in their practice. Together we can achieve good outcomes by delivering customised care to each individual patient.
To earn your CPD hours from this article, visit mieducation.com/cataract-in-optometry-practices-enhancing-patient-management.
Associate Professor Smita Agarwal MBBS MS (Ophth) GradDipRefCatSurg FRANZCO is a senior comprehensive ophthalmologist based on the South Coast of New South Wales. She is a Clinical Associate Professor at the Graduate School of Medicine, University of Wollongong, and a Senior Lecturer at the University of Sydney, and Head of Ophthalmology in the Illawarra/ Shoalhaven region.
Assoc Prof Agarwal specialises in cataract and refractive surgery and has special interest in management options for keratoconus. She has published several research papers in peer-reviewed journals locally and overseas, and has been an invited speaker at prestigious ophthalmology meetings and seminars nationally and internationally.
References available at mieducation.com.