mi education
From Surface to Surgery:
Collaborating to Optimise the Tear Film for Surgical Precision
Successful cataract and refractive surgery begins well before the patient enters the operating theatre. As the eye’s first refractive surface, the tear film is critical for accurate biometry, clear intraoperative visualisation, and ultimately, surgical outcomes and patient satisfaction.1 Even subtle tear film instability can compromise preoperative measurements, increase the risk of refractive surprises, and diminish surgical outcomes.
In this article, ophthalmologist Dr Darian-Smith and optometrist Dr Margaret Lam discuss the benefits of collaboration between the professions ahead of surgery.
WRITERS Dr Erica Darian-Smith and Dr Margaret Lam
LEARNING OBJECTIVES
On completion of this CPD activity, participants should:
1. Understand the prevalence of dry eye disease, particularly in surgical candidates,
2. Realise the importance of early detection and intervention to optimise the tear film ahead of cataract and refractive surgery,
3. Be prepared to proactively screen for dry eye, and
4. Understand the need for ongoing collaborative care pre- and postocular surgery to improve patient outcomes.
A substantial proportion of surgical candidates present with clinical signs of dry eye disease (DED) yet remain asymptomatic. If left undetected, these patients face an increased likelihood of suboptimal surgical outcomes, postoperative discomfort, and dissatisfaction – even when the surgical procedure itself is technically successful.2
Addressing these challenges requires a proactive, collaborative approach. Optometrists, as the first point of contact for many patients, are well placed to detect and initiate tear film optimisation at the time of referral. Ophthalmologists, in turn, can build on these early interventions to reduce surgical delays, improve the reliability of biometric data, and ultimately enhance patient outcomes, satisfaction, and trust.
By working in partnership – integrating early identification, targeted optimisation, and coordinated post-surgical care – optometrists and ophthalmologists can deliver more predictable results, streamline the surgical pathway, and elevate the overall standard of patient care. Together, they can ensure that every patient enters surgery with a healthy, optimised tear film – optimising both surgical outcomes and patient experiences.
WHY PREOPERATIVE TEAR FILM MANAGEMENT MATTERS
Dry eye disease is highly prevalent, affecting 5–50% of the population and up to 63% in some groups, depending on diagnostic criteria and risk factors.3,4 Its impact spans both older cataract patients and younger refractive candidates. For many, contact lens intolerance driven by DED is a common reason for seeking laser vision correction, while surgical procedures themselves can also induce or exacerbate dry eye symptoms.5
Studies show that up to 80% of cataract patients present with at least one sign of ocular surface dysfunction prior to surgery, while preoperative symptoms have been reported in 38% of laser-assisted in situ keratomileusis (LASIK) and 48% of photorefractive keratectomy (PRK) patients in the refractive surgery population.6-10 Importantly, a large proportion of patients remain asymptomatic despite clinical indication of disease.6,8,11
With approximately 250,000 cataract procedures and thousands of refractive surgeries performed each year in Australia, proactive screening and optimisation of the tear film should be prioritised in practice.12-15 Clinicians may assume a reasonable probability of ocular surface disease – even when patients deny symptoms – making routine surface screening essential.5,6,16 Untreated DED in both symptomatic and asymptomatic patients can compromise preoperative measurements, reduce postoperative comfort, and may ultimately be the difference between a technically successful or truly satisfactory surgery.2,5,17
IMPACT ON BIOMETRY MEASUREMENTS AND POST-OP RESULTS
The precorneal tear film plays a pivotal role in the eye’s total refractive power, and even subtle instability can affect the accuracy of preoperative biometry.18 Whether planning cataract extraction, refractive procedures such as LASIK or PRK, or premium intraocular lens (IOL) implantation, precise preoperative measurements are essential for achieving optimal surgical outcomes. Tear film instability can:17-21
• Distort corneal power measurements and topography, leading to variable keratometry readings,
• Undermine IOL calculations, increasing the risk of postoperative refractive surprises – specifically, it can change the toricity of a lens and the axis of astigmatism, which can greatly impact on the final refractive outcome,
• Result in poor or fluctuating visual quality and, ultimately,
• Lower patient satisfaction, even when the surgery itself is technically successful.
As modern patients’ expectations increase, both preoperative tear film optimisation and ongoing postoperative maintenance have become integral to the surgical journey.
Achieving these outcomes requires close collaboration between optometrists and ophthalmologists, with optometrists playing a proactive role in early detection, management, and patient education. By prioritising tear film stability at every stage, clinicians can help ensure both the technical and experiential success of ocular surgery.
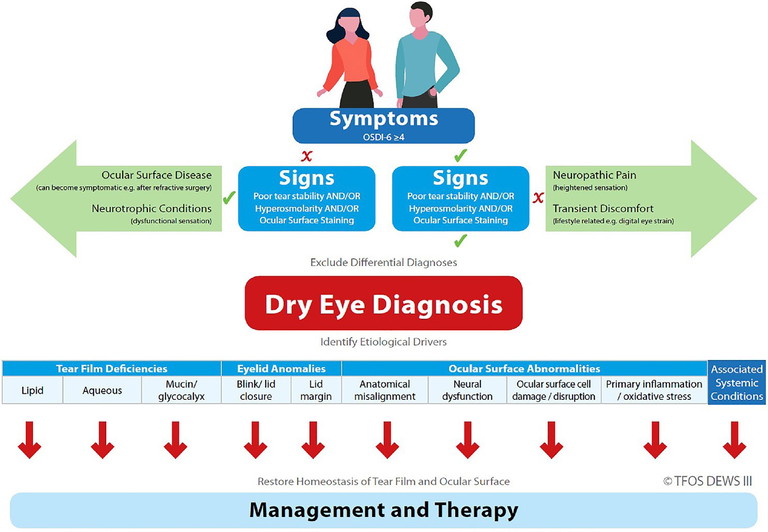
Figure 1. Dry eye disease management and therapy.22
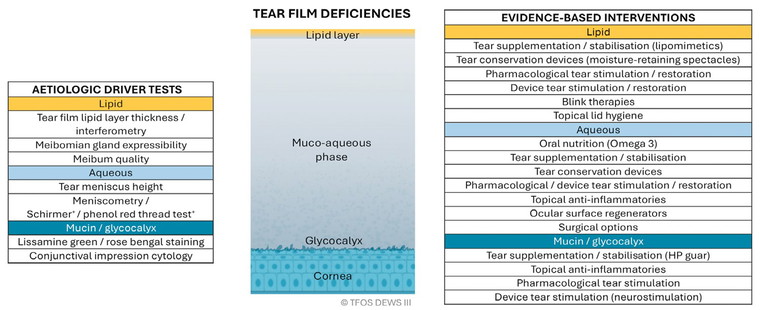
Figure 2. Tear film deficiencies.24
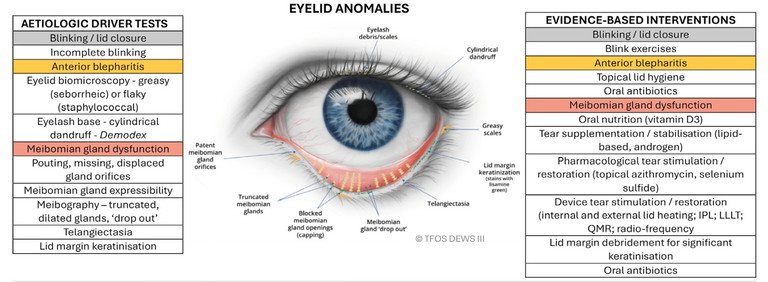
Figure 3. Eyelid anomalies.24
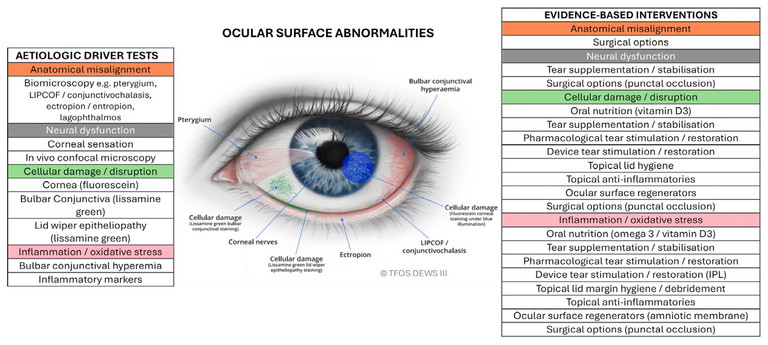
Figure 4. Ocular surface abnormalities.24
PREOPERATIVE DRY EYE DIAGNOSIS AND MANAGEMENT
Meeting patients’ high expectations for visual outcomes following surgery means addressing ocular surface disease before surgery. Optometrists are uniquely positioned to initiate optimisation of the ocular surface, supporting ophthalmologists in accurate surgical planning and enhancing patient satisfaction.
DED is multifactorial and can be challenging to manage but a systematic, evidence-based approach streamlines care. The TFOS DEWS II and III reports remain the gold standard, providing clear frameworks for both diagnosis and management.22-24
Practical preoperative screening tools include:22
• Symptom questionnaire: Ocular Surface Disease Index (OSDI-6) (score ≥4)
• Non-invasive tear break-up time (NITBUT): <10 seconds,
• Tear film osmolarity: ≥308 mOsm/L in either eye or interocular difference >8 mOsm/L,
• Ocular surface staining: >5 corneal fluorescein spots, >9 conjunctival lissamine green spots, or lid margin staining ≥2 mm length and ≥25% width.
A diagnosis is typically based on a positive symptom score plus at least one abnormal objective test (NITBUT, osmolarity, or staining). However, as many patients may exhibit significant ocular surface signs without symptoms, it is still recommended that these cases are managed proactively.22 It is also important to consider that heavy contact lens use can cause the cornea to become neuropathic to an extent, reducing the severity and type of symptoms that a patient may experience – even if clinical signs point towards moderate to severe ocular surface disease.
Practical Guidance on Preoperative Management
The results of a thorough dry eye evaluation are paramount in guiding treatment decisions before surgical referral. The updated TFOS DEWS III Management and Therapy report shifts the focus from a staged approach to achieving specific treatment goals, offering algorithms based on the clinically relevant drivers (Figure 1) of each patient’s condition.23,24
Subclassification and Targeted Management23,24
DED Subtypes. TFOS DEWS II and III emphasise subclassifying DED into aqueous-deficient (ADDE), evaporative (EDE), or mixed forms. Evidence suggests that approximately two-thirds of patients present with EDE.
Expanded Drivers. The latest TFOS DEWS III report recognises a broader spectrum of aetiological drivers – including tear film deficiencies, eyelid anomalies, and ocular surface abnormalities – requiring tailored diagnostic and therapeutic strategies (Figures 2–4).
Tailored Therapy. Distinguishing the dominant driver is critical for selecting effective interventions and optimising patient outcomes.
Management Principles23-24
• Preservative-free artificial tears (AT) remain a cornerstone of evidence-based DED management, providing tear supplementation and stabilisation.
• Lifestyle modifications and meibomian gland function optimisation are essential adjuncts.
• Concurrent management of multiple deficiencies is often necessary, as dry eye subtypes frequently overlap.
USE OF CATIONORM
When choosing an AT, an option to consider is Cationorm (CSL Seqirus). Cationorm is a preservative-free oil-in-water AT for DED that uses cationic emulsion (CE) technology.25 The unique formulation, with its positive-charge, is designed to be attracted to the negatively-charged ocular surface, optimising spread and residence time on the ocular surface without compromising on viscosity (Figure 5A).25 Unlike many other ATs, Cationorm targets all layers of the tear film (Figure 5B) and is suitable for the different subtypes of dry eye disease including evaporative, aqueous deficient and mixed.25-28
The efficacy of Cationorm for the treatment of DED has been demonstrated in several randomised, controlled, multicentre clinical trials.25,29-31 Evidence has also highlighted its specific value in the early postoperative period following refractive surgery, when tear film instability is common and recovery depends on ocular surface optimisation.
• In a study of 80 post-LASIK patients, Cationorm demonstrated significantly greater improvements in tear break-up time (TBUT) and patient-reported symptoms (dryness, irritation, burning) compared with Systane Ultra, with benefits evident by day 15 and maintained at one month.32
• In 129 patients undergoing transPRK or Epi-Bowman keratectomy (EBK), Cationorm was superior to 0.15% sodium hyaluronate for improving OSDI scores at both one week and one month. Patients using Cationorm also reported significantly less blurred vision after drop instillation.33
Together, these findings support Cationorm, not only as an effective treatment for DED in general, but also as a valuable choice for DED both before and after surgery to optimise tear film stability and support surgical recovery.
CASE STUDY: DR DARIAN-SMITH
Prior to refractive lens replacement or laser eye surgery, all patients at Eagle Eye Surgeons are optimised for surgery, with an important focus on dry eye for which we provide a comprehensive suite of treatments.
Even those that do not have considerable ocular surface disease need treatment prior to surgery for accurate diagnostic scanning. This is in the form of preservative free lubrication four times daily for a period of two to four weeks prior to surgery. Our preferred preservative free lubricant is Cationorm as it is effective in treating both evaporative and aqueous deficiency subtypes of dry eye. We couple this with Lacritec (Stiltec) for Omega 3 supplementation. In cases with pre-existing ocular surface disease, generally in heavy contact lens wearers, we add an addition of topical steroid such as FML (fluorometholone, AbbVie) four times daily for a month prior in a weaning dosage.
The benefits of priming our refractive patients with a preservative free lubricant such as Cationorm are numerous:
• The accuracy of keratometry readings on both corneal tomography and optical coherence tomography (OCT) devices (Pentacam and MS39) and biometry (IOL Master 700) are greatly improved. This affects the type of lens being inserted into the eye or, specifically for laser refractive surgery, the accuracy of the refraction being inputted into the laser.
• Postoperative comfort and prevention of the development of worsening dry eye after surgery. After surgery for both lens and refractive laser patients, preservative free lubricants are continued for a few months to aid with tear film regeneration. We couple this with custom-made preservative-free topical postoperative steroids and antibiotics. The tear film usually reverts to its preoperative baseline approximately six to eight weeks after surgery, so it is essential that lubrication continues until this disruption is restored.
“… as many patients may exhibit significant ocular surface signs without symptoms, it is still recommended that these cases are managed proactively”
A 52-year-old female was seen at our practice. She was undergoing assessment for suitability for Presbyond laser eye surgery, a type of refractive LASIK procedure combining the principles of optimisation of spherical aberrations coupled with micro-anisometropia, designed to remove the need for glasses for both distance and near.
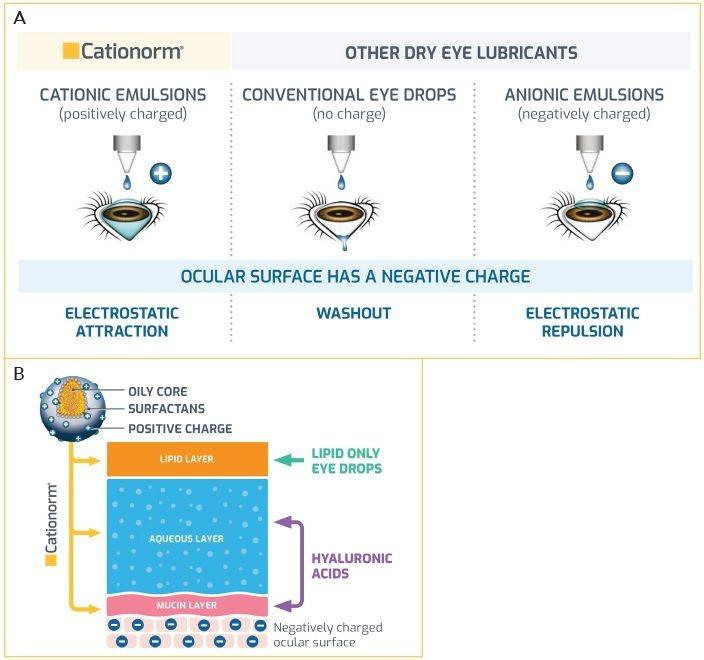
Figure 5. A) The advanced, positively-charged technology used in Cationorm is designed to enhance attraction to the negatively-charged ocular surface.25 B) The combination of an oily core, surfactants, positive charge and lubricants, enables Cationorm to address all layers of the tear film, making it suitable for aqueous deficient, evaporative and mixed dry eye.25-28
She was a heavy soft daily contact lens wearer for many years. Contacts were removed for a period of five days prior to the initial assessment. She was found to have a rapid TBUT (eight seconds) and mild aqueous deficiency dry eye with inferior superficial punctate epithelial erosions (SPEEs) 4–5. She was a low hyperope with presbyopia. A contact lens holiday was initiated, and the patient was asked to use Cationorm four times daily for a month, coupled with Lacritec. The patient returned four weeks later with a change in her prescription and importantly, a change in the axis of her astigmatism – the mild-moderate preoperative dry eye which was most likely contact lens induced had resolved with a tear film of 14 seconds and complete absence of SPEEs. The patient was booked for surgery, and the refraction was repeated on the day of surgery with no changes. The patient underwent routine bilateral Presbyond laser surgery. At the one week review she was 6/4.8-2 and J2 in both eyes. Despite undergoing LASIK, the preoperative drop regimen was continued for a period of eight weeks. The patient did not experience any discomfort or symptoms of ocular surface dysfunction. This case highlights the importance of preoperative optimisation of the ocular surface to ensure stability and accuracy of refractions, and also to ensure a safe laser outcome for our patients.
CONCLUSION
In summary, dry eye disease is common and potentially often underdiagnosed in surgical candidates. Proactive screening and management by optometrists – using evidence-based frameworks and close collaboration with ophthalmologists – are essential for optimising the tear film, improving surgical accuracy, and enhancing patient satisfaction. Early intervention and coordinated care set the foundation for successful outcomes in cataract and refractive surgery. And finally, while ocular surface optimisation upfront is critical, maintenance following the procedure remains equally vital.
This article is sponsored by CSL Seqirus. Drs Erica Darian-Smith and Margaret Lam were paid an honorarium by CSL Seqirus to author this article.
To earn your CPD hours from this article, visit: mieducation.com/from-surface-to-surgery-collaborating-to-optimise-the-tear-film-for-surgical-precision.
References available at mieducation.com.
Referral Checklist:
Ocular Surface Optimisation and Continuum of Care
FOR OPTOMETRISTS (PRE-REFERRAL)
□ Screen every surgical candidate for DED, regardless of symptoms.
□ Perform baseline testing (symptom questionnaire and at least one objective test: NITBUT, osmolarity, staining).
□ Identify exacerbating factors (contact lens overwear, systemic medications, environment).
□ Initiate targeted management (artificial tears, lid hygiene, meibomian gland optimisation, lifestyle changes). Consider artificial tears that target all layers of the tear film and preservative-free options to minimise corneal toxicity (e.g. Cationorm) and prescribe any other appropriate treatments, for example, warm compresses and Omega 3 supplementation.
□ Allow six to eight weeks of therapy prior to biometry, where possible.
□ Confirm ocular surface stability and readiness for referral for consideration for surgery.
FOR OPHTHALMOLOGISTS (AT REFERRAL AND PRE-SURGERY)
□ Review and build on optometrist’s optimisation plan.
□ Repeat/verify key surface tests before biometry.
□ Delay surgery if significant instability remains.
□ Discuss expectations with patient regarding DED management.
FOR SHARED POSTOPERATIVE CARE
□ Continue artificial tear/lid hygiene regimen post-surgery.
□ Monitor for exacerbation of DED symptoms.
□ Escalate therapy if recovery is delayed or symptoms worsen.
□ Maintain ongoing co-management for chronic dry eye.

Dr Erica Darian-Smith MBBS MMed GradDipRefCatSurg FRANZCO is an ophthalmologist specialising in refractive, cataract, and corneal surgery. She is Co-Founder and Director of Eagle Eye Surgeons, a boutique practice in two Sydney locations.
Trained at Prince of Wales Hospital in Sydney, she completed a two-year fellowship in corneal and refractive surgery and external eye diseases in Toronto, Canada. There, she gained subspeciality expertise in refractive surgery and treatment of all corneal diseases, including corneal transplants. Dr Darian-Smith is a fellow of the World College of Refractive Surgery and Visual Sciences and serves as a Visiting Medical Officer at Nepean Public Hospital in Sydney.

Dr Margaret Lam BOptom is Head of Optometry Services at 1001 Optometry in Bondi Junction and an Adjunct Senior Lecturer at the University of New South Wales’ School of Optometry and Vision Science. She practises full-scope optometry with a focus on myopia management, dry eye, and specialty contact lenses, including orthokeratology and keratoconus. She is a past National President of Optometry Australia.