mieducation
BCLA CLEAR Presbyopia:
Management with Intraocular Lenses
In our continuing series, encapsulating the relevant practice conclusions from the BCLA CLEAR Presbyopia publications, Dr Sandeep Dhallu provides an overview of the management of presbyopia with intraocular lenses (IOLs).
WRITER Dr Sandeep Dhallu
LEARNING OBJECTIVES
On completion of this CPD activity, participants should:
1. Understand the patient factors that can influence post operative success,
2. Be aware of intraocular lens technologies currently available and those in development,
3. Realise their advantages and disadvantages, and
4. Appreciate the need to understand patients’ needs and expectations, and evaluate visual performance.
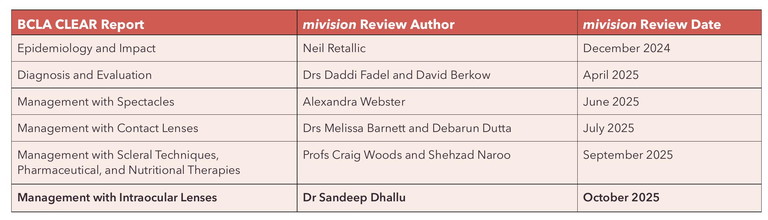
There is no single agreed standardised paradigm for the treatment of presbyopia. Instead, there are various management options available, including spectacle lenses, contact lenses, and refractive and surgical options, such as implantation with IOLs. The optimal presbyopia treatment option depends on several specific patient-related factors and these should be taken into consideration to achieve the best outcomes. These include the patient’s visual requirements (whether this be related to occupational needs or their leisure activities), their current and prior ocular health history, refractive and physical considerations, as well as age (Figure 1). Communication plays a vital role in gathering this information to reach the most appropriate management plan for each patient, based on their individual needs and aspirations.
Intraocular lenses have improved markedly in the past five decades and continue to be the focus of much research and development with novel lens designs and materials entering the market regularly. The cataract surgery procedure itself has also undergone refinement, and both of these developments have allowed better outcomes to be achieved by patients post-operatively. This article summarises the findings from the BCLA CLEAR Presbyopia series,1 on management with intraocular lenses, and readers are encouraged to read the full article for more detailed information.
COMMUNICATION
Good communication plays a fundamental role in the practitioner-patient relationship and can greatly influence patient success with the chosen management plan. Presbyopia can significantly impact a person’s quality of life, their self-esteem, work productivity, and overall psychological wellbeing.2 It is therefore important to explain to a patient, in lay-terms, what presbyopia is, as well as its progressive nature so that patients are able to understand how and why it may affect their ability to perform their usual everyday tasks. This is also an opportunity to alleviate any concerns or misconceptions they may have.
When discussing options for cataract surgery and IOLs, it is necessary to inform the patient of the complications associated with cataract surgery. However, it is just as important that they are aware of the specific complications that are more likely to occur with more advanced IOL designs, such as the risk of dysphotopsia. This is often explained either as a dark shadow or bright arcs, streaks or starbursts. Dysphotopsia can have a big impact on patient satisfaction postoperatively, especially if unanticipated.
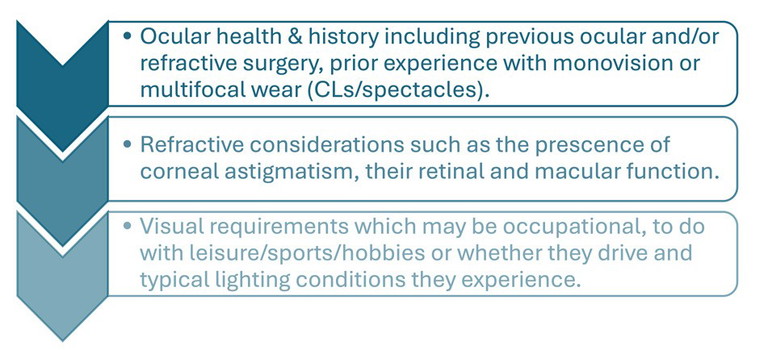
Figure 1. Some of the key patient factors to consider when selecting the optimal presbyopia correction for a patient.
PATIENT NEEDS AND EXPECTATIONS
Visual Requirements
Understanding the dynamic visual needs of every individual patient is key to patient success when considering the best presbyopia correcting option for them. This will vary according to factors such as occupation and hobbies, and it is important to ascertain what ‘distance’ is a priority as this will likely need to be enhanced. It is useful to determine how motivated the patient is to achieve spectacle independence, as this is one of the key drivers of patient satisfaction following presbyopia correcting IOL implantation.2 For instance, would the patient be willing to accept wearing spectacles for specific tasks such as driving, or very close work?
“it is just as important that they are aware of the specific complications that are more likely to occur with more advanced IOL designs, such as the risk of dysphotopsia”
It is equally important to have an awareness of any issues they may have had with any previous modes of correction. Those who have worn monovision and/or multifocal contact lenses previously may be better equipped to cope with the cons of this modality, such as the likelihood for photic phenomena, and therefore may be more likely to consider multifocal IOLs. Conversely, those who have had issues with contact lens wear previously may pose more of a problem and should be questioned further to determine the cause for this dissatisfaction, whether it be linked to discomfort arising from ocular surface issues, or vision-related intolerance such as haloes and glare. Both factors could indicate that the patient may be a less suitable candidate for multifocal or extended depth of focus (EDOF) IOLs.
Previous Surgery
Those who have undergone ocular or refractive surgery previously, and are used to spectacle independence, may have higher expectations for this after cataract surgery, and so may need to be counselled accordingly. What’s more, post-operative outcomes are less predictable in these patients and so special consideration is needed when selecting IOL power.3,4
OCULAR HEALTH ASSESSMENT
Corneal topography is a useful tool for mapping the corneal curvature and to help with IOL power calculations. Those with corneal astigmatism are less likely to achieve the best visual outcomes post-operatively, and it is important to identify and minimise corneal astigmatism when premium IOLs are to be used.5 Corneal tomography is perhaps a better option as it provides a more in-depth assessment with additional details, including corneal thickness and corneal shape.
Retinal and macular function are key factors that will influence visual outcomes, and how successful premium IOLs, such as multifocal and EDOF IOLs, may be. Ocular diseases such as age-related macular degeneration and diabetic retinopathy can compromise visual performance with these IOLs, and these patients may be better suited for monofocal lenses or possibly monovision correction.6
HISTORY OF INTRAOCULAR LENS DEVELOPMENT
Cataract surgery is the most commonly performed surgery in the UK, and indeed the world.7 Single vision or monofocal IOLs have long been implanted following cataract surgery, and are still the mainstay within the UK as they provide the most cost effective option for healthcare services. While a large proportion of patients opt for bilateral distance vision correction with monofocal IOLs, many others choose monovision.8 The use of monovision IOLs in refractive surgery has been practised from as early as 1984 with more established use since the mid 1990s.9
Multifocal IOLs were first implanted in the late 1980s and included both refractive and diffractive designs. Foldable IOLs gained popularity at a similar time and were transformative as they allowed smaller incisions to be made, thus resulting in better refractive outcomes. The first multifocal IOLs were made of polymethyl methacrylate (PMMA) and there were initial limitations relating to this material. Subsequent materials included silicone, which also had limitations, including a low refractive index, necessitating thicker lens profiles.
Modern lenses tend to be made of acrylic materials, which have higher refractive indices and so are thinner, therefore allowing a more controlled unfolding than silicone lenses.10 More recently, there have been advances in lens design including EDOF, trifocal, and light adjustable, as well as ‘accommodating’ designs.1
IOL DESIGNS
Monofocal
Standard single focus IOLs are currently the most widely implanted IOL type due to their relative low cost, good outcomes, and low incidence of photic phenomena.11 However, they do not allow for complete spectacle independence and typically provide good uncorrected vision at one focal point only – usually the distance. Thus, patients usually require corrective lenses for near and intermediate tasks. Aspheric optics can be added to an IOL to provide a wider range of vision.
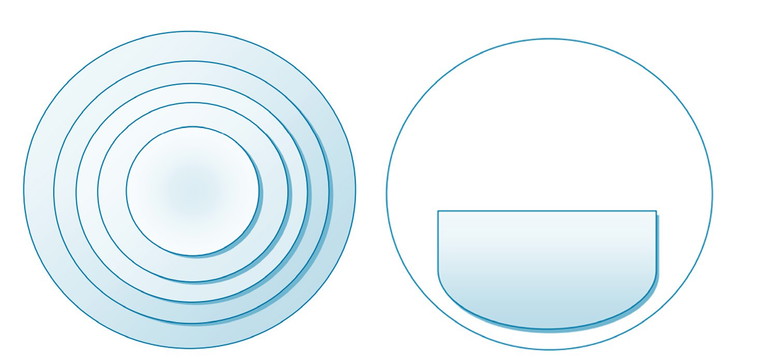
Figure 2. An example of a concentric ring design (left) and segmented (right) multifocal design.
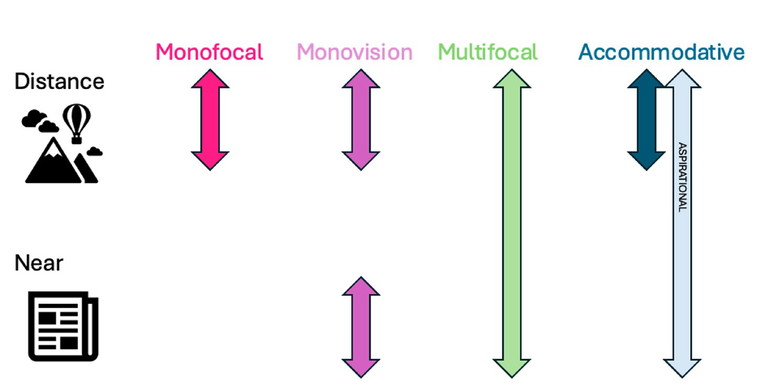
Figure 3. A comparison of the range of clear focus with different presbyopia correcting IOLs (adapted from BCLA CLEAR Presbyopia: ‘Management with Intraocular Lenses’).1
Pseudophakic monovision usually involves the dominant eye being corrected for distance vision and the non-dominant eye corrected for near to mid-range vision using traditional monofocal IOLs. However, the patient will be required to undergo neuroadaptation and so it is only recommended in those with good tolerance. As with laser refractive surgery (see BCLA CLEAR Presbyopia: ‘Management with Corneal Techniques’, section 2.612 ), a contact lens monovision trial is recommended prior to surgery to assess adaptation and tolerance. Other limitations of monovision include a reduction in stereoacuity, which is less affected in multifocal IOL designs.13
Multifocal
Refractive multifocal IOLs often include a concentric design, with zones of higher optical power focussing incoming rays of light for near vision overlayed onto the optic that gives distance vision. These IOLs are more prone to photic phenomena due to the numerous optical transitions present within the pupil area14 and this remains one of their main drawbacks. They are also more costly, can reduce contrast sensitivity, and require patients to undergo neural adaptation.15
More recently, segmented lenses have been developed that feature the near portion in a specific area of the IOL, much like in a bifocal spectacle lens (Figure 2). Segmented IOLs are rotationally asymmetric IOLs that rely on good centration as the distribution of light to the near segment depends upon the proportion of near segment within the pupil. They have been found to be more prone to optical quality degradation when decentred,16 but otherwise have a low incidence of glare and haloes and are somewhat comparable with monofocal IOLs in this regard. They have been reported to give good levels of vision and patient satisfaction.17
Diffractive designs use diffraction of light at a boundary to create multiple focal points, with the separation between ring edges determining the effective near addition power of the IOL. They can be apodised, whereby the step height is reduced gradually from the centre to the periphery to optimise light distribution between near, intermediate, and distance focal points, which is beneficial under varying light levels and pupil sizes. In fully diffractive multifocal IOLs, the concentric ring covers the entire central IOL optic and so the splitting of light is not affected by pupil size. Partially diffractive monofocal IOLs only incorporate this diffractive pattern over a specific area of the optic and so are more affected by pupil size.
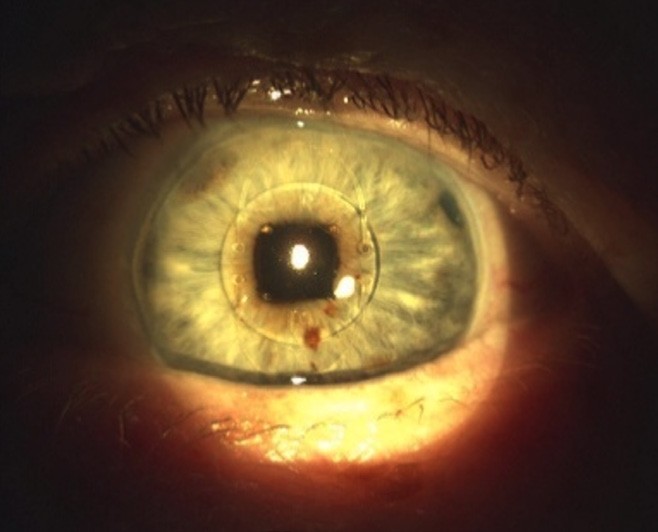
Figure 4. An iris peg lens with an iris clip.1
A comparison of refractive and diffractive IOLs suggested that eyes implanted with refractive multifocal IOLs showed better uncorrected distance and intermediate visual acuity, while eyes implanted with diffractive multifocal IOLs had better uncorrected near visual acuity with less photopic phenomenon.18 Surgeons can implant an IOL of different design or power in the second eye to extend the range of vision. For instance, multifocal IOLs can be combined with a different IOL design, like a segmented bifocal IOL to reduce photic phenomena.19
Accommodative IOLs
Accommodative IOLs should, by definition, demonstrate anatomically measurable changes in dioptric power, and have been in development for over two decades. Flexible haptic IOLs give a proposed increase in optical power due to a forward movement induced by lens capsule constriction.
However, while initial reports suggested a benefit to near visual acuity, the objectively measured accommodative range was minimal and reported to have declined over time due to lens fibrosis. Alternatives include dual optic designs, which achieve a wide accommodative range from separation between high plus-powered anterior and negative posterior optics, and variable focus IOLs, which are based on a lateral shift between two lenses.
Anatomical and physiological complication rates do not appear to differ between different multifocal IOLs20 or compared to monofocal IOLs, however more cases of posterior capsule opacification and the need for laser capsulotomy were reported in patients implanted with early accommodative IOLs. While a truly ‘accommodating’ IOL would be considered the holy grail for presbyopia, there is not enough evidence that current lenses are able to maintain a sustained change in optical power (Figure 3).
Phakic IOLs for Presbyopia
An alternative type of IOL is a phakic IOL, which does not require removal of the crystalline lens. Instead, the IOL may be introduced into the cornea (see BCLA CLEAR Presbyopia: ‘Management with Corneal Techniques’12 ) or in front of or behind the iris. Anterior chamber lenses can include designs like iris clip or iris peg lenses (Figure 4).
Initially, these IOLs were monofocal, but multifocal and toric designs have since been developed. They can be used alongside other treatments, such as laser refractive surgery so that less laser reshaping of the cornea is required in those with high refractive errors. However, there have been comparatively fewer presbyopia correcting designs developed for phakic IOLs, and disadvantages of these lenses include a risk of causing damage to the anterior chamber angle during surgery, secondary glaucoma, and possible traumatic cataract formation.
POST-OPERATIVE ASSESSMENT
There are several different measurements that can be taken following surgery to evaluate visual outcomes. These include measurement of visual acuity, particularly binocular visual acuity, to determine the level of close and intermediate vision and whether this is sufficient for that patient’s visual requirements. Binocular defocus curve testing, whereby visual acuity is measured through lenses of differing power, provides an important objective analysis of visual outcomes with multifocal IOLs.21 It is also useful to measure refractive error; while small residual refractive errors may be tolerated by the patient, larger uncorrected astigmatism or other ametropia are more problematic and may need to be addressed. Some IOL designs can reduce contrast sensitivity function, and so this is also a useful measure to take post-operatively.22
Subjective patient questionnaires can also be a good way to measure post-operative success. Social media has been shown to provide a valuable insight into the real-world perception of presbyopic patients, and is a useful resource that could perhaps be utilised further to gather greater insights into the lived experience of patients and widen our understanding of the expectations that patients have regarding presbyopia correction. One study, which analysed social media posts from patients with presbyopia, found that patient dissatisfaction following IOL implantation was largely related to needing glasses after surgery as well as the presence of visual disturbances, with complications and adverse events being the least discussed theme among patients.2 In cases where a patient is not satisfied with the outcome of multifocal IOL implantation, lens exchange with an alternative optical design or a monofocal IOL may be offered to relieve unsatisfactory visual outcomes.23
FUTURE DIRECTIONS
New IOL materials and designs are continually being developed, and recent examples include crosslinked polyisobutylene and a light-controlled refractive index material. Furthermore, femtosecond sculpted lens technology has been developed to alter the refractive index of an implanted IOL by adding water to a selected area, giving the potential to add and erase individualised multifocal optics. Other emerging developments and innovations include mechano-optoelectronic implants with their own energy supply and solar powered autofocus to be controlled with an app.1
“With an ageing population, the demand for presbyopia correction is rising, along with the need to develop new and innovative IOLs”
Top Tips for Eye Care Professionals
1. Use clear and effective communication when explaining what presbyopia is, its progressive nature, and the management options that are currently available, ensuring patient expectations are managed early.
2. Listen carefully to your patient’s individual visual requirements so that you have a good understanding of what tasks are most important for them, taking on board any past experiences (both positive and/or negative) with previous methods of correction.
3. Appreciate the limitations of each IOL type and decide whether these are likely to be tolerable for that patient.
4. Use a combination of subjective and objective measures when evaluating outcomes to gain a truer picture of post-operative success.
5. Stay up to date with new and emerging innovations.
SUMMARY
With an ageing population, the demand for presbyopia correction is rising, along with the need to develop new and innovative IOLs to keep pace with the ever-increasing visual demands of an increasingly digital world. The ability to continue using electronic devices is a key requirement for presbyopic patients. Understanding the patient’s current and future visual needs, while accounting for previous experiences, are key drivers for patient success; good communication between practitioner and patient is essential to ascertain this. Managing patient expectations about spectacle independence and the likelihood of visual disturbances is also crucial to minimise the risk of dissatisfaction. The breakout box above provides some key tips for eye care professionals on this exciting and evolving approach to presbyopia management.
To earn your CPD hours from this article, visit mieducation.com/bcla-clear-presbyopia-management-with-intraocular-lenses.
Acknowledgement and recognition to the authors of the original paper – Cristina Schnider, Leonard Yuen, Radhika Rampat, Dagny Zhu, Sandeep Dhallu, Tanya Trinh, Bharat Gurnani, Ahmed Abdelmaksoud, Gurpreet Bhogal-Bhamra, James S Wolffsohn, and Shehzad A Naroo.
The full report can be accessed at BCLA CLEAR Presbyopia: Management with Intraocular Lenses in Contact Lens and Anterior Eye (contactlensjournal. com). The report can also be accessed with the QR code.

This initiative was facilitated by the BCLA, with financial support by way of educational grants provided by Alcon, Bausch and Lomb, CooperVision, EssilorLuxottica, and Johnson and Johnson Vision.
The editors for this article series are Neil Retallic and Dr Debarun Dutta.
References
1. Schnider C, Yuen L, Naroo SA, et al. BCLA CLEAR presbyopia: Management with intraocular lenses. Cont Lens Anterior Eye. 2024;47(4):102253. doi: 10.1016/j.clae.2024.102253.
2. Zhu D, Dhariwal M, Zhang J, Smith A, Martin P. Patient perception and self-reported outcomes with presbyopia-correcting intraocular lenses (PCIOLs): A social media listening study. Ophthalmol Ther. 2024;13(1):287-303. doi: 10.1007/s40123-023-00840-8.
3. Li L, Yuan L, Yuan X, et al. Comparative analysis of IOL power calculations in postoperative refractive surgery patients: a theoretical surgical model for FS-LASIK and SMILE procedures. BMC Ophthalmol. 2023;23(1):416. doi: 10.1186/s12886-023-03164-0.
4. Pan X, Wang Y, Li Z, Ye Z. Intraocular lens power calculation in eyes after myopic laser refractive surgery and radial keratotomy: Bayesian network meta-analysis. Am J Ophthalmol. 2024;262:48-61. doi: 10.1016/j.ajo.2023.09.026.
5. Yeu E, Cuozzo S. Matching the patient to the intraocular lens: preoperative considerations to optimize surgical outcomes. Ophthalmology. 2021;128(11):e132-41. doi: 10.1016/j.ophtha.2020.08.025.
6. Hinnig RB, Martins LF, Penha FM. Spectral domain oct for screening of macular diseases prior to multifocal intraocular lens implantation. Int J Retina Vitreous. 2022;8(1):77. doi: 10.1186/s40942-022-00427-8.
7. Donachie PH, Barnes BL, Buchan JC, et al. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: Report 9, Risk factors for posterior capsule opacification. Eye (Lond). 2023;37(8):1633-9. doi: 10.1038/s41433-022-02204-1.
8. Bafna S, Gu X, Fevrier H, Merchea M. IRIS® Registry (Intelligent Research In Sight) analysis of the incidence of monovision in cataract patients with bilateral monofocal intraocular lens implantation. Clin Ophthalmol. 2023:3123-9. doi: 10.2147/opth.S424195.
9. Morgan PB, Efron N. Global contact lens prescribing 2000–2020. Clin Exp Optom. 2022;105(3):298-312. doi: 10.1080/08164622.2022.2033604.
10. Vacalebre M, Frison R, Fazio E, et al. Current state of the art and next generation of materials for a customized intraocular lens according to a patient-specific eye power. Polymers (Basel). 2023;15(6):1590. doi: 10.3390/polym15061590.
11. Hu JQ, Sarkar R, Afshari NA, et al. Cost-effectiveness analysis of multifocal intraocular lenses compared to monofocal intraocular lenses in cataract surgery. Am J Ophthalmol. 2019;208:305-12. doi: 10.1016/j.ajo.2019.03.019.
12. Craig JP, Barsam A, Kretz F, et al. BCLA CLEAR Presbyopia: Management with corneal techniques. Cont Lens Anterior Eye. 2024;47(4):102190. doi: 10.1016/j.clae.2024.102190.
13. Bohac M, Jagic M, Dekaris I, et aI. Stereoacuity and multifocal intraocular lenses – a systematic review. Acta Inform Med. 2023;31(1):62. doi: 10.5455/aim.2023.31.62-67.
14. Leyland M, Zinicola E. Multifocal versus monofocal intraocular lenses in cataract surgery: a systematic review. Ophthalmology. 2003;110(9):1789-98. doi: 10.1016/S0161-6420(03)00722-X.
15. Zhang L, Lin D, Lin H, et al. Comparison of visual neuroadaptations after multifocal and monofocal intraocular lens implantation. Front Neurosci. 2021;15:648863. doi: 10.3389/fnins.2021.648863.
16. Xu J, Zheng T, Lu Y. Effect of decentration on the optical quality of monofocal, extended depth of focus, and bifocal intraocular lenses. J Refract Surg. 2019;35(8):484-92. doi: 10.3928/1081597X-20190708-02.
17. Oshika T, Arai H, Inoue Y, Fujita Y. Five-year clinical outcomes of low-add-power segmented rotationally asymmetrical intraocular lens. Ophthalmol Ther. 2023;12(3):1649-56. doi: 10.1007/s40123-023-00703-2.
18. Shao D, He S. Meta-analysis of clinical randomized controlled trials comparing refractive with diffractive multifocal intraocular lenses in cataract surgery. [Zhonghua yan ke za Zhi] Chin J Ophthalmol. 2014;50(2):109-20.
19. Son HS, Khoramnia R, Auffarth GU, et al. Functional outcomes and reading performance after combined implantation of a small-aperture lens and a segmental refractive bifocal lens. J Refract Surg. 2019;35(9):551-8. doi: 10.3928/1081597X-20190806-02.
20. Zamora-de La Cruz D, Bartlett J, Gutierrez M, Ng SM. Trifocal intraocular lenses versus bifocal intraocular lenses after cataract extraction among participants with presbyopia. Cochrane Database Syst Rev. 2023(1) Art. No.: CD012648. doi: 10.1002/14651858.CD012648.pub3.
21. Buckhurst PJ, Wolffsohn JS, Shah H, et al. Multifocal intraocular lens differentiation using defocus curves. Invest Ophthalmol Vis Sci. 2012;53(7): 3920-3926. doi: 10.1167/iovs.11-9234.
22. Wolffsohn JS, Berkow D, Morgan PB, et al. BCLA CLEAR Presbyopia: Evaluation and diagnosis. Cont Lens Anterior Eye. 2024;47(4):102156. doi: 10.1016/j.clae.2024.102156.
23. Schallhorn JM, Schallhorn SC, Venter JA, et al. Incidence of intraoperative and early postoperative adverse events in a large cohort of consecutive refractive lens exchange procedures. Am J Ophthalmol. 2019;208:406-14. doi: 10.1016/j.ajo.2019.08.025.

Dr Sandeep Dhallu is a senior lecturer in optometry at the University of Hertfordshire in the United Kingdom. She is a registered optometrist, a Fellow of the Higher Education Academy, and a Fellow of the British Contact Lens Association. She has research interests in ocular nutrition, dry eye, and contact lenses.