mitechnology
Advancing Outcomes:
MS-39 AS-OCT & Osiris-T Aberrometer
WRITERS Dr Graham Furness and David Hsu

The Eyetek Osiris.
Advancement in technology plays a significant role in the evolution of clinical decision making. The quality of patient management can improve with the simple addition of a new piece of medical equipment. Dr Graham Furness describes the “notable influence” that two devices – the MS-39 AS-OCT and the Osiris-T aberrometer – have made to his cataract and refractive clinic.
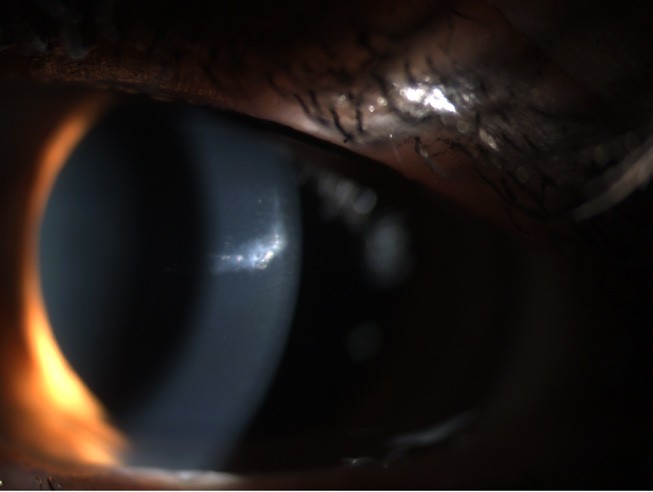
Figure 1A

Figure 1B
The MS-39 is an anterior optical coherence tomographer (OCT) with built-in placido disk corneal topography that generates detailed reports including epithelial thickness and point spread function maps. These features enable the early detection of corneal abnormalities, such as keratoconus, and enable the surgeon to visualise the severity of impact on the patient’s vision. Many built-in integrations, such as intraocular lens (IOL) calculations based on raytracing and laser in situ keratomileusis (LASIK) flap thickness mapping, are useful in a refractive clinic setting.
The Osiris-T is a corneal topographer with the ability to measure high-order aberrations across a whole eye. It provides a detailed analysis of the patient’s visual system and has simulation maps that allow for easy patient education on what can be a complex problem. Coupling the MS-39 and the Osiris-Tprovides a robust system for examining and managing anterior eye conditions.
The following two case studies demonstrate excellent outcomes enabled with these devices.
PENETRATING EYE INJURY
The first case is of a patient who had suffered a penetrating eye injury that resulted in a corneal scar (Figure 1A) and traumatic cataract (Figure 1B). The patient presented for a second opinion having been recommended a lamellar keratoplasty by their previous doctor.
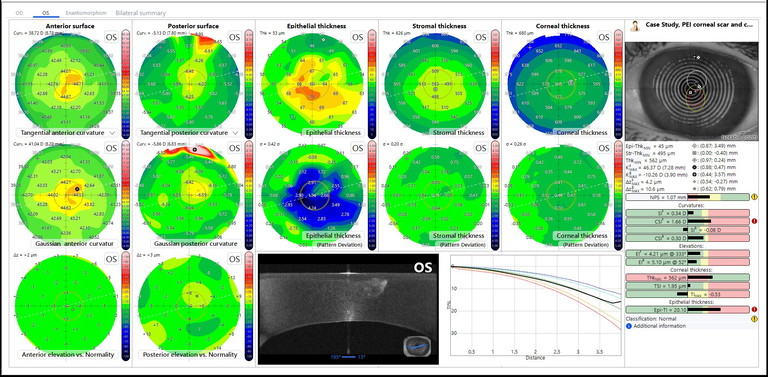
Figure 2
Corneal topography from the MS-39 (Figure 2) indicated a good recovery of the ocular surface profile. The unaided vision in the affected eye was 6/7.5, but the patient suffered from photopsia that would have been contributed by both the corneal and lenticular opacities. The Osiris-T was able to differentiate the effects of photopsia caused by the corneal scar and cataract.
Figure 3A is a report that demonstrates the ocular wavefront of the entire eye, which revealed that the patient was experiencing a wide variety of higher-order aberrations, particularly in coma and trifoil.
The point spread function (PSF) map represents the amount of light scatter induced when a single point of light is viewed through the ocular system. Figure 3B shows that PSF improves, but not entirely, when the patient corrects the lower order aberrations of defocus with prescription lenses.
A report of the patient’s corneal wavefront (Figure 3C), notably showed few higher-order aberrations and a much better PSF. This strongly suggests that the patient’s photopsia symptoms were mostly induced by the cataract and not from the corneal scar. Consequently, the patient proceeded with cataract surgery and achieved a 6/4.5 unaided outcome.
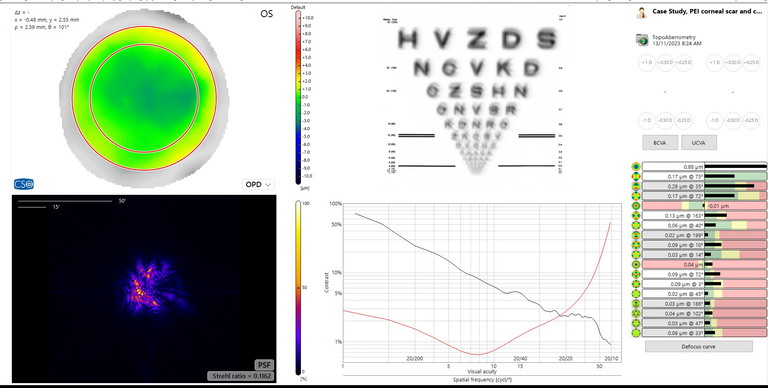
Figure 3A
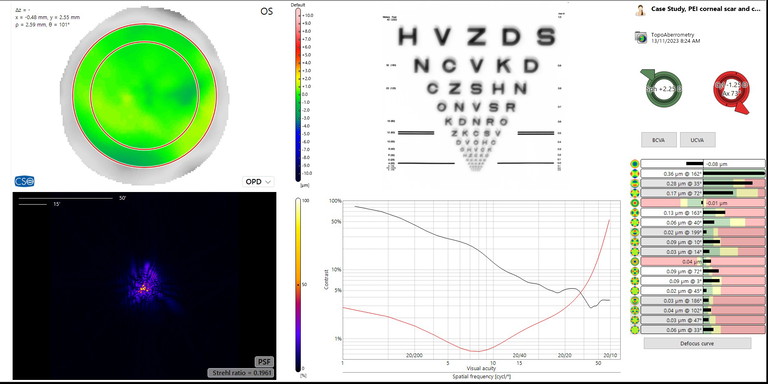
Figure 3B
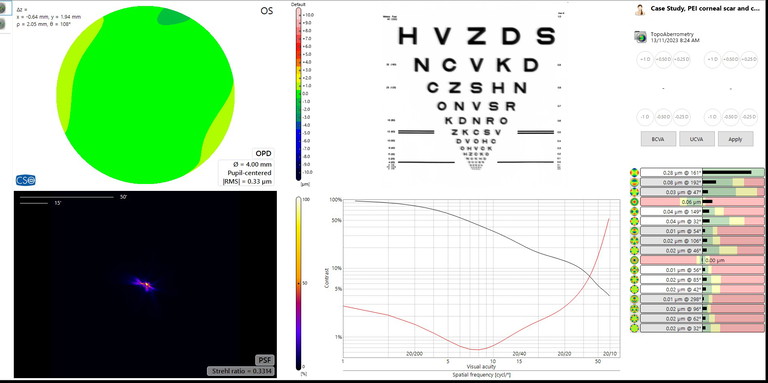
Figure 3C
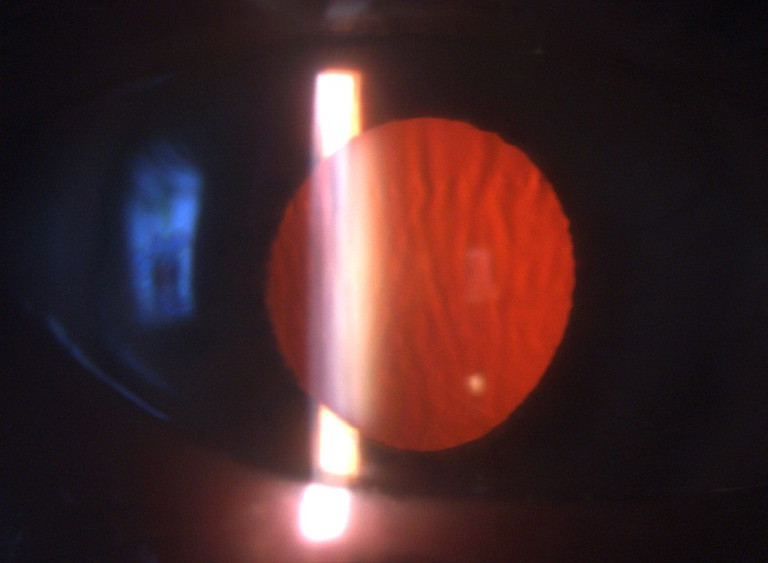
Figure 4A
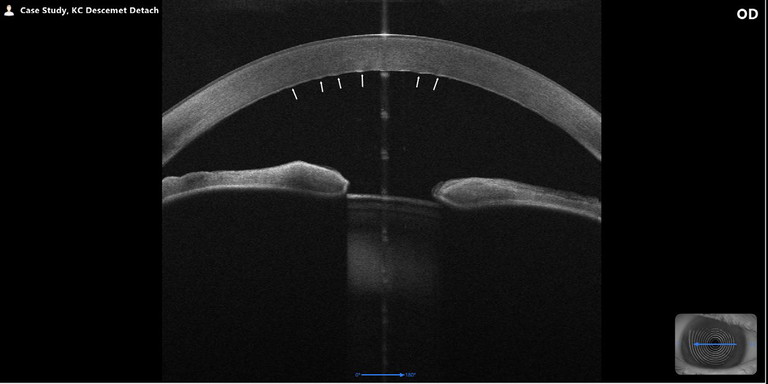
Figure 4B
DESCEMET’S MEMBRANE DETACHMENT
The second case is of a patient who was referred in for cataract surgery. The patient’s vision was R 6/18 L 6/15. Prominent bilateral vertical folds in Descemet’s membrane were identified (Figures 4A and 4B). The patient was unaware of a forceps birth, and obstetrical forceps-induced Descemet folds are typically unilateral and to the left eye due to the left occiput anterior foetal position being the most common during labour.1 Corneal topography suggested bilateral keratoconus due to the asymmetry in posterior corneal curvature.
The MS-39 has a specific keratoconus report that includes the typical topography maps, but also symmetry index curvatures and epithelial thickness maps (Figure 5). The symmetry index of the anterior curvature (SIF) and posterior curvature (SIB) measures the vertical asymmetry, where a positive value indicates a steeper inferior hemisphere compared to the superior hemisphere, while a negative value indicates a steeper superior hemisphere.2
Importantly, the MS-39 can also analyse epithelial thickness remodelling.
This keratoconus report can visualise compensatory epithelial thickening as the corneal stroma changes. Without the ability to measure epithelial thickness, it can be difficult to diagnose early stages of keratoconus as the compensatory thickening masks the irregular changes of the stroma, yielding a normal anterior surface. Typical keratoconus would usually show apical epithelial thinning with surround epithelial thickening. This patient’s epithelial thickness map was uniform with normal superior thinning due to eyelid mechanisms representing posterior keratoconus involvement.
However, endothelial guttata was also observed in both eyes, indicating that the patient had Fuch’s endothelial dystrophy with concomitant keratoconus. The concomitant nature of these corneal dystrophies is not unheard of. In a retrospective study of 138 patients with keratoconus, 8% of them were also found with the presence of corneal guttata.3 Corneal endothelial cell density typically ranges between 4,000 and 5,000 cells/mm2 at birth and decreases with age at an average rate of 0.45% per year, with an approximate value of 2,000–3,000 cells/mm2 in a normal adult eye,4 with the percentage of hexagonal cells expected to be 60%.5 In keratoconus, it is typical to have normal endothelial cell density, but with a decrease in hexagonal cells,3 and this was observed in our patient (R 2,588.1 cells/mm2 50% hexagonality L 2,199.7 cells/mm2 54% hexagonality).
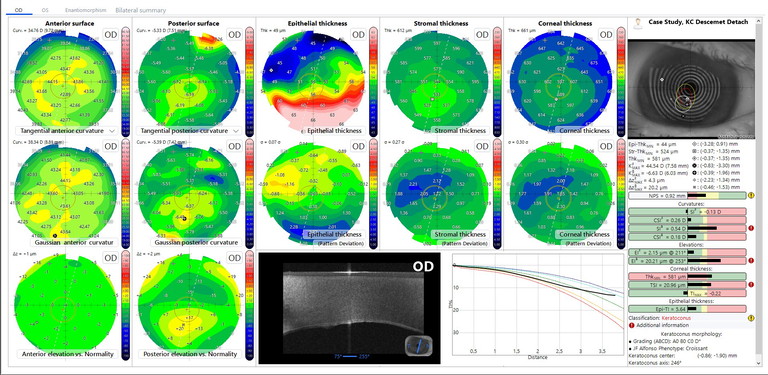
Figure 5
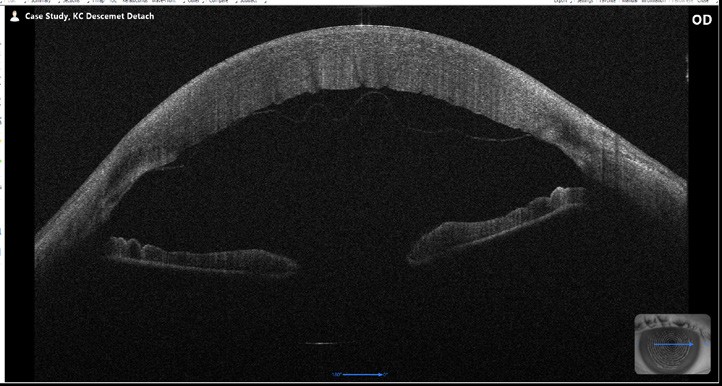
Figure 6
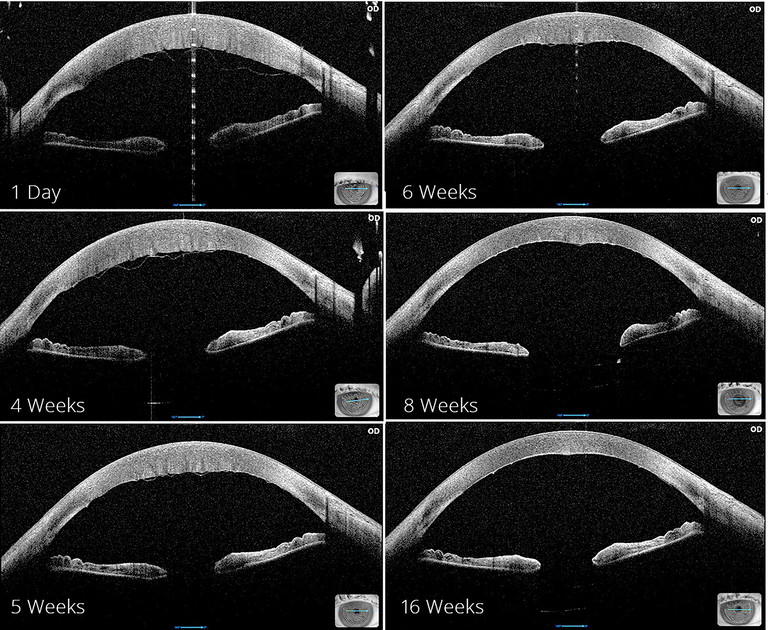
Figure 7
The patient was educated on his irregular cornea and was warned of a complex cataract surgery and an expected slow recovery. Intraoperatively, the Descemet’s membrane detached and was identified using the MS-39 A-OCT (Figure 6). Descemet’s membrane detachment is not uncommon, occurring in 43% of cataract operations.6 The majority are small detachments, at the peripheral site of corneal incisions, that will resolve without intervention, while 0.5% are large and involve the central cornea.7 Resolution without any intervention was unlikely for this patient, and consequently an anterior chamber air bubble was inserted, with the patient postured on their back for an extended period to encourage adhesion of the separated membrane. Rho-kinase inhibitor eye drops were also added to aid with corneal cell regeneration. The MS-39 was able to track the recovery process and the transformation was dramatic (Figure 7).
At 14 weeks post-operation, the patient’s unaided acuity was 6/9 and improved to 6/7.5 with pinhole.
EVIDENCE DRIVEN PATIENT OUTCOMES
These two case studies are recent examples of how modern technology has evolved our ability to make clinical decisions to deliver positive patient outcomes. Without the ability to assess whole eye aberrometry there is no other quantitative measurement that would definitively justify the benefits of cataract surgery in the first case. Similarly in the second case study, an anterior OCT was key in the prompt diagnosis and management of the Descemet’s membrane detachment.
This article was sponsored by Eyetek.
Dr Graham Furness is the founder and Medical Director of Insight Eye Clinic. He specialises in cataract and refractive surgery and was one of the first surgeons in Perth to regularly perform cataract surgery using the small incision technique under topical anaesthesia. He was a previous Chairman of the Perth Eye Hospital and currently serves as a Medical Advisory Board member.
David Hsu BVis Sci M.Optom is a clinical optometrist at Insight Eye Clinic with a special interest in ocular pathology and ophthalmic optics.
References available at mivision.com.au