mieducation
BCLA CLEAR Presbyopia:
Management with Scleral Techniques, Lens Softening, Pharmaceuticals, and Nutritional Therapies
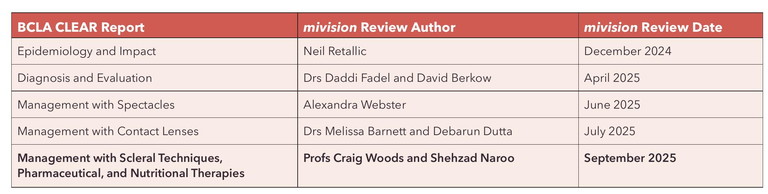
As part of the BCLA CLEAR presbyopia project, a group was formed to review the literature relating to the management of presbyopia by scleral and crystalline lens softening, as well as pharmaceutical and nutritional therapies. This group was led by Professor Shehzad Naroo, from Aston University.1 This article, the fifth of a series encapsulating significant conclusions from the BCLA CLEAR Presbyopia publications, was written by Professors Craig Woods and Shehzad Naroo.
LEARNING OBJECTIVES
On completion of this CPD activity, participants should:
1. Understand how the anatomy of the sclera changes with age, causing presbyopia,
2. Be aware of current and emerging treatments to soften the crystalline lens,
3. Comprehend current and emerging treatments to soften the sclera, and
4. Be aware of current and emerging treatments targeting miosis.
WRITERS Professor Craig Woods and Professor Shehzad Naroo
SCLERAL ANATOMY – CROSSLINKING AND RIGIDITY
The sclera consists of 90% type I collagen and 10% type III collagen; these collagen molecules are crosslinked to form fibrils and fibres. The rigidity of the sclera is created by the density of the crosslinking, which increases with age by the accumulation of advanced glycation end products. The bulk of the sclera also increases in thickness with age, effectively reducing its internal diameter. The combination of increased rigidity and diameter reduction impedes the dynamic processes that occur during accommodation, creating a lag and resistance to the movement phases of the ciliary muscle. This increasing rigidity also leads to a shift in the lens posture, adopting a more accommodated position instead of the fully relaxed flattened position. While the ciliary muscle retains the same contraction force found in a younger eye, the resistance of the sclera and the increased rigidity of the lens capsule contribute to the reduction in the dynamic range of focus of the eye, resulting in a loss of accommodation, i.e. presbyopia.2-6
The classic theory for the development of presbyopia is by Helmholtz, who suggested that the crystalline lens thickens and hardens with age over many decades, resulting in a diminished amplitude of accommodation. Recent studies have shown that with ageing, there is an increased rigidity in other surrounding tissues such as the sclera.5
Treatments that address these age-related changes to ocular rigidity were the focus of this BCLA CLEAR Presbyopia report. Strategies to reduce sclera rigidity and soften the crystalline lens to restore accommodation formed the main part of this report.
We have long known that improved near vision can be achieved by inducing myopia, preferably in the form of monovision, and from this literature review it became apparent that several systemic medications could lead to transient myopia, but only bilaterally. While this is most likely more of an unwanted side effect than a reason to use that medication, still, near vision would have been improved.
Finally, other management strategies were considered that led to an increase in the depth of focus of the eye, namely pharmaceutical and optical options.
TREATMENTS TARGETING THE CRYSTALLINE LENS
Mechanical Perspective
Femtosecond laser energy applied in a grid pattern produces micro-incisions within the lens peripheral tissue, splits lens fibres, and creates sliding plates by breaking bonds. This treatment is known as femtosecond lentotomy; it effectively softens the lens to restore accommodation. Promising in vitro studies have taken place on human donor and porcine crystalline lenses.7-11 However, further ongoing clinical results have not yet been reported and, at this stage, this is only considered suitable for the period prior to cataract removal.
“Poor nutrition and excessive exposure to ultraviolet light have been implicated in the early onset of presbyopia”
Therapeutic Perspective
Lipoic acid choline esters have been shown to chemically reduce disulphide bonds in the crystalline lens.12 These bonds are thought to be responsible for the progressive lens stiffening associated with presbyopia. A preclinical study with lipoic acid choline esters (Evo6 ophthalmic solution 1.5%) showed a dose dependant increase in lens elasticity and a reduction of protein disulphides in mice.13 However, a Phase 2 clinical trial involving 124 presbyopes failed to show a significant difference in binocular near visual acuity in humans between the test and the control groups at three months.14
Nutritional and Environmental Perspectives
Poor nutrition and excessive exposure to ultraviolet light have been implicated in the early onset of presbyopia. This BCLA CLEAR Presbyopia report reviewed whether nutritional approaches could sustain accommodation or delay presbyopia.
Astaxanthin. Considering nutritional supplements, astaxanthin, a red-orange cartenoid found in fish such as salmon, shrimp, and crabs, can act as an antioxidant in the human humour.15 On entering the crystalline lens, it has been shown to reduce sunlightrelated oxidative damage to the lens proteins.16
In a clinical trial, oral administration of astaxanthin 5 mg/day over four weeks as a supplement, resulted in an increase in accommodation amplitude from 2.3 ± 1.4D to 2.8 ± 1.6D, p<0.01 in comparison to a control group, where the change was 2.2 ± 1.0D to 2.3 ± 1.1D. There were 13 presbyopic participants in each study group.17
Combination supplements. In a randomised double-masked controlled trial, 24 presbyopic participants took a placebo and 24 presbyopic participants took a dietary supplement for four weeks. The supplement consisted of a daily dose of lutein 10 mg, astaxanthin 4 mg, bilberry extract 20 mg, black soybean hull extract 26.5 mg, and docosahexaenoic acid 50 mg. The near point of accommodation increased to 1.32 ± 0.39 D for the intervention group compared to 0.11 ± 0.34 D for the placebo group.18
TREATMENTS TARGETING SCLERAL TISSUE
Laser Scleral Microporation
Laser scleral microporation (LSM) was previously known as laser anterior ciliary excision (LaserACE).19 In this procedure, four ocular fornix-based peritomies are performed, whereby ablations are applied to the scleral tissue starting 0.5 mm posterior to the limbus to an 80% depth.
For LSM, a YAG (yttrium aluminium garnet) laser with a fibre optic probe generates a spot lesion 600 microns in diameter and is used to generate the nine micro-excisions in the four oblique quadrants. These micro-excisions are performed in three critical zones over the ciliary complex to increase the pliability of the sclera (pliable matrix zones, Figure 1). The goal is to reduce the scleral rigidity and thus restore the mechanical efficiency of the natural accommodation mechanism and increase accommodation; the dynamic range of focus (DRoF). In a study involving elderly monkeys with seven-month post-procedure follow-up, an increase in the DRoF was demonstrated (Figure 2). This treatment has been demonstrated as repeatable and increasingly effective with age. Because this procedure does not affect change to the cornea or crystalline lens, and is repeatable over time, it holds significant promise.
Scleral Expansion Based Treatment
This treatment is based on Schacher’s theory for presbyopia,21 where it is suggested that the narrowing of the circumlenticular space, due to the increasing lens diameter and reduction in the internal scleral diameter associated with age, results in a loss of ciliary zonule tension. To address this, four small strips of poly(methyl methacrylate) (PMMA) are quadrantally inserted into the sclera with the goal to expand the scleral diameter. This scleral expansion widens the sclera’s internal diameter and thus the circumlenticular space, restoring the ciliary zonule tension and accommodation. A two-year clinical trial reported that 80% of the 344 participants achieved a distance corrected near visual acuity of 20/40 at 40 cm by 24 months. Data collection is currently ongoing for the 36-month time point.22
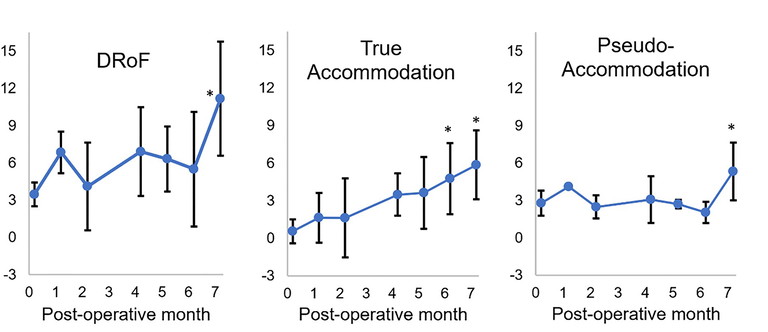
Figure 1. The pliable matrix zones with zones one to three being of clinical significance.1
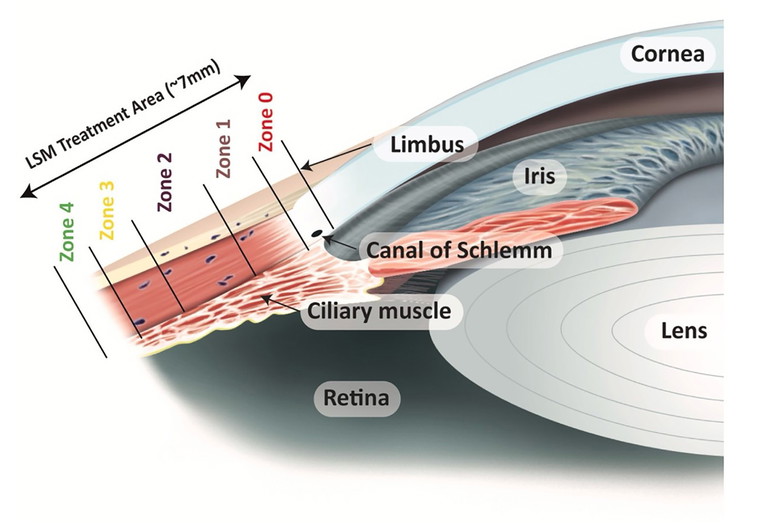
Figure 2. Dynamic range of focus (DRoF), true accommodation, and pseudoaccommodation in monkeys treated with laser scleral microporation. True accommodation improved steadily after treatment. * = timepoints differ significantly from baseline. Figure adapted from Ting et al. 2022.20
PHARMACEUTICAL TREATMENTS TARGETING THE PUPIL, MIOSIS
A miotic pupil increases the depth of field of the eye but also causes a loss of retinal illumination.23 Pilocarpine ophthalmic, a cholinergic agonist, has long been used to induce miosis, most commonly in the management of glaucoma.24 However, pilocarpine has well-documented side effects of headache, stinging on insertion, ocular redness, poor night vision, refractive error changes, and an increased risk of retinal detachment. In one case series report, it was noted that when pilocarpine had been used to reverse mydriasis in a young population, it resulted in temporarily induced myopia.25
There has been recent interest in using pilocarpine to increase the depth of focus of the eye to manage presbyopia. One study demonstrated that over 30 days, an improved near vision efficacy occurred using the 1.25% concentration.26 In October 2021, Vuity 1.25% (pilocarpine HCI ophthalmic solution) was approved by the United States Food and Drug Administration for the treatment of presbyopia. Currently, in development by Ocuphire Pharma is a combination drop containing phentolamine ophthalmic solution (0.75%) along with pilocarpine (0.4%). This combination drop was able to demonstrate significant improvement in unaided near vision for up to six hours post-instillation.27
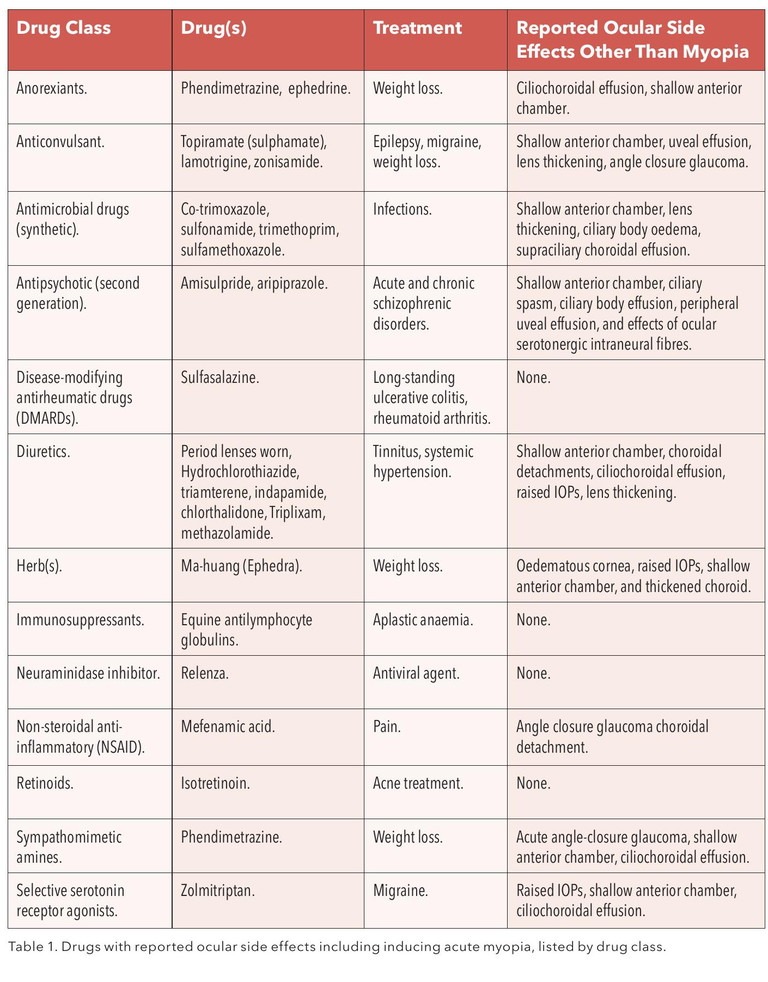
Incidental Systemic Pharmaceutical Effects: Inducing Myopia
Finally, presbyopia could be managed by inducing myopia. While this would obviously impact distance vision, near vision would be improved. The ideal mechanism would be to induce myopia unilaterally, thus creating monovision. A series of published case reports highlighted several systemic drugs that included bilateral transient myopia as a side effect, thus improving near vision. While myopia was induced, it is important to note this was likely an unwanted side effect and was often just one of many other unwanted, more serious side effects, as shown in Table 1.
IN SUMMARY
The ophthalmic community has been trying to manage presbyopia for centuries and in this BCLA CLEAR Presbyopia report some of the less mainstream solutions, as distinct from the main core optical aids, i.e. spectacles, contact lenses or intraocular lenses, were reviewed – particularly those targeting the sclera and the crystalline lens. New treatments are emerging to reduce the rigidity of the sclera or soften the crystalline lens, but as yet all are in the early development phases. This BCLA CLEAR Presbyopia report provided a summary of the scientific evidence that is available for these novel management strategies.
Some of these treatments do show promise, such as laser scleral microporation, to effectively reduce scleral rigidity while demonstrating good safety. Scleral expansion bands do not appear to have shown the expected promise, and no further research has been reported. Studies of lens softening with a femtosecond laser appear to have been halted. Regarding pharmacological management, the majority of research relates to the maintenance of a miotic pupil. The goal of the miosis is to increase the depth of focus while being independent of luminance; the predominant agent being pilocarpine.
Tips for Practice
• This paper details treatments for presbyopia that are at the fringes of current practice and based on emerging evidence.
• Treatments such as the use of pilocarpine that increase the depth of focus of theeye are commercially available.
• Treatments that ‘soften’ the sclera and crystalline lens are still in development and show promise.
• Treatments that expand the circumlenticular space still need stronger evidence to confirm efficacy.
• Practitioners should be aware of these novel ideas as they may see patients who have undergone these procedures.
• Some of these techniques will re-emerge in future as methods to manage patients with presbyopia.
“New treatments are emerging to reduce the rigidity of the sclera or soften the crystalline lens, but as yet all are in the early development phases”
To earn your CPD hours from this article visit mieducation.com/bcla-clear-presbyopiamanagement-with-scleral-techniques-lenssoftening-pharmaceutical-and-nutritional-therapies.
Acknowledgement and recognition to the authors of the original paper: Naroo SA, Woods CA, GilCazorla R, Ang RE, Collazos M, Eperjesi F, Guillon M, Hipsey AM, Jackson MA, Price ER, and Wolffsohn JS.
This initiative was facilitated by the BCLA, with financial support by way of educational grants provided by Alcon, Bausch and Lomb, CooperVision, EssilorLuxottica, and Johnson and Johnson Vision. The editors for this article series are Neil Retallic and Dr Debarun Dutta.
The full article can be accessed at pubmed.ncbi. nlm.nih.gov/39098809 or by following the QR code.

References
1. Naroo SA, Woods CA, Wolffsohn JS, et al. BCLA CLEAR presbyopia: Management with scleral techniques, lens softening, pharmaceutical and nutritional therapies. Cont Lens Ant Eye. 2024;47(4):102191. doi:10.1016/j.clae.2024.102191
2.Fisher RF. Presbyopia and the changes with age in the human crystalline lens. J Physiol. 1973 Feb;228(3):765-79. doi: 10.1113/jphysiol.1973.sp010111.
3. Koopmans SA, Terwee T, Kooijman AC, et al. Polymer refilling of presbyopic human lenses in vitro restores the ability to undergo accommodative changes. Invest Ophthalmol Vis Sci. 2003 Jan;44(1):250-7. doi: 10.1167/iovs.02-0256.
4. Zhou H, Yan H, Yan W, Wang X, Li Q. In vivo ultraosound elastographic evaluation of the age-related change of human lens nuclear stiffness. BMC Ophthalmol. 2020 Apr 6;20(1):135. doi: 10.1186/s12886-020-01404-1.
5. Detorakis ET, Pallikaris IG. Ocular rigidity: biomechanical role, in vivo measurements and clinical significance. Clin Exp Ophthalmol. 2013 Jan-Feb;41(1):73-81. doi: 10.1111/j.1442-9071.2012.02809.x.
6. Hipsley AM, Chapter 41; VisioDynamics theory: A biomechanical model for the aging ocular organ. In Mastering the techniques of presbyopia surgery. 2006 Jaypee digital. doi: 10.5005/jp/books/10508_41.
7. Schumacher S, Oberheide U, Lubatschowski H, et al. Femtosecond laser induced flexibility change of human donor lenses. Vision Res. 2009 Jul;49(14):1853-9. doi: 10.1016/j.visres.2009.04.028.
8. Krueger RR, Sun XK, Stroh J, Myers R. Experimental increase in accommodative potential after neodymium: yttrium-aluminum-garnet laser photodisruption of paired cadaver lenses. Ophthalmology. 2001 Nov;108(11):2122-9. doi: 10.1016/s0161-6420(01)00834-x.
9. Hahn J, Fromm M, Krüger A, et al. Measurement of ex vivo porcine lens shape during simulated accommodation, before and after fs-laser treatment. Invest Ophthalmol Vis Sci. 2015 Aug;56(9):5332-43. doi: 10.1167/iovs.14-16185.
10. Zhang J, Wang R, Gu Y, et al. Safety evaluation of femtosecond lentotomy on the porcine lens by optical measurement with 50-femtosecond laser pulses. Lasers Surg Med. 2013 Sep;45(7):450-9. doi: 10.1002/lsm.22154.
11. Ripken T, Oberheide U, Lubatschowski H, et al. fs-Laser induced elasticity changes to improve presbyopic lens accommodation. Graefes Arch Clin Exp Ophthalmol. 2008 Jun;246(6):897-906. doi: 10.1007/s00417-007-0699-x.
12. Korenfeld MS, Robertson SM, Burns W, et al. Topical lipoic acid choline ester eye drop for improvement of near visual acuity in subjects with presbyopia: a safety and preliminary efficacy trial. Eye (Lond). 2021 Dec;35(12):3292-3301. doi: 10.1038/s41433-020-01391-z.
13. Garner WH, Garner MH. Protein disulfide levels and lens elasticity modulation: Applications for presbyopia. Invest Ophthalmol Vis Sci. 2016 May 1;57(6):2851-63. doi: 10.1167/iovs.15-18413.
14. UNR844. A study of safety and efficacy of UNR844 chloride (UNR844-Cl) Eye drops in subjects with presbyopia. 2019 [cited 2024 April]. Clinical Trial Repository]. Available at: classic.clinicaltrials.gov/ct2/show/NCT03809611.
15. Hashimoto H, Arai K, Obara Y, et al. Effects of astaxanthin on antioxidation in human aqueous humor. J Clin Biochem Nutr. 2013 Jul;53(1):1-7. doi: 10.3164/jcbn.13-6. Epub 2013 May 18.
16. Wu TH, Liao JH, Hu CC, et al. Astaxanthin protects against oxidative stress and calcium-induced porcine lens protein degradation. J Agric Food Chem. 2006 Mar 22;54(6):2418-23. doi: 10.1021/jf052651q.
17. Nagaki Y, Hayasaka S, Uonomi T, et al. Effects of astaxanthin on accommodation, critical flicker fusion, and pattern visual evoked potential in visual display terminal workers. J Tradit Med 2002;19:170–3.
18. Kono K, Shimizu Y, Yui K, et al. Effect of multiple dietary supplement containing lutein, astaxanthin, cyanidin-3-glucoside, and dha on accommodative ability. Curr Med Chem. 2014 Aug;14(2):114–25. doi: 10.2174/187152221402150408111137.
19. Hipsley A, Ma DH, Sun CC, Jackson MA, Goldberg D, Hall B. Visual outcomes 24 months after LaserACE. Eye Vis (Lond). 2017;4:15. doi: 10.1186/s40662-017-0081-y.
20. Ting DSJ, Liu YC, Mehta JS, et al. Improvement in accommodation and dynamic range of focus after laser scleral microporation: A potential treatment for presbyopia. Transl Vis Sci Technol. 2022 Dec 1;11(12):2. doi: 10.1167/tvst.11.12.2.
21. Davies LN, Biswas S, Wolffsohn JS, et al. BCLA CLEAR presbyopia: Mechanism and optics. Cont Lens Anterior Eye. 2024 Aug;47(4):102185. doi: 10.1016/j.clae.2024.102185..
22. VisAbility. A Clinical Trial of The VisAbility Micro Insert System for Presbyopic Patients [cited 2024 April]. Clinical Trial Repository]. Available at: classic.clinicaltrials.gov/ct2/show/NCT02374671.
23. Mathôt S. Pupillometry: psychology, physiology, and function. J Cogn. 2018 Feb 21;1(1):16. doi: 10.5334/joc.18.
24. Haghpanah N, Alany R. Pharmacological treatment of presbyopia: A systematic review. Eur J Transl Myol. 2022 Sep 19;32(3):10781. doi: 10.4081/ejtm.2022.10781.
25. Gilmartin B, Amer AC, Ingleby S. Reversal of tropicamide mydriasis with single instillations of pilocarpine can induce substantial pseudo-myopia in young adults. Ophthalmic Physiol Opt. 1995 Sep;15(5):475-9. PMID: 8524578.
26. Price FW Jr, Hom M, Wirta DL, et al. Combinations of pilocarpine and oxymetazoline for the pharmacological treatment of presbyopia: Two randomized phase 2 studies. Ophthalmol Sci. 2021 Oct 2;1(4):100065. doi: 10.1016/j.xops.2021.100065.
27. Pepose JS, Kolli A, Patel R, Rahmani K, Sooch M, Brigell MG, et al. The efficacy of phentolamine ophthalmic solution and low-dose pilocarpine to improve distance-corrected intermediate visual acuity in patients with presbyopia. Invest Ophthalmol Visual Sci 2022;63(7):1809 – F0425-1809 – F0425.
Craig A Woods BSc(Hons) PhD GCertOcThera MCOptom FAAO FBCLA is an adjunct Professor, School of Optometry, University of New South Wales, a clinical consultant for Zeiss Vision Care, the Executive Manager of Educational Development for the International Association of Contact Lens Educators, and President Elect of the International Society for Contact Lens Research. He is also a member of the editorial boards for both the Contact Lens and Anterior Eye and Eye and Contact Lens journals. He has authored over 200 refereed and professional papers and text-book chapters in related fields of ocular surface disease and contact lenses.

Shehzad A Naroo BSc(Hons) MSc PhD FIACLE FAAO FBCLA FEAOO FCOptom SFHEA is a Professor of Investigative Ophthalmology and Optometry at Aston University (UK). He teaches and researches around the topic of anterior eye. Prof Naroo is Editor-in-Chief of the BCLA journal Contact Lens and Anterior Eye. He is the former President of the International Association of Contact Lens Educators (IACLE) and now serves as Vice-President. He is a past recipient of the World Council of Optometry International Optometrist Award, in recognition of this philanthropic work in countries with less developed health care systems. He is the West Midlands Regional Lead Hospitaller to the St John’s Eye Hospital in Jerusalem. Prof Naroo graduated optometry at Aston University and did his MSc and Phd in Manchester. He has authored over 200 refereed and professional papers.