mieducation
Do No (Ocular Surface) Harm: How to Uncover Iatrogenic Dry Eye
Dry eye disease (DED) is a multifactorial disorder of the ocular surface, characterised by a loss of tear film homeostasis and accompanied by ocular symptoms such as discomfort, visual disturbance, and poor tear film stability.1 Based on the predominant underlying disease mechanisms, DED is traditionally classified into two main subtypes – aqueous-deficient dry eye (ADDE) and evaporative dry eye (EDE).1 But regardless of aetiology, both forms perpetuate a vicious cycle of tear film instability and hyperosmolarity, ultimately leading to ocular surface inflammation.2
Dr Ally Xue and Helen Gleave discuss the causes of iatrogenic dry eye and how you can mitigate their adverse effects on the ocular surface to improve patient quality of life.
WRITERS Dr Ally Xue and Helen Gleave
LEARNING OBJECTIVES
On completion of this CPD activity, participants should:
1. Be able to identify common causes of iatrogenic dry eye,
2. Know how to mitigate their adverse effects on the ocular surface,
3. Recognise the influence of blinking patterns and East Asian eyelid morphology on dry eye, and
4. Be aware of the role of hyaluronic acid in commercial eye drop formulations and its implication for iatrogenic dry eye.
Dry eye is one of the most common reasons patients seek eye care, which is unsurprising given DED affects millions of people worldwide, with prevalence rates reported to be as high as 50%.3 As healthcare professionals, we strive to manage and alleviate our patients’ symptoms. However, it is important to acknowledge that medical interventions themselves can sometimes inadvertently contribute to the onset or worsening of the condition – a phenomenon known as iatrogenic dry eye.4
Thanks to the work of the Tear Film and Ocular Surface Society (TFOS), most clinicians are now familiar with the importance of tailoring dry eye management based on a patient’s position along the aqueous deficient dry eye (ADDE) to evaporative dry eye (EDE) spectrum. In 2017, the TFOS Dry Eye Workshop II (DEWS II) notably highlighted iatrogenic dry eye in its reports, reflecting its growing prevalence.4 Iatrogenic dry eye refers to ocular surface disease that is unintentionally caused by medical examination or treatments, including topical or systemic medications, contact lens wear, ocular surgeries, and aesthetic procedures. Additionally, current research indicates that East Asian populations may be more vulnerable to these risk factors.3,5,6 Therefore, an understanding of these contributors is essential for the effective prevention and management of iatrogenic dry eye.
WHAT ARE COMMON CAUSES OF IATROGENIC DRY EYE?
Despite their therapeutic intent, many routine ophthalmic and medical interventions can inadvertently cause adverse effects on the ocular surface.
Ocular Surgeries
Dry eye disease is a well-documented complication of various ocular surgeries, including corneal refractive procedures, cataract surgery, keratoplasty, corneal cross-linking, eyelid surgery, vitreoretinal interventions, glaucoma surgery, and conjunctival operations.4
Refractive surgery. Procedures like laserassisted in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK) involve corneal ablation or nerve transection, leading to reduced corneal nerve density, which impairs sensation and triggers a neurotrophic form of dry eye.4,7,8 Although nerve regeneration occurs over time, symptoms may persist for months and in some cases, become chronic.7 Studies have shown that East Asian patients tend to experience more severe and prolonged dry eye symptoms after LASIK compared to non-Asian cohorts.8 This disparity may be linked to intrinsic factors such as blinking behaviour, as well as eyelid and orbital anatomy that could predispose the Asian ocular surface to dry eye development.5
Cataract surgery. Patients undergoing lens replacement surgery are typically older and often have pre-existing ocular surface disease.9 Other mechanisms involved with cataract extraction that can exacerbate or trigger the onset of DED include the use of topical anaesthetics and antiseptics, exposure-related keratopathy during surgery, release of inflammatory mediators, conjunctival goblet cell loss, and the use of preserved postoperative eye drops.4
Eyelid surgery. Due to the close interaction between the eyelids, tear film, and ocular surface, surgical procedures involving the eyelids (e.g., blepharoplasty) can potentially lead to dry eye as a postoperative complication.4 Initially, the swelling and inflammation that naturally occur after surgery may interfere with normal eyelid function, resulting in improper lid closure, reduced blink rate, and impaired tear distribution. In addition, adverse changes in eyelid position may lead to incomplete blinking or lagophthalmos, both of which can contribute to dry eye development.10
Management strategies. Preoperative assessment of the ocular surface is vital. A significant proportion of patients undergoing ocular surgery are believed to exhibit signs and/or symptoms of dry eye disease.4,7,9 Identifying and managing existing DED before surgery can improve postoperative outcomes. Patients with pre-existing dry eye should be informed of the risk of symptom exacerbation following surgery. Where possible, ocular surface health should be stabilised with appropriate dry eye treatment prior to any intervention.4 Postoperative care should include continued management, typically involving the use of lubricating ointments, omega 3 fatty acid supplementation, and preservative-free artificial tears containing hyaluronic acid.4 The latter has demonstrated increased protection against desiccation and surfactant insult in an in vitro study,11 as well as improved dry eye symptoms following cataract surgery in a retrospective clinical study.12

Iatrogenic causes of dry eye.
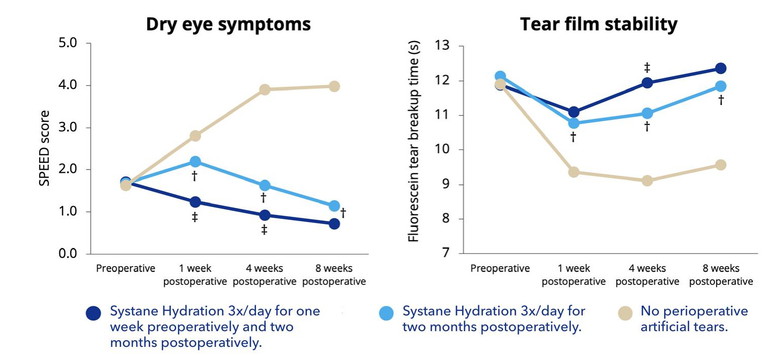
Figure 1. Perioperative use of Systane Hydration reduces signs and symptoms of postoperative dry eye.12
SPEED (Standard Patient Evaluation of Eye Dryness).
Study examined Systane Hydration preserved formulation, which contains the same concentrations of sodium hyaluronate, hydroxypropyl-guar (HP-Guar), propylen glycol (PG), and polyethylene glycol 400 (PEG 400) as Systane Hydration preservative free, as well as the preservative Polyquad.
P <0.05 Systane Hydration 3x/day for one week preoperatively and two months postoperatively and Systane Hydration 3x/day for two months postoperatively vs. no perioperative artificial tears.
P <0.05 Systane Hydration 3x/day for one week preoperatively and two months postoperatively and Systane Hydration 3x/day for two months postoperatively.
Managing Perioperative Dry Eye The effect of Systane Hydration in perioperative management plans for dry eye sufferers was investigated by Favuzza across 17 centres in Italy.12
The data of 419 patients not previously affected by DED, who had undergone cataract surgery in one eye, were reviewed retrospectively. The patients were included in three different groups according to their use of ocular lubricants pre and post surgery: Group A patients instilled the HP-Guar/HA solution i.e. Systane Hydration, three times per day for one week pre operatively and for two months postoperatively; Group B instilled HP-Guar/HA i.e. Systane Hydration for two months postoperatively only; Group C did not instil any artificial tears pre or post surgery. All patients followed the same antibiotic and anti-inflammatory postoperative topical regimen.12
Dry eye was evaluated through tear break-up time and corneal fluorescein staining, and also the Standardised Patient Evaluation of Eye Dryness (SPEED) questionnaire. The SPEED questionnaire is comprised of eight questions to evaluate both the frequency and severity of symptoms. The patient grades the severity of symptoms on a scale of zero to four, with zero being no symptoms and four being intolerable symptoms. The numeric value for each answer is added, with scores ranging from zero to 28. The tests were performed at the preoperative visit and then postoperatively at weeks one, four, and eight.12
Tear break-up time and corneal staining were significantly lower in Groups A and B compared to Group C in the post-operative period (Figure 1). With the use of lubricating eye drops both before and after surgery, Group A showed two times lower SPEED scores, even compared to Group C, at one week post-operatively, and five times lower SPEED scores one month post-operatively. The study concluded that the use of the HPGuar/HA solution was effective at reducing post cataract surgery ocular discomfort and tear instability, particularly if also instilled in the preoperative period.12
Drug-Induced Dry Eye
Topical medications. Many prescribed eye drops, especially preserved glaucoma medications, have been linked to dry eye disease. While effective in microbial control, preservatives like benzalkonium chloride (BAK) have detergent effects on the lipid layer of the tear film, as well as cytotoxic, neurotoxic, and pro-inflammatory effects on the ocular surface.13
Management strategies. Where possible, clinicians should reduce the preservative load by switching to preservative-free formulations and using combination drops to reduce total preservative exposure. For patients with glaucoma, surgical alternatives such as selective laser trabeculoplasty could be considered to help reduce the overall drop burden.14
Systemic medications. Numerous classes of systemic drugs have been linked to dry eye disease, including antihypertensives, diuretics, antidepressants, antihistamines, non-steroidal anti-inflammatory drugs (NSAIDs), isotretinoin, and hormone replacement therapies.15
• Antihypertensives and diuretics. These can reduce aqueous tear production by altering systemic fluid balance.4

• Antidepressants and antihistamines. These medications possess anticholinergic properties that can decrease the production of aqueous and mucous tear components.4
• Isotretinoin. Commonly prescribed for acne management, isotretinoin has been associated with meibomian gland dysfunction, which can contribute to the development of evaporative dry eye.4
Management strategies. As eye care providers, we should be aware of these associations to educate patients that their dry eye could be exacerbated by some of their medications, and help manage their ocular symptoms through supportive therapies. While it may not be feasible to alter systemic medications, patients should be encouraged to collaborate with their doctors to adjust any non-essential medications.
Contact Lens-Induced Dry Eye
Contact lens wear can adversely impact the ocular surface and tear film, contributing to both the onset and worsening of dry eye symptoms.
• Tear film effects. Contact lenses can thin the lipid layer, increase tear evaporation and tear osmolarity, reduce tear meniscus volume and tear turnover rate.4
• Physiological effects. Contact lenses may induce physiological changes on the ocular surface, including alterations in corneal Langerhans cells, reduced conjunctival goblet cell density, lid wiper epitheliopathy, and meibomian gland dropout.4
• Inflammation. Inflammation may be triggered by mechanical friction from the contact lenses or by tear film stagnation, leading to the accumulation of debris, metabolic by-products, and bacterial exotoxins.16
Management strategies. Management includes ensuring proper contact lens fit and selecting appropriate lens materials. Consider switching to daily disposable lenses,4 or to materials with a water surface,** such as Total1 and Precision1, to optimise properties such as lubricity17 and surface softness.18# Additional strategies include using lens materials with internal wetting agents, supplementing with topical lubricants, switching to hydrogen peroxide disinfection, omega 3 and omega 6 fatty acid supplementation, punctal plugs, and azithromycin for lid margin disease.4 Through these strategies, we hope to avoid reducing contact lens wear time or discontinuing lens wear.
Aesthetic Medicine and Cosmetic Products
A growing number of cosmetic procedures involving the periocular region have been linked to adverse effects on the ocular surface.19 These include eyelash curling, dyeing, tinting, and perming, as well as botulinum toxin (Botox), dermal fillers, platelet-rich plasma (PRP) injections, chemical peels, conjunctival tattooing, eyelid piercing and tattooing, microdermabrasion, micro-needling, and various forms of skin resurfacing or tightening.4,20
Injectables commonly used for cosmetic rejuvenation, such as Botox, can also contribute to dry eye development.19 This may occur through its effects on meibomian gland function, reflex tear secretion, blink dynamics, and eyelid closure. In some cases, patients may develop lagophthalmos or reduced blink strength, leading to increased ocular surface exposure and tear film instability.21
“Iatrogenic dry eye refers to ocular surface disease that is unintentionally caused by medical examination or treatments”
In addition to procedures, cosmetic and skincare products such as eyeliner, mascara, powders, lash growth serums, and facial creams can also destabilise the tear film. We often observe particulate matter in the tear film during slit lamp examination, indicating ocular surface contamination. Topical retinoids applied near the eyelid margins, particularly prescription-strength formulations, may further impair meibomian gland function and disrupt lipid secretion, contributing to evaporative dry eye.20
Moreover, many over-the-counter eyelash growth serums contain prostaglandin analogues. Longterm use of these products can be associated with adverse effects such as blepharitis, meibomian gland dysfunction, ocular irritation and redness, iris and periocular skin hyperpigmentation, excessive hair growth, and periorbitopathy.22
Management strategies. Management of ocular surface symptoms associated with cosmetic treatments typically involves patient education and behavioural modification. When patients are receptive, discontinuation or reduced frequency of certain cosmetic products, particularly eyeliner applied to the waterline, can be helpful.23
Additional preventative strategies include:20
• Avoid sharing cosmetic products.
• Clean application tools regularly.
• Adhere to product expiration dates and replace them appropriately (eyeliner and mascara every three months; eye shadow and foundation every six to 12 months.
• Remove make-up thoroughly at the end of each day.
• Apply topical treatments (e.g. retinol creams, lash growth serums) with caution around the eyelids.
• Pay attention to the ingredients used in cosmetics and skincare products.
WHAT IS THE ROLE OF BLINKING AND EYELID MORPHOLOGY IN DRY EYE?
Blinking plays an important role in maintaining ocular surface health.24 Each blink serves to spread and replenish the tear film across the corneal and conjunctival surfaces, ensuring even distribution of the lipid and muco-aqueous layers. This process helps to clear debris, stabilise the tear film, and maintain optimal visual quality.25 Additionally, blinking stimulates the secretion of lipids from the meibomian glands, which are essential for preventing excessive tear evaporation.2 When blinking is incomplete or infrequent, it disrupts these protective mechanisms and may predispose individuals to evaporative dry eye and meibomian gland dysfunction.26,27
Normal blink function can be compromised by a range of factors, including the medical and cosmetic interventions discussed in earlier sections, as well as various lifestyle and environmental influences.4,20,28 These disruptions can reduce blink coverage and increase ocular surface exposure, thereby destabilising the tear film.4,10,21 One of the most prevalent modern risk factors is prolonged digital device use, which has been shown to significantly increase interblink intervals and promote partial blinking.28 Over time, these behaviours can lead to reduced meibomian gland secretion, destabilisation of the tear film, and the development of symptomatic dry eye, even in younger individuals.27
Despite its importance, blink assessment remains underutilised in clinical practice. Evaluation of blink rate, completeness, and quality can offer insight into the underlying causes of DED.24,26 Methods of assessment include direct observation at the slit lamp, high-speed video analysis, or the use of dedicated diagnostic devices such as the Oculus Keratograph or LipiView. Identifying patients with incomplete blinking allows for early intervention through strategies such as patient education, blink awareness techniques, and training exercises to help restore effective blinking patterns.25,27,28
Eyelid anatomy also plays a significant role in dry eye pathophysiology, particularly in East Asian populations.2,3,5,6,29 Although the underlying reasons for ethnic differences in the natural history of dry eye disease are not yet fully understood, it is thought that anatomical traits, such as increased eyelid tension, may contribute to a higher prevalence of incomplete blinking, even in younger individuals.6 Notably, studies have shown that Asian participants exhibit a greater incidence of lid wiper epitheliopathy and meibomian gland dropout compared to their White counterparts, while tear meniscus height tends to be comparable across ethnicities.3,5,6,29 These findings suggest a tendency towards evaporative mechanisms in this group, rather than aqueous-deficient forms of dry eye.5
Although further research is warranted, current evidence supports a proactive approach to managing dry eye in East Asian patients, a population identified as being at increased risk for the disease.3 Diagnostic imaging techniques, such as meibography and lipid layer interferometry, can help detect subtle meibomian gland changes before clinical symptoms arise. Mainstay home-based therapies include warm compresses, consistent eyelid hygiene, and manual meibum expression.30 Additional interventions may involve the use of lipidbased artificial tears, blink training to stimulate meibomian gland secretion, and in-office procedures such as low-level light therapy31 or intense pulsed light.32
“Diagnostic imaging techniques… can help detect subtle meibomian gland changes before clinical symptoms arise”
WHY DO ARTIFICIAL TEARS FORMULATIONS MATTER?
Patients can be confused by the array of options for lubricating eye drops and may not understand the differences between them. Alcon has introduced a range of multidose preservative free products in the Systane range, in addition to the existing single use vials. The Systane family of lubricating eye drops has a unique formulation combining HP-Guar and borate, which forms a viscoelastic gel promoting the retention of the demulcents.33 Systane Hydration, previously discussed in the study investigating perioperative management of dry eye, combines hyaluronic acid* with HP-Guar and borate. In the bottle or vial, HP-Guar and borate are loosely crosslinked due to interaction with sorbitol. On instillation into the eye, the sorbitol is diluted and together with the change in pH, the HP-Guar and borate crosslink to form a viscoelastic meshwork. This meshwork preferentially binds to damaged areas of the corneal epithelium and acts like a bandage34 to enhance moisture retention and reduce tear evaporation.35
The HP-Guar/HA combination of Systane Hydration has been shown to support healing of the damaged ocular surface, assisting cell viability and regeneration.11,33 This combination also resulted in greater and faster wound healing (measured in reepithelialisation) compared to HA alone in a laboratory study.36π In a laboratory study, Systane Hydration provided significantly longer tear film break-up time vs an HA only formulation.37
The Role of Systane Complete
With many patients suffering from iatrogenic dry eye experiencing EDDE, the need to support all layers of the tear film, including the lipid layer, should also be considered.30 In a normal tear film, the lipid layer consists of oils, but also a component called phospholipids. These phospholipids work by stabilising the interface between the lipid layer and the underlying aqueous layer.38 The formulation of Systane Complete looks to support all layers of the tear film by combining HP-Guar and borate with nano-sized lipid droplets comprised of mineral oil surrounded by phospholipid. These droplets facilitate integration into the tear film39 and optimise the coverage area of phospholipid delivered to the tear film.30 Using Systane Complete four times per day has been shown to increase lipid layer thickness compared to a drop, which did not contain lipid, and this effect was seen to be ongoing.40 This study also noted that after using lubricating drops four times per day, patients who experience improvement in their symptoms are likely to do so at the one month follow-up. If there is no improvement in symptoms after one month, alternative management should be considered.
Secondly, the study recommended encouraging the ongoing use of lubricants. This is because improvement in clinical signs, such as ocular surface staining and lid wiper epitheliopathy, can take longer to improve, even if there is a reduction in dry eye symptoms after one month.40
HOW CAN YOU MAKE A DIFFERENCE TO OUTCOMES?
By carefully considering the risk of iatrogenic dry eye, along with diagnosing and appropriately managing any existing dry eye disease, we can significantly enhance patient surgical outcomes, improve tolerance to medical treatments that may cause dry eye disease, and ultimately improve patient quality of life.

Dr Ally Xue BOptom (Hons) PhD is a research fellow at Auckland University Faculty of Medical and Health Sciences, Ophthalmology, New Zealand. Dr Xue received an honorarium for her time contributing to the article.

Helen Gleave BScOpt (Hons) MCOptom is the Senior Professional Education and Development Manager at Alcon. She is responsible for training and education programmes in contact lenses, contact lens care, and dry eye, including Alcon Dry Eye Academy and Dry Eye Academy Online. She has delivered education to a broad range of audiences, and spoken at numerous optometry conferences, educational events, and webinars across Australia and New Zealand.
This article was sponsored by Alcon. ANZ-SYY-PRA-2500004
To earn your CPD hours from this article, visit mieducation.com/do-no-ocular-surface-harm-to-uncover-iatrogenic-dry-eye.
* Systane Hydration lubricant eye drops contain sodium hyaluronate, the salt form of hyaluronic acid.
** Water content approaches >80% at the surface.
#Based on surface modulus measured with atomic force microscope nanoindentation studies with delefilcon A material (TOTAL1 sphere lenses).
π Based on an animal model.
References available at mieducation.com.