mieducation
When Intervention is Less Intrusive:
The Changing Face of Glaucoma Management
Glaucoma is the leading cause of permanent blindness worldwide, with prevalence projected to increase over time. Treatment of open angle glaucoma (OAG) focusses on reducing intraocular pressure (IOP), which has been established as the only proven modifiable risk factor in disease progression.1-6While topical medications were once the first-line treatment for glaucoma management, Dr Phoebe Moore proposes that the paradigm is shifting towards early implementation of interventional and surgical treatment options.
WRITER Dr Phoebe Moore
LEARNING OBJECTIVES
On completion of this CPD activity, participants should:
1. Understand options for glaucoma management by general ophthalmologists,
2. Recognise the risks and benefits of interventional treatment,
3. Be aware of which patients are suitable for minimally invasive glaucoma surgery (MIGS), and
3. Be cognisant of risks associated with MIGS compared to long-term topical therapy.
The traditional paradigm for achieving IOP reduction for OAG patients has relied on topical medication therapy as the firstline treatment, with escalation of topical drop therapy as required, reserving surgical management for severe or uncontrolled cases.1
The 1990s saw an explosion of topical medication options for the management of glaucoma, revolutionising the ability to manage this progressive, blinding condition with a low-risk, intervention-free medication that was more effective than previous options.
The historical preference for topical therapy and reservation towards surgical management was understandable in bygone eras because of the high relative risk of interventional procedures and filtration surgery (with apologies to our more experienced colleagues for describing the 1990s as a bygone era).
DROPS: AN UNHAPPY MARRIAGE
Clinicians are all too familiar with patients on ‘maximal tolerated medical therapy’, consisting of multiple drops and carefully communicated regimens that patients are required to strictly adhere to, lest they experience irreversible vision loss.
The clinician and patient form an almostmatrimonial agreement whereby drops shall be used ‘for better or for worse, in sickness and in health, with red eyes or white eyes, until death do us part’.
However, faithfulness to the eye drop marriage vow is often punished, not rewarded. For many of our patients, the experience of a marriage to drops is more likely worse than better, more likely sickness than health, more likely red eyes than white eyes.
While an essential tool in the clinician’s arsenal for glaucoma management, and notwithstanding the place they have held to avert preventable blindness, topical glaucoma therapy is accompanied by a host of negative and undesirable consequences.2
In a bygone era, when choosing the lesser of all evils, topical medications were accepted as first-line therapy due to the risks of alternative therapies. However, in a changing era of glaucoma management options, there is also a changing face of first-line glaucoma treatment, and it no longer consists of periorbitopathy, hyperaemia, and dry eye.
Drop-related challenges familiar to both patients and clinicians are wide reaching and develop due to a plethora of patientdependent and patient-independent factors.7,8
Compliance issues and drop nonadherence are widely reported among glaucoma patients, which confers an increased risk of disease progression.2 Complex regimens for patients, requiring multiple drops per day can be challenging, particularly for older patients or those with cognitive decline. The challenges are compounded by difficulties with instillation and the ongoing saga of pharmaceutical product discontinuation, necessitating modifications in already complex regimens.9
Topical therapy is associated with greater circadian fluctuations in IOP compared to interventional treatment, even when used with perfect compliance, which in turn is associated with greater progression.10,11
Unwanted side effects are common, experienced by more than 50% of patients receiving topical glaucoma therapy, and often render treatment untenable for patients. Ocular surface toxicity is a common consequence of topical medications, experienced by up to 70% of patients.2 Ocular surface toxicity is not only distressing for patients but is also problematic should the patient require escalation to filtration surgery.12-14
While rare, topical therapy is not without more significant risk. These risks may be ocular, including intraocular inflammation, cystoid macular oedema, and periorbital fat atrophy.2
And the risks of topical therapy are not always confined to the eye. In a challenge to the commonly held notion that ‘surgery is dangerous, drops are safe’, topical glaucoma therapy is not without systemic respiratory and cardiovascular risk, morbidity, and albeit rare, mortality.15
“Drop-related challenges familiar to both patients and clinicians are wide-reaching and develop due to a plethora of patient-dependent and patient-independent factors”
Finally, the cumulative cost of medications is not an insignificant burden for patients requiring lifelong therapy, an issue that is heightened in the current economic climate and is an increasing factor for many patients with compliance issues.16
Considering all the above, it is little wonder that a patient’s quality of life is negatively impacted both by a glaucoma diagnosis, and even further by topical glaucoma treatment.17 Topical glaucoma therapy has been consistently shown to negatively impact quality of life, due to a combination of factors including side effects, difficulty with drop instillation, and treatment burden, which can further contribute to drop noncompliance.7,9,17
Conversely, the ability to discontinue drops or decrease drop dependence is associated with an increase in perceived quality of life.18
So, in 2025, as clinicians, we must ask the question: is it still acceptable standard practice to urge glaucoma patients to persist in unhappy matrimony to their drops? Or should the red eye serve as a red flag that this may be a toxic relationship? Toxic not only to the ocular surface, but to the patient’s overall wellbeing and quality of life.
THE CHANGING FACE OF TREATMENT OPTIONS
The historical paradigm of glaucoma management has overwhelmingly relied on topical therapy, with surgery reserved for recalcitrant cases. This was not a denial of the limitations and adverse effects common to topical treatment, but rather a recognition of the high risk of traditional filtration surgery relative to topical therapy.
However, the 21st century has seen an explosion of treatment options for glaucoma, and with this, a shift in the risk profile of interventional glaucoma treatment relative to topical treatment. The traditional paradigm of glaucoma treatment is no longer fit-for-purpose.
The LiGHT trial19 marked a shift in firstline treatment of glaucoma. There is a substantial evidence base supporting the shift away from drops and embracing selective laser trabeculoplasty (SLT) as an early intervention for glaucoma management.
Beyond SLT, interventional glaucoma management with minimally invasive glaucoma surgery (MIGS) has emerged as an umbrella term describing a group of procedures that lower IOP and minimise drop requirement, while minimising tissue or angle destruction and the procedural risk associated with bleb-forming or suprachoroidal procedures.20-22 This lower risk allows for earlier adoption of interventional management, effective and sustained reductions in IOP, and decreased requirement for topical therapy, while avoiding the risks associated with traditional filtration surgery.
MINIMALLY INVASIVE GLAUCOMA SURGERY
While cataract surgery alone will often achieve a degree of IOP reduction for glaucoma patients, combining planned cataract surgery with a MIGS device achieves greater reductions in IOP. Additionally, there is a greater likelihood of the patient achieving post-operative drop-independence compared to cataract surgery alone.23-25 Fan Gaskin et al.25 reported that 57% of eyes with mild to moderate glaucoma undergoing cataract surgery with MIGS achieved drop independence versus 36% for patients undergoing cataract surgery alone.
Readers will be familiar with the current array of MIGS devices, the most common of which are Glaukos’ iStent trabecular microbypass system in its various generations, and Alcon’s Hydrus microstent. Initially developed to be used in combination with cataract surgery, these MIGS devices lower IOP by enhancing conventional aqueous outflow. Both devices have demonstrated effective reductions in IOP and decreased medication requirement, with similar safety outcomes to cataract surgery alone.26,27
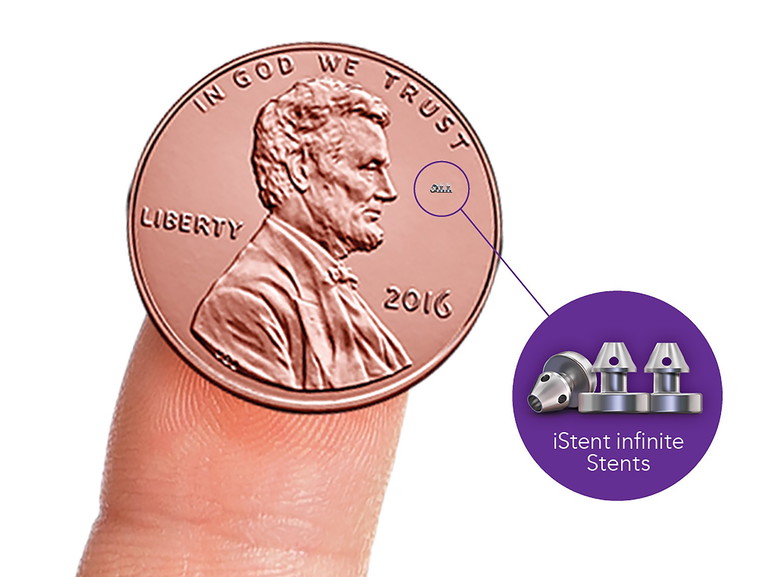
First released in 2004, there have now been four generations of the iStent MIGS device, from the original iStent, to the iStent inject released in 2010, the iStent inject W released in 2019, all of which consisted of two implantable bypass devices. Most recently the iStent infinite was released. This latest permutation has three implantable devices contained within a single preloaded injector. The implants occupy just 3% of the trabecular meshwork but optimise the aqueous outflow across 240˚.1,27,28
Since its release in 2004 and across its generations, the iStent has established a record of effective and sustained reduction in IOP for patients with ocular hypertension, mild to moderate primary glaucoma, and secondary glaucoma, with high rates of topical medication discontinuation and low rates of secondary filtration surgery.1,29-31
In the longest published follow-up to date of 10 years, Neuhann et al.1 reported IOP reduction of 12.9–19% for patients undergoing cataract surgery combined with the firstgeneration iStent. Of these eyes, 77.8% had IOP ≤18 mmHg, versus 50.8% preoperatively. Additionally, 47.6% achieved IOP ≤15 mmHg versus 25.4% preoperatively, and 33.3% of eyes achieved post-operative drop independence, versus 3.2% pre-operatively. Nearly all eyes maintained the reduced medication over the 10 years. No filtration surgeries were required over the 10-year follow-up.
While traditionally used for mild to moderate glaucoma, there is a body of evidence supporting the role of MIGS in moderate to severe glaucoma, with a positive risk-benefit profile when compared to filtration surgery.32

STANDALONE VS COMBINATION WITH CATARACT SURGERY
While traditionally reported in combination with cataract surgery, attention has more recently been given to MIGS as a successful standalone procedure, either in phakic or pseudophakic patients.33,34
Moraes et al.35 report a 16.5% reduction in IOP and 72.3% reduction in medications with the iStent inject device over a five-year follow-up for patients with mild to moderate open angle glaucoma. Of these cases, 79% of eyes received the iStent inject in combination with cataract surgery, while 21% received the iStent as a standalone procedure in already pseudophakic eyes.
The procedure had a favourable safety profile and low complication rate. Intraoperative bleeding was reported in three cases. There was one case of peripheral anterior synechiae (PAS) into the implant ostium, treated with peripheral iridotomy under gonioscopic visualisation.
Sixty-six per cent of eyes achieved drop independence, compared to just 1.8% preoperatively, with the mean number of IOPlowering medications reducing from 2.24 at baseline to 0.62 at last follow-up. Four eyes required a secondary procedure – two required trabeculectomy and two received SLT.
Sarkisian et al.36 evaluated the iStent infinite device as a standalone procedure in 72 eyes with open angle glaucoma not adequately controlled by prior surgical or medical therapies over a 12-month follow-up. Six of the eyes were phakic. Of all eyes, 76.1% achieved a ≥20% reduction in mean diurnal IOP (MDIOP) with 53% achieving ≥30% MDIOP reduction and 21.2% achieving a ≥40% reduction.
“As evidence-based, forward thinking, patient-focussed practitioners, are we willing to have our paradigm challenged?”
No serious device-related adverse events were recorded. There were three cases of significant hyphaema, two events of stent migration seen in one eye, and two cases of stent obstruction. With the exception of the stent obstruction, which was not treated, all device-related adverse events resolved completely.
Six eyes receiving standalone iStent were phakic. There were no cases of progressive cataract, and no cataract surgery was required within the 12-month follow-up.
ISTENT VS HYDRUS
In the INTEGRITY study, Ahmed et al.28 compared the iStent infinite with the Hydrus microstent in adults with open angle glaucoma with six months followup published to date. MIGS devices were implanted as standalone procedures in both phakic and pseudophakic eyes. Ninety-one eyes received the iStent infinite, 89 eyes received the Hydrus implant.
At six months post-implantation, both the iStent infinite and Hydrus Microstent effectively reduced IOP. However, the iStent demonstrated a higher rate of significant IOP reduction (≥20% reduction) without medications, and was associated with fewer adverse events and surgical complications.
In the iStent group, one eye had a fourth stent implanted as a result of one of the stents being improperly placed below the scleral spur. In one phakic eye receiving the iStent infinite, the device damaged the anterior capsule, requiring cataract surgery the following day. This eye developed PAS.
In the Hydrus group, implantation was aborted in one eye due to three unsuccessful attempts, positioning into the supraciliary space with iris prolapse requiring an intraoperative iridotomy. This eye developed PAS and dyscoria. One of the pseudophakic Hydrus eyes also experienced vitreous prolapse due to significant capsular tear, and required vitrectomy during the surgical procedure. Seven additional Hydrus eyes were reported to have adverse events associated with improper placement. One eye was complicated by iridodialysis and inadvertent iridectomy with subsequent PAS. Other reported complications related to the stent being less than ideally positioned.
In the iStent group, PAS was reported in 4.4%, iris atrophy in 3.3%, and improper anatomical placement in 1.1%, with a reported surgical complication rate of 3.3%. The Hydrus group had higher rates with PAS in 10.1%, improper anatomical placement in 7.9%, and significant hyphaema in 4.5%, with a reported surgical complication rate of 16.9%. There were no severe or vision-threatening complications in either group.
THE CHANGING PARADIGM: EARLY INTERVENTION
As clinicians, we operate under the creed of primum non nocere – first, do no harm. This creed is outworked in the management of glaucoma through an approach of choosing the lesser of all evils. We are well aware that all treatment modalities carry risk and compromise, and it is our job to assist our patients in the prevention of vision loss while minimising this risk and compromise.
“In 2025, we need to consider the evidence and ask the question: when it comes to glaucoma treatment, where does the greatest harm lie? Is intervention less intrusive?”
In a bygone era, when choosing the lesser of all evils, topical medications were accepted as first-line therapy due to the risks of alternative therapies. For generations, this balance of risk has swung in favour of topical glaucoma therapy, leading to the paradigm most of us are familiar with in the management of glaucoma: drops, drops, drops, drops, and then finally, surgery.
But in 2025, in an age of changing treatment options, the traditional paradigm of glaucoma treatment is no longer fit-for-purpose. As evidence-based, forward thinking, patientfocussed practitioners, are we willing to have our paradigm challenged?
As clinicians, we are called to be holistic in the care of our patients. To consider their preference, their quality of life. To do no harm.
In 2025, we need to consider the evidence and ask the question: when it comes to glaucoma treatment, where does the greatest harm lie? Is intervention less intrusive?
This is a question that has been asked widely in clinical circles across Australia, and the response of our colleagues is a resounding push away from topical treatment towards early intervention in the form of SLT or MIGS procedures for management of glaucoma.37
We recognise that topical glaucoma therapy has held, and continues to hold, a vital place in the management of glaucoma. We also recognise that MIGS procedures are not without risk. However, in advocating for our patients, we need to weigh the one-time risk of an interventional procedure against the cumulative, life-long risk of topical therapy.
Our end goal in glaucoma treatment is to avoid preventable blindness and thereby preserve quality of life. Are we willing to accept that our traditional treatment modalities may be hindering the very quality of life we are endeavouring to preserve? When it comes to holistic patient care, preservation of vision and quality of life, is intervention less intrusive?
“Our end goal in glaucoma treatment is to avoid preventable blindness and thereby preserve quality of life”
To earn your CPD hours from this article, visit mieducation.com/when-intervention-is-less-intrusivethe-changing-face-of-glaucoma-management.
This article was sponsored by Glaukos.
References
1. Neuhann TH, Neuhann RT, Hornbeak DM. Ten-year effectiveness and safety of trabecular micro-bypass stent implantation with cataract surgery in patients with glaucoma or ocular hypertension. Ophthalmol Ther. 2024 Aug;13(8):2243-2254. doi: 10.1007/s40123-024-00984-1.
2. Radcliffe NM, Shah M, Samuelson TW. Challenging the ‘topical medications-first’ approach to glaucoma: A treatment paradigm in evolution. Ophthalmol Ther 2023;12(6):2823-2839. doi: 10.1007/s40123-023-00831-9.
3. Flaxman SR, Bourne RRA, Taylor HR, et al. Vision Loss Expert Group of the Global Burden of Disease Study. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017 Dec;5(12):e1221-e1234. doi: 10.1016/S2214-109X(17)30393-5.
4. Tham YC, Li X, Cheng CY, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014 Nov;121(11):2081-90. doi: 10.1016/j.ophtha.2014.05.013.
5. Heijl A, Leske MC, Hussein M, et al. Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002 Oct;120(10):1268-79. doi: 10.1001/archopht.120.10.1268.
6. Gordon MO, Beiser JA, Kass MA, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002 Jun;120(6):714-20; discussion 829-30. doi: 10.1001/archopht.120.6.714.
7. Skalicky SE, Goldberg I, McCluskey P. Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol. 2012 Jan;153(1):1-9.e2. doi: 10.1016/j.ajo.2011.05.033.
8. Bedrood S, Berdahl J, Sheybani A, Singh IP. Alternatives to topical glaucoma medication for glaucoma management. Clin Ophthalmol. 2023 Dec 14;17:3899-3913. doi: 10.2147/OPTH.S439457.
9. Nordstrom BL, Friedman DS, Walker AM, et al. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol. 2005 Oct;140(4):598-606. doi: 10.1016/j.ajo.2005.04.051.
10. Stewart WC, Konstas AG, Nelson LA, Kruft B. Meta-analysis of 24-hour intraocular pressure studies evaluating the efficacy of glaucoma medicines. Ophthalmology. 2008 Jul;115(7):1117-1122.e1. doi: 10.1016/j.ophtha.2007.10.004.
11. Muniesa MJ, Ezpeleta J, Benítez I. Fluctuations of the intraocular pressure in medically versus surgically treated glaucoma patients by a contact lens sensor. Am J Ophthalmol. 2019 Jul;203:1-11. doi: 10.1016/j.ajo.2019.02.003.
12. Camras CB. Comparison of latanoprost and timolol in patients with ocular hypertension and glaucoma: a six-month masked, multicenter trial in the United States. The United States Latanoprost Study Group. Ophthalmology. 1996 Jan;103(1):138-47. doi: 10.1016/s0161-6420(96)30749-5.
13. Kolko M, Gazzard G, Baudouin C, Cvenkel B, et al. Impact of glaucoma medications on the ocular surface and how ocular surface disease can influence glaucoma treatment. Ocul Surf. 2023 Jul;29:456-468. doi: 10.1016/j.jtos.2023.05.012.
14. Broadway DC, Grierson I, O'Brien C, Hitchings RA. Adverse effects of topical antiglaucoma medication. II. The outcome of filtration surgery. Arch Ophthalmol. 1994 Nov;112(11):1446-54. doi: 10.1001/archopht.1994.01090230060021.
15. Nelson WL, Fraunfelder FT, Kuritsky JN, et al. Adverse respiratory and cardiovascular events attributed to timolol ophthalmic solution, 1978-1985. Am J Ophthalmol. 1986 Nov 15;102(5):606-11. doi: 10.1016/0002-9394(86)90532-5.
16. Patel AR, Schwartz GF, Smith OU. Economic and clinical burden associated with intensification of glaucoma topical therapy: A US claims-based analysis. J Glaucoma. 2021 Mar 1;30(3):242-250. doi: 10.1097/IJG.0000000000001730.
17. Nordmann JP, Auzanneau N, Ricard S, Berdeaux G. Vision related quality of life and topical glaucoma treatment side effects. Health Qual Life Outcomes. 2003 Dec 10;1:75. doi: 10.1186/1477-7525-1-75.
18. Samuelson TW, Singh IP, Katz LJ, et al. Quality of life in primary open-angle glaucoma and cataract: An analysis of VFQ-25 and OSDI from the iStent inject® pivotal trial. Am J Ophthalmol. 2021 Sep;229:220-229. doi: 10.1016/j.ajo.2021.03.007.
19. Gazzard G, Konstantakopoulou E, Bunce C, et al. LiGHT Trial Study Group. Laser in Glaucoma and Ocular Hypertension (LiGHT) trial. A multicentre, randomised controlled trial: design and methodology. Br J Ophthalmol. 2018 May;102(5):593-598. doi: 10.1136/bjophthalmol-2017-310877.
20. Castro C, Marta A, Marques JH, Barbosa I, et al. Ocular surface changes in primary open angle glaucoma patients treated with topical antihypertensive drugs. J Glaucoma. 2023 Oct 1;32(10):e113-e120. doi: 10.1097/IJG.0000000000002272.
21. Boland MV, Corcoran KJ, Lee AY. Changes in performance of glaucoma surgeries 1994 through 2017 based on claims and payment data for United States Medicare beneficiaries. Ophthalmol Glaucoma. 2021 Sep-Oct;4(5):463-471. doi: 10.1016/j.ogla.2021.01.004.
22. Saheb H, Ahmed II. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012 Mar;23(2):96-104. doi: 10.1097/ICU.0b013e32834ff1e7.
23. Zhang ML, Hirunyachote P, Jampel H. Combined surgery versus cataract surgery alone for eyes with cataract and glaucoma. Cochrane Database Syst Rev. 2015 Jul 14;2015(7):CD008671. doi: 10.1002/14651858.CD008671.pub3.
24. Laroche D, Madu CT. Preventing blindness with early cataract surgery and micro-invasive glaucoma surgery in patients over 50: Guidance for patients, physicians and world governments in dealing with glaucoma. Clin Ophthalmol. 2023 Oct 4;17:2929-2938. doi: 10.2147/OPTH.S422415.
25. Fan Gaskin JC, Bigirimana D, Ang GS, et al. Glaucoma Investigation and Research Unit, Royal Victorian Eye and Ear Hospital. prospective, randomized controlled trial of cataract surgery vs combined cataract surgery with insertion of iStent inject. Ophthalmol Glaucoma. 2024 Jul-Aug;7(4):326-334. doi: 10.1016/j.ogla.2024.02.004.
26. Samuelson TW, Sarkisian SR Jr, Katz LJ, et al. iStent inject Study Group. Prospective, randomized, controlled pivotal trial of an ab interno implanted trabecular micro-bypass in primary open-angle glaucoma and cataract: Two-year results. Ophthalmology. 2019 Jun;126(6):811-821. doi: 10.1016/j.ophtha.2019.03.006.
27. Samuelson TW, Chang DF, Singh K, et al. HORIZON Investigators. A schlemm canal microstent for intraocular pressure reduction in primary open-angle glaucoma and cataract: The HORIZON study. Ophthalmology. 2019 Jan;126(1):29-37. doi: 10.1016/j.ophtha.2018.05.012.
28. Ahmed IIK, Berdahl JP, Navratil T, et al. Six-month outcomes from a prospective, randomized study of iStent infinite versus hydrus in open-angle glaucoma: The INTEGRITY study. Ophthalmol Ther. 2025 May;14(5):1005-1024. doi: 10.1007/s40123-025-01126-x. .
29. Salimi A, Watt H, Harasymowycz P. Long-term outcomes of two first-generation trabecular micro-bypass stents (iStent) with phacoemulsification in primary open-angle glaucoma: eight-year results. Eye Vis (Lond). 2021 Nov 16;8(1):43. doi: 10.1186/s40662-021-00263-1.
30. Lindstrom R, Sarkisian SR, Voskanyan L, et al. Four-year outcomes of two second-generation trabecular micro-bypass stents in patients with open-angle glaucoma on one medication. Clin Ophthalmol. 2020 Jan 13;14:71-80. doi: 10.2147/OPTH.S235293.
31. Ferguson TJ, Mechels KB, Berdahl JP, et al. iStent trabecular microbypass stent implantation with phacoemulsification in patients with open-angle glaucoma: 6-year outcomes. Clin Ophthalmol. 2020 Jul 2;14:1859-1866. doi: 10.2147/OPTH.S247910.
32. Paletta Guedes RA, Chaoubah A, et al. Standalone implantation of 2-3 trabecular micro-bypass stents (iStent inject ± iStent) as an alternative to trabeculectomy for moderate-to-severe glaucoma. Ophthalmol Ther. 2022 Feb;11(1):271-292. doi: 10.1007/s40123-021-00424-4.
33. Healey PR, Clement CI, Aghajanian L, et al. Standalone istent trabecular micro-bypass glaucoma surgery: A systematic review and meta-analysis. J Glaucoma. 2021 Jul 1;30(7):606-620. doi: 10.1097/IJG.0000000000001805.
34. Ferguson TJ, Ibach M, Berdahl JP, et al. Trabecular microbypass stent implantation in pseudophakic eyes with open-angle glaucoma: Long-term results. J Cataract Refract Surg. 2019 Apr;45(4):414-420. doi: 10.1016/j.jcrs.2018.11.005.
35. Guedes RAP, Gravina DM, Chaoubah A, et al. Five-year outcomes of iStent inject implantation with or without phacoemulsification in eyes with open-angle glaucoma. Ophthalmol Ther. 2025 Jun;14(6):1219-1235. doi: 10.1007/s40123-025-01134-x.
36. Sarkisian SR Jr, Grover DS, Navratil T, et al. iStent infinite Study Group. Effectiveness and safety of iStent infinite trabecular micro-bypass for uncontrolled glaucoma. J Glaucoma. 2023 Jan 1;32(1):9-18. doi: 10.1097/IJG.0000000000002141.
37. Newman AR, Andrew NH. Changes in Australian practice patterns for glaucoma management. Clin Exp Ophthalmol. 2019 Jul;47(5):571-580. doi: 10.1111/ceo.13456.

Dr Phoebe Moore BMed (Dist) MMed FRANZCO is a general ophthalmologist with subspecialty expertise in retinal diseases, uveitis, and cataract. She is based in Tamworth, New South Wales, and practises in regional Australia.