mieducation
Progressing Myopes: Why Your Management Matters
Back in 2016, Professor Brien Holden described myopia as a crucial global health issue and forecast that 50% of the world’s population will be myopic by 2050 and 10% will have high myopia.1
Australia is in a strong position to tackle the challenges of myopia management, thanks to its highly skilled eye care professionals, a comprehensive range of myopia management technologies, and a well-supported (albeit not perfect) Medicare-funded eye care system. But we need to act now.
WRITER Soojin Nam
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Understand why proactive myopia management is essential,
2. Realised the many options for managing myopia and the efficacy,
3. Be aware of risk and compliance issues, and
4. Realise considerations when ceasing treatment.
It is well established that high myopia increases the risk of serious eye conditions, such as retinal detachment, myopic macular degeneration, cataracts, and glaucoma.2 It is predicted that without changing current interventions, 0.57% of the world’s population will be affected by myopic maculopathy by 2050.3 For the progressing myope, every 1D increase in myopia will increase their risk of myopic maculopathy by 67%.4 This means that it really is never too late to start managing myopia. A decrease of even just one dioptre is equivalent to a reduction of myopic maculopathy risk by 40%.4
A simple target for myopia management is to control it under -6.00D. This is because for myopes greater than -6.00D, the risk of visual impairment by the age of 75 increases to 39% (representing a five-fold risk).
Additionally, the aim of myopia management is to keep the axial length at adulthood under 26 mm. In an emmetropic eye, axial length grows by 0.1 mm per year to 0.2 mm until age 10 and then 0.1 mm until it stabilises. The myopic eye in single vision lenses, by comparison, progresses faster at 0.3 mm per year until age 10 and then 0.2 mm.
The risk of visual impairment increases as axial length elongates: for axial length greater then 26 mm there is a 25% increased risk compared to an increased risk of more than 90% for axial length greater than 30+.5
RECENT INTERVENTIONS TO MANAGE MYOPIA
Interventions for slowing myopia progression available in Australia include topical lowdose atropine eye drops (compounded concentrations and Eikance 0.01% (Aspen Pharmacare)), peripheral plus spectacle lenses (defocus incorporated multiple segments (DIMS, HOYA)), highly aspherial lenslets target (HALT, EssilorLuxottica) lenses, repeated low-level red-light (RLRL) therapy, multifocal and dual-focus soft contact lenses, and orthokeratology (OK).
New entrants to the myopia spectacle lens portfolio include MyoMe (CR Labs) which uses Myo-Freeform technology; MyoStock (CR Labs), which uses hexagon-implicated defocus segments (HIDS) technology, and MyCon (Rodenstock), which concentrates on the horizontal retina providing peripheral blur nasally and temporally to the optical centre of the lens. On the horizon for Australian patients are diffusion optics technology (DOT) spectacle lenses, and Abiliti 1-Day contact lenses (currently available in New Zealand). When searching for the holy grail of the most effective modality, keep in mind, that the most significant consideration is compliance – is the child happy to wear this consistently?
Note that there are limited direct comparisons of myopia control treatments, and a recent comprehensive review8 concluded that no single method shows clear superiority, with OK, soft multifocal contact lenses (SMCL), peripheral plus defocus spectacles, and lowdose atropine monotherapy demonstrating similar effectiveness. For ease of comparison, Table 1 only details the efficacy from axial length reduction (but not the refractive error) compared to the study control.
Current optical myopia interventions (including the recent spectacle peripheral plus lenses) are all based on the premise they induce myopic peripheral blur on the peripheral retina (assuming 30º from the fovea).6 While the data is very promising, we still don’t know the optimal level of blur required to influence eye growth or how to measure the ideal retinal eccentricity (somewhere between 20–40º) that might influence myopia regression.
The appeal of 0.01% atropine in managing myopia has recently declined due to conflicting results concerning its impact on axial elongation. The variability in patient compliance with 0.01% atropine could also explain these discrepancies. A recent meta-analysis review has identified 0.05% atropine as the most effective concentration for managing progressing myopia. Despite its effectiveness, the higher concentration of atropine may lead to side effects, such as increased blur at near and heightened light sensitivity, which could make it a less attractive option for some patients or will require supportive lenses such as sunglasses or reading addition.9 Some myopic children are considered to be ‘poor responders’ to lowdose atropine, and around 45% of children will continue to progress by more than 0.5D over six months with 0.05% atropine.10
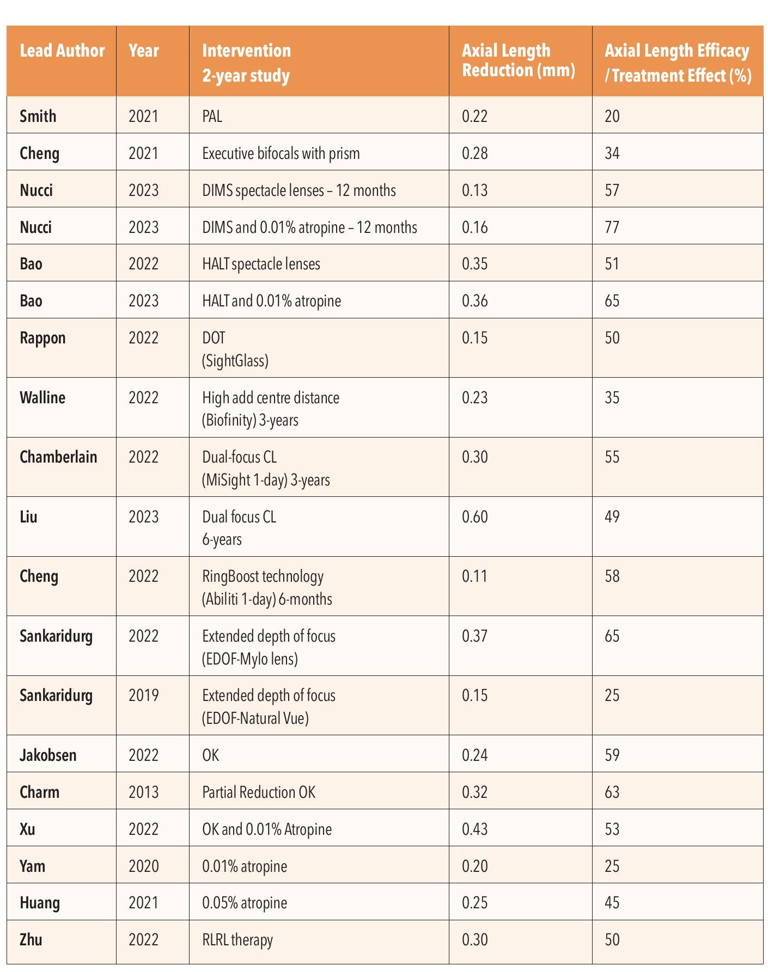
Table 1. Recent updates on interventions to manage the progressing myope. Studies can be sourced via Lawrenson, J.G., et al.6 and Zhang, X.J. et al.7
Abbreviations: PAL (progressive addition lens); DIMS (defocus incorporated multiple segments); HALT (highly aspherical lenslet target); DOT (diffusion optics technology); CL (contact lens); OK (orthokeratology); RLRL (repeated low level red light).
Orthokeratology was recognised as the first optical method for myopia control with the publication of a randomised controlled trial in 2012,11 yet it still accounts for only 1.2% of all contact lens fittings across 45 countries.12 Research shows that combining 0.01% atropine with OK13 or DIMS lenses14 is more effective than monotherapy. However, the effectiveness of 0.01% atropine combined with SMCL with a +2.50D add15 did not result in better efficacy. A recent 2024 study further supported the effectiveness of combination therapies,16 finding that OK with atropine and DIMS with atropine significantly reduced axial elongation more than each monotherapy. This synergistic effect was especially pronounced in older children (aged 10–14 years) compared to younger ones (aged six to 10 years). This suggests that combination therapies may be even more beneficial as children grow older, possibly due to different responses to atropine or changes in eye growth rates with age.
REGULATORY APPROVALS
Eikance 0.01% is the only low-dose atropine concentration with Australian Therapeutic Goods Administration (TGA) approval since 2021. However, some clinicians are prescribing higher concentrations of atropine, such as 0.025% or 0.05%, for high-risk myopic patients. The field of dual therapy is still developing, and emerging research continues to refine our understanding of the most effective treatment protocols for the different risk profiles of progressing myopes.
It is worth mentioning that the absence of approval of myopia control products by the United States Food and Drug Administration is a complication in clinical practice. Notable mentions are MiSight contact lenses, which were approved for myopia correction and myopia control in February 2019 (with a strict criterion for children between the ages of eight to 12 years old with a refraction of -0.75 to -4.00 with -0.75D or less of astigmatism), closely followed in May 2019 by the only CE-mark approved OK lens for myopia control, Menicon Bloom. Most of the treatments listed in the Cochrane Review:17 OK (which has extensive research on efficacy and safety), dual-focus soft contact lenses, low-dose atropine, and peripheral defocus spectacle lenses, are being prescribed for myopia control off-label. This lack of regulatory endorsement can affect patient communication, efficacy of compounded atropine formulations, and prescribing practices among eye care professionals.
Compounded low-dose atropine is diluted from available 1% atropine or prepared from raw materials. Dilution alters the concentration of preservatives and other constituents, which can influence the final product’s stability and consistency. As part of management, we need to explain to patients the need to follow instructions from their chemist on storing and replacement of bottles. Poor treatment outcomes or greaterthan-expected adverse effects may be due to inconsistency in formulations inherent in compounding pharmaceuticals.
The latest multi-centre, randomised control trial with repeated low-level red-light therapy demonstrates this is a promising new approach in the management of myopia,18 with efficacy appearing to be in line with current interventions. This therapy employs desktop laser diode devices that emit longwavelength light (635–650 nm) that is used at home. The Eyerising myopia management device, which uses RLRL technology, has both TGA and New Zealand Medsafe approval, as well as regulatory approval in Europe, the UK, and China.
As a non-optical and non-pharmaceutical intervention, this expands the myopia management portfolio.19
RISK AND COMPLIANCE CONSIDERATIONS
Contact Lenses and Orthokeratology
Orthokeratology raises concerns due to the increased risk of microbial keratitis (MK), particularly as it is worn overnight. The incidence of MK with overnight wear of OK in children is noted to be about 13.9 per 10,000 patient years,20 which is slightly higher than the incidence associated with soft contact lens wear in children for daily wear (2.7 cases per 10,000 patient years).21 The risk of MK is, however, a mitigatable risk that can be minimised with regular followups, and education about the importance of lens care and hygiene practices. Due to the average age of school students, parents are usually closely involved with the care and maintenance of their child’s contact lenses.
Low-Dose Atropine
Atropine eye drops can cause adverse ocular effects such as photophobia and blurred near vision, which tend to become more frequent and severe with higher concentrations.22 There is anecdotal evidence and some limited literature suggesting that these side effects may be more pronounced in children with fairer complexions, though further research is needed to confirm this. For low-concentration atropine drops, such as 0.05% and 0.025%, around 20% of children report photophobia within the first two weeks of use.23 This incidence decreases to less than 8% by the end of the first and third years, indicating a trend of adaptation over time.24 Blurred near vision is another possible side effect, yet less than 2% of children in the LAMP (Low-Concentration Atropine for Myopia Progression) study required progressive addition lenses (PALs) in the first year of treatment, with this figure rising to about 10% by the third year.23,24 Long-term adaptation appears to mitigate these initial side effects.
Repeated Low-Level Red-Light Therapy
Adverse events with RLRL have mainly been monitored through questionnaires and assessments of best-corrected visual acuity, with limited use of optical coherence tomography (OCT) imaging for detailed retinal examination.25 A recent case report involving a 12-year-old girl revealed temporary vision loss and retinal changes after five months of RLRL treatment, including foveal damage and reduced macular autofluorescence, which improved after discontinuing the therapy for three months.26 (Editor’s note: See further, ‘Global Insights on Repeated Low-Level Red-Light Therapy for Myopia’, p79.) This underscores the need for enhanced monitoring using OCT and vigilant safety protocols to promptly detect and manage potential retinal issues, ensuring cautious and informed use of RLRL therapy.
IMPACT ON VISION QUALITY
Visual Acuity and Contrast Sensitivity
The newer myopia control lenses, such as highly aspherical lenslet (HAL) and defocus incorporated multiple segments (DIMS), can affect visual acuity and contrast sensitivity, particularly in conditions of lower contrast. While children usually adapt well to these lenses, there have been reports of some reductions in visual quality. These reductions are particularly noticeable in peripheral vision or in environments with low contrast, highlighting the need for consideration and monitoring when prescribing these innovative lens types.
Adaptation and Comfort
Most children adapt effectively to interventions like multifocal and dual focus lenses, experiencing minimal impact on their perceived visual quality or comfort. Both in clinical practice and research trials, children who wear these types of lenses have reported good adaptation and no significant visual impairment.
MANAGING THE FAST-PROGRESSING MYOPE
Opinions on first-line treatment for myopia differ between ophthalmology and optometry. The World Optometry Council recommends optical treatments, emphasising the importance of clear vision for school-age students. In contrast, the World Society of Paediatric Ophthalmology and Strabismus recommends atropine. Ultimately, regardless of the initial treatment prescribed, all approaches converge towards the same goal. Collaborative care between optometry and ophthalmology is essential for the best interest of the patient.
“ … for myopes greater than -6.00D, the risk of visual impairment by the age of 75 increases to 39% (representing a five-fold risk) ”
Given the context of managing myopia in children, particularly focussing on early intervention, the decision between starting with monotherapy, a stepwise approach, or immediate dual therapy should consider several factors. These include the child’s risk of rapid progression, the efficacy and safety profiles of available treatments, and the practicalities of managing and monitoring these interventions. There are three clinical options: monotherapy and change intervention as required; monotherapy first then dual therapy; and dual therapy from the start.
Monotherapy and Change Intervention as Required
Using a single-treatment strategy has several advantages, such as the ability to clearly assess its effectiveness without the confusion of multiple interventions. It also reduces the risk of potential side effects or complications that might arise from combining different treatments, making it easier for both the patient and their family to manage compliance and monitoring.
However, there are disadvantages as well; there might be a delay in achieving optimal control of myopia progression if the initial treatment isn’t sufficient.
This approach demands close monitoring to swiftly detect any inadequacies in controlling the progression and to make timely adjustments to the management plan.
Monotherapy First then Dual Therapy
This approach offers several advantages, starting with the simplicity of beginning with a single, less invasive treatment and the flexibility to escalate therapy (such as the addition of low-dose atropine) if needed. It allows for an initial evaluation of a simpler intervention before considering more dual therapy and establishes a clear pathway for progression if the initial control is not sufficient. However, there are some downsides. For instance, there may be a period of suboptimal myopia control if the initial monotherapy isn’t effective, before transitioning to a combination therapy.
Dual Therapy from the Start
The advantages of starting with a dual therapy include potentially lowering the risk of rapid myopia progression and severe cases of myopia, which is especially important for children at high risk, such as those with an early onset or a family history of significant myopia. Combination treatment of 0.01% atropine with OK is more effective.13 An early, robust intervention can also be more effective in slowing down the growth of the eye’s axial length in these high-risk scenarios.
On the downside, this approach complicates treatment management, demanding more from both the patient and their caregivers in terms of adherence and regular monitoring. There’s also a higher chance of experiencing side effects or complications due to the intensity and combination of treatments. This can be particularly tough for families, especially if the child is younger or has difficulty with certain treatments, such as atropine eye drops.
Regardless of which option is chosen, initiating myopia management as early as possible and close monitoring is key.
WHEN TO STOP
Myopia management can be approached through both optical and pharmaceutical strategies, with the decision to discontinue treatment depending on several factors, primarily the patient’s age and the rate of refractive error change. Myopia progression typically slows during late adolescence or early adulthood, but the exact age at which it stabilises can vary, sometimes extending into the 20s.27 A guideline for ceasing treatment is not straightforward but a stable refractive error and axial length growth may suggest that myopia progression has stabilised; the patient’s age being the caveat in this consideration. The COMET trial showed that 23% of myopes are still progressing at the age of 18; 10% at the age of 21; and 4% at the age of 24.27
When it comes to tapering off myopia control treatments, such as atropine, OK, or multifocal soft contact lenses, a key concern is the potential for a ‘rebound effect’. This phenomenon involves an acceleration of myopia progression once the treatment is discontinued. Managing this transition is important to prevent a rapid increase in myopia that could negate the benefits gained during treatment. Strategies for tapering treatments often involve gradual reduction and careful monitoring of the patient’s refractive status and axial length (every three months). A 2024 systematic review, that assessed the extent of rebound effects following the cessation of optical and pharmacologic myopia control interventions, is summarised below.28
Orthokeratology: Has strong rebound effects, which tend to slow down after five years. Because axial length growth can accelerate, it’s advised not to stop OK treatments before the age of 14. The rebound effect might be linked to a reversal in choroidal thickening, rebounding into choroidal thinning, or a loss of peripheral myopic defocus.
Multifocal Soft Contact Lenses: Show weak rebound effects, which are not statistically significant in several studies, although Chamberlain et al.29 found promising continued treatment effect over a six-year period.
Peripheral-Plus Spectacle Lenses: Variable rebound effects, making the outcomes not yet conclusive.
Atropine: Higher doses are associated with significant rebound effects. Recent trends recommend tapering off atropine rather than abrupt cessation to avoid the rebound phenomenon associated with sudden withdrawal. A practical approach is to prescribe low-dose atropine for two years initially.30 Consider stopping atropine if there is no significant progression in the second year. Re-introduce atropine treatment if myopia progression does not remain stable and continue until the progression rate decreases to less than 0.25D per year.
Repeated Low-Level Red-Light Therapy: Early findings suggest modest rebound effects.
It should be noted that there aren’t specific studies that comprehensively address the rebound and sustained efficacy of dual therapy treatments for myopia control, as this is a relatively new area of research. It would be reasonable to monitor closely and reintroduce intervention as appropriate.
CONCLUSION
Embracing an evidence-based approach to myopia management is crucial in modern optometry, ensuring that treatments are safe, effective, and personalised to each patient’s needs. By using high-quality evidence, optometrists can greatly improve patient outcomes, enhance safety, and build trust with their patients.
To earn your CPD hours from this article visit: mieducation.com/progressing-myopes-why-your-management-matters.
References
1. Holden, B.A., Fricke, T.R. Wilson, D.A., et al., Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042.
2. Bullimore, M.A., Ritchey, E.R., et al., The risks and benefits of myopia control. Ophthalmology. 2021;128(11):15611579. DOI: 10.1016/j.ophtha.2021.04.032.
3. Fricke, T.R., Jong, M., Resnikoff, S., et al., Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Br J Ophthalmol. 2018 Jul;102(7):855-862. DOI: 10.1136/bjophthalmol-2017-311266.
4. Bullimore, M.A., Brennan, N.A., Myopia control: Why each diopter matters. Optom Vis Sci. 2019;96(6):463–465.
5. Tideman, J.W.L., Polling, J.R., Klaver, C.C.W., Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018 May;96(3):301-309. DOI: 10.1111/aos.13603.
6. Lawrenson, J.G., Shah, R., Walline, J.J., et al., Interventions for myopia control in children: a living systematic review and network meta-analysis. Cochrane Database Syst Rev. 2023 Feb 16;2(2):CD014758. DOI: 10.1002/14651858.CD014758.pub2.
7. Zhang, X.J., Zaabaar, E., Yam, J.C., Advances in myopia control strategies for children. Br J Ophthalmol. 2024 May 22:bjo-2023-323887. DOI: 10.1136/bjo-2023-323887. Epub ahead of print.
8. Brennan, N.A., Toubouti, Y.M., Cheng, X., Bullimore, M.A., Efficacy in myopia control. Prog Retin Eye Res. 2021;83:100923.
9. Hou, P., Wu, D., Yang, G., et al., Comparison of the efficacy and safety of different doses of atropine for myopic control in children: A meta-analysis. Front Pharmacol. 2023 Sep 11;14:1227787. DOI: 10.3389/fphar.2023.1227787.
10. Wu, P.C., Yang, Y.H., Fang, P.C., The long-term results of using low-concentration atropine eye drops for controlling myopia progression in schoolchildren. J Ocul Pharmacol Ther. 2011;27:461–6.
11. Cho, P., Cheung, S.W., Retardation of myopia in Orthokeratology (ROMIO) study: A 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53:7077–7085.
12. Morgan, P.B., Efron, N., Woods, C.A., et al., International survey of orthokeratology contact lens fitting. Cont Lens Anterior Eye. 2019;42:450–454.
13. Tsai, H.R., Wang, J.H., Chiu, C.J., et al., Efficacy of atropine, orthokeratology, and combined atropine with orthokeratology for childhood myopia: A systematic review and network meta-analysis. J Formos Med Assoc. 2022 Dec;121(12):2490-2500. DOI: 10.1016/j.jfma.2022.05.005.
14. Nucci, P., Lembo, A., Evans, B.J.W., et al., A comparison of myopia control in European children and adolescents with defocus incorporated multiple segments (DIMS) spectacles, atropine, and combined DIMS/atropine. PLoS One. 2023 Feb 16;18(2):e0281816. DOI: 10.1371/journal.pone.0281816.
15. Jones, J.H., Mutti, D.O., Jones-Jordan, L.A., et al., Effect of combining 0.01% atropine with soft multifocal contact lenses on myopia progression in children. Optom Vis Sci 2022; 99: 434–442.
16. Tang, T., Lu, Y., Zhao, M., et al., Comparison of the long-term effects of atropine in combination with orthokeratology and defocus incorporated multiple segment lenses for myopia control in Chinese children and adolescents. Eye (Lond). 2024 Jun;38(9):1660–1667. DOI: 10.1038/s41433-024-02987-5. Epub 2024 Feb 28.
17. Lawrenson, J.G., Shah, R., Walline, J.J., Interventions for myopia control in children: A living systematic review and network meta-analysis. Cochrane Database Syst Rev. 2023 Feb 16;2(2):CD014758. DOI: 10.1002/14651858. CD014758.pub2.
18. Xu, Y., Cui, L., Zou, H., et al., Repeated low-level red-light therapy for myopia control in high myopia children and adolescents: A randomized clinical trial. Ophthalmology. 2024 Jun 5:S0161–6420(24)00318-X. DOI: 10.1016/j. ophtha.2024.05.023. Epub ahead of print.
19. Liu, H., Yang, Y., Guo, J., et al., Retinal damage after repeated low-level red-light laser exposure. JAMA Ophthalmol 2023;141:693–5.
20. Bullimore, M.A., Sinnott, L.T., Jones-Jordan, L.A., The risk of microbial keratitis with overnight corneal reshaping lenses. Optom Vis Sci. 2013 Sep;90(9):937–44. DOI: 10.1097/OPX.0b013e31829cac92.
21. Bullimore, M.A., Richdale, K., Incidence of corneal adverse events in children wearing soft contact lenses. Eye Contact Lens. 2023 May 1;49(5):204–211. DOI: 10.1097/ ICL.0000000000000976.
22. Gong, Q., Janowski, M., Luo, M., et al., Efficacy and adverse effects of atropine in childhood myopia: A metaanalysis. JAMA Ophthalmol. 2017 Jun 1;135:624–630.
23. Yam, J.C., Jiang, Y., Tang, S.M., et al., Lowconcentration Atropine for Myopia Progression (LAMP) Study: A randomized, double-blinded, placebocontrolled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019 Jan;126:113–124.
24. Yam, J.C., Zhang, X.J., Zhang, Y., et al., Three-year clinical trial of Low-concentration Atropine for Myopia Progression (LAMP) Study: Continued versus washout: Phase 3 report. Ophthalmology. 2022 Mar;129:308–321.
25. Xiong, R., Zhu, Z., Jiang, Y., et al., Sustained and rebound effect of repeated low-level red-light therapy on myopia control: A 2-year post-trial follow-up study. Clin Exp Ophthalmol 2022; 50: 1013–1024.
26. Liu, H., Yang, Y., Zhao, P., Retinal damage after repeated low-level red-light laser exposure. JAMA Ophthalmol. 2023 Jul 1;141(7):693–695. DOI: 10.1001/ jamaophthalmol.2023.1548.
27. COMET Group, Myopia stabilization and associated factors among participants in the Correction Of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013 Dec 3;54(13):7871–84. DOI: 10.1167/iovs.13-12403.
28. Chiu, Y.C., Tsai, P.C., Chiu, C.J., Systematic review of myopia progression after cessation of optical interventions for myopia control. J Clin Med. 2023 Dec 21;13(1):53. DOI: 10.3390/jcm13010053.
29. Chamberlain, P., Logan, N. Young. G., et al., Clinical evaluation of a dual-focus myopia control 1 day soft contact lens: 6-year results. 2020 American Academy of Optometry annual meeting.
30. Chia, A., Lu, Q.S., Tan, D., Five-year clinical trial on atropine for the treatment of myopia 2: Myopia control with atropine 0.01% eyedrops. Ophthalmology 2016;123(2):391-99. DOI: 10.1016/j.ophtha.2015.07.004.

SooJin Nam MOptom BOptom MBA (exec) is a part-owner of five Eyecare Plus optometry practices in Sydney and has a strong interest in three main areas: binocular vision dysfunctions, myopia control and orthokeratology. She was previously a director for both Optometry NSW/ ACT and Eyecare Plus and is a current member of the Australian Optometric Panel. She is a regular contributor to the optometry industry as a key opinion leader.