mifeature
The Legacy & Lessons of CFEH
16 Years of Impact

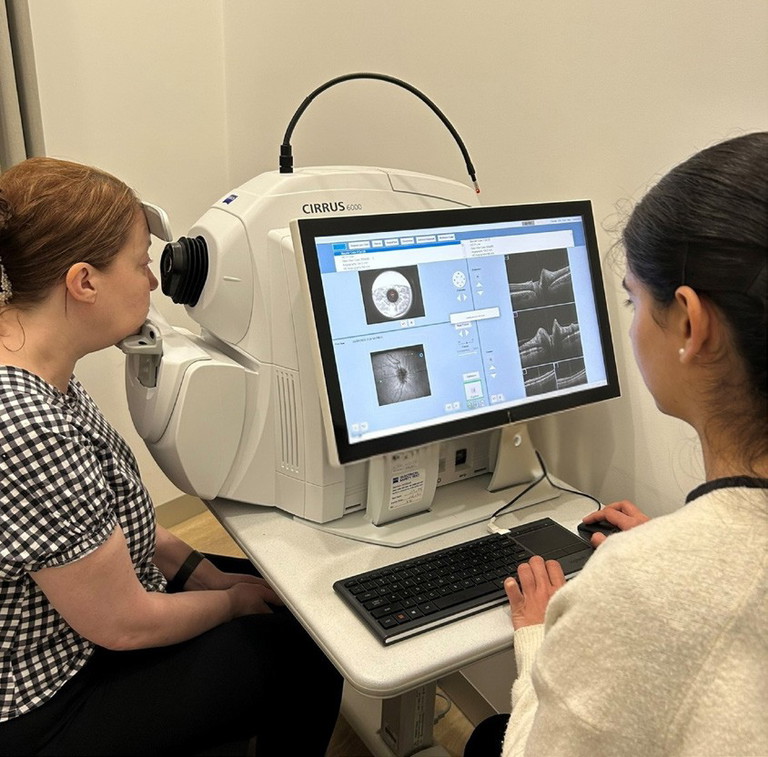
CFEH Clinical Technician Rubanni Nijjar taking OCT images at the Cameron Centre.
This month, the Centre for Eye Health (CFEH) clinical team will discharge its final patients, marking the end of 16 years of diagnostic and management service provision. Since its establishment in 2009, as a joint venture between Guide Dogs NSW/ACT and the University of New South Wales, CFEH has been at the forefront of collaborative care, education, research, and advanced diagnostics.
It has worked hand-in-hand with community optometrists, partnered with Prince of Wales Hospital (POWH) Ophthalmology to develop a Glaucoma Management Clinic (GMC), and through Westmead Hospital’s C-Eye-C program, delivered timely care for patients with glaucoma and diabetes.
In this article long-term members of the CFEH team review some of the organisation’s achievements and its legacy.
WRITER Sarah Holland
For over 15 years, Guide Dogs NSW/ACT has generously supported CFEH with the vision of reducing preventable blindness. With an aspirational strategy to create a world that is inclusive and accessible for people with low vision or blindness, Guide Dogs NSW/ACT has made the difficult decision to focus its efforts more closely on services and advocacy.
“Redirecting our funding will allow us to increase our low vision service offerings and expand our influence through social change and advocacy,” explained Guide Dogs NSW/ ACT CEO Dale Cleaver.
While operational priorities have been realigned, the value of CFEH to patients, optometrists, and the broader health system has consistently been recognised by Guide Dogs NSW/ACT. As CFEH General Manager Sarah Holland reflected, “Our health system is facing growing demand as the population ages, and collaborative care offers a clear path forward”.
“While there are pockets of excellence across the country, truly impactful collaborative care is still lacking due to reluctance to change and a funding gap. If we want these models to endure and expand, they need to sit within a framework of government funding so they can be delivered sustainably at scale.”

The original CFEH optometrists in 2009, from left: Paula Katalinic, Andrew Watham, Agnes Choi, Assoc Prof David Pye, Prof Michael Kalloniatis, George Rennie, and Michael Yapp. Absent: Anna Delmadoros.

CFEH Senior Staff Optometrist Sophia Zhang giving an education presentation on AMD to final year UNSW optometry students.

CFEH Kensington client services team: Natalie Borstein, Tanja Kegel, Michelle Chang, Ashleigh Neville, and Joanne Collier.
A SHIFTING INDUSTRY LANDSCAPE
Over the past 15 years, optometry has been transformed by the availability of imaging technologies in community practices. During this evolution, CFEH and other educational bodies played a central role, supporting optometrists to adopt new tools, interpret results, stay up to date with ocular disease research, and work effectively with ophthalmology.
More than 1,000 UNSW optometry students have benefited from work-integrated learning placements at CFEH, while the Centre’s continuing professional development programs built a national and international reputation. These efforts helped foster lifelong learning and raise the quality of community optometry.
The impact has been profound. Optometrists’ ability to manage chronic eye conditions, such as glaucoma, diabetic retinopathy, and age-related macular degeneration, has expanded enormously. Yet participation in collaborative care remains influenced by well-known barriers: equipment costs, financial pressures, practice location, time constraints, and practitioner confidence.
Continued development of collaborative care includes acknowledging the role for optometrists to provide community-based care as an alternative to early and potentially unnecessary entry to hospital clinics. This process can also expedite access for patients who truly need public hospital services when private care is not financially possible or not preferred.
For more than a decade, CFEH filled this role in New South Wales by providing intermediate-tier care that relieved pressure on the public health system. It became a vital resource for community optometrists, offering access to advanced imaging, diagnostic support, and disease management services, all delivered at no cost to patients thanks to Guide Dogs NSW/ACT’s backing.
The University of NSW, as the academic partner since 2008, has recognised the magnitude of Guide Dogs NSW/ACT’s investment and the vision it enabled. The joint approach was transformative and enabled a step change in clinical practice, research, and education.
DIAGNOSTIC FOUNDATIONS
CFEH began as a referral centre, created to provide advanced ocular imaging and diagnostic support when technologies like optical coherence tomography (OCT) were still new. From the start, UNSW’s involvement ensured research and education were central to clinical service. This framework supported patient care while creating an environment for professional development and well-focussed research.
Referring optometrists received detailed, evidence-based reports that guided their decisions and built their diagnostic skills. Collaboration with POWH Ophthalmology provided asynchronous and telehealth review where needed, supporting CFEH optometrists to work confidently within their scope. This model ensured optimal patient outcomes and strong professional growth for staff.
The collaboration between UNSW, CFEH, and the POWH yielded significant advances in research and education. Achievements included building a vast clinical database to refine diagnostic methods, and developing protocols and teaching resources that continue to benefit the profession.
COLLABORATIVE CARE IN ACTION
In 2016, CFEH expanded its role by working with Associate Professor Michael Hennessy, Professor Minas Coroneo, and Dr Katherine Masselos to establish the Glaucoma Management Clinic (GMC). Here, CFEH optometrists delivered frontline care for glaucoma patients, supported by ophthalmology when treatment needed to be initiated or escalated. Clear referral pathways ensured smooth access to surgical care and advanced disease management. This model significantly reduced hospital demand, allowing clinics to prioritise patients with severe glaucoma.
“The joint approach was transformative and enabled a step change in clinical practice, research, and education”

CFEH research team (2017) back row from left: Dr Jessie Huang-Lung, Cornelia Zangerl, Dr Nayuta Yoshioka, Dr Jack Phu, Dr Nicholas Tan. Front row: Dr Angelica Ly, Dr Barbara Zangerl, Prof Michael Kalloniatis, Dr Lisa Nivison-Smith, and Dr Agnes Choi.

CFEH clinical team (2019) back row from left: Dr Vincent Khou, Dr Angelica Ly, Dr Jack Phu, Dr Wilson Luu, Gonzalo Jacome, Dr Nayuta Yoshioka, Sophia Zhang, Dr Janelle Tong, Lindsay Moore, Elizabeth Wong, Jaclyn Chiang, Pauline Xu. Front row: Paula Katalinic, Henrietta Wang, Michael Yapp, Carol Chu, Dr Jessie Huang-Lung.

2025 Kensington clinical and management team, from left: Michael Yapp, Gonzalo Jacome, Tania Lu, Sarah Holland, Pauline Xu, Aleena Hamid, Tania Seligmann, Nicole Lawson, Irene Wei. Absent: Michele Clewett, Meri Galoyan, Sarah Liao, Lindsay Moore, Sophia Zhang.
Collaboration extended further in 2020 through Westmead Hospital’s Community Eye Care (C-Eye-C) program, led by Professor Andrew White. Patients with glaucoma or diabetic retinopathy referred to Westmead were examined by optometrists, with ophthalmologists reviewing results electronically. Referral protocols ensured that only patients needing escalation attended hospital clinics.
A peer-reviewed study published in 2020 found that 68% of patients seen through C-Eye-C did not require an ophthalmology appointment, while per-patient costs were 43% lower through the collaborative pathway.1 CFEH contributed around 1,000 appointments annually to this model, again easing hospital wait times and improving access for those in greatest need.
Clinic Operations Manager Michael Yapp, who helped lead these collaborations, explained, “Roadblocks to entry to the public hospital system confront community optometrists every day”.
“Establishing new collaborative models requires funding and champions for change. For pathways to be effective and efficient, two key factors are pivotal: well-defined protocols and effective communication. At CFEH, success came from refining protocols to reflect the latest research and building strong partnerships between hospitals, optometry, and patients, supported by reliable communication through secure e-platforms and My Health Record.”
EDUCATION AND KNOWLEDGE SHARING
Beyond direct care, CFEH has left a profound educational legacy. With a database of more than 65,000 patients, its clinicians developed unmatched expertise in imaging and ocular disease diagnosis. This expertise was shared widely through CPD lectures, workshops, webinars, telehealth consultations, and resources such as the CFEH Chairside References and Atlas, which will continue to support the profession into the future.
UNSW students also benefited greatly. CFEH clinicians taught posterior eye disease to third-year students, delivered lectures, grand rounds, and journal clubs, participated in oral examinations, and hosted final-year students on six-week rotations. These placements provided practical training in advanced imaging and disease management, leaving a lasting impact on optometry education.
A Message from Optometry Australia
Collaborative models, such as those pioneered by CFEH, have been shown to be safe, efficient, cost-effective, and strongly supported by patients. We need to embrace models of care that allow optometrists and ophthalmologists to work in truly collaborative arrangements, where optometrists work to their full scope of clinical practice. By doing so, we not only expand access to timely, high-quality eye care, but also ensure that our limited healthcare resources are used in the most effective way possible.
Skye Cappuccio, Chief Executive Officer, Optometry Australia.
ADVANCING THE KNOWLEDGE BASE
While clinical service was CFEH’s foundation, research soon became integral. Under the leadership of former Centre Director Professor Michael Kalloniatis, CFEH developed a research agenda focussed on identifying optimal models of integrated care and creating new diagnostic protocols.
The GMC itself provided fertile ground for research, enabling development of new testing protocols supported by multiple research grants.
By the numbers, CFEH’s research record is impressive:
• 168 peer-reviewed articles since 2013, many in leading journals.
• 2,526 citations and an H-index of 29 (Web of Science).
• AU$7.2 million in research funding from competitive and other grants.
• 11 PhD and six MSc completions, with three PhD students still in progress.
For a relatively small organisation, these outputs are extraordinary. By training clinician-scientists and publishing widely, CFEH has contributed lasting advances to vision science and clinical practice.
WHAT COMES NEXT?
In the lead-up to the closure of CFEH, the team has worked tirelessly to transition patients into new care pathways. Regulatory and funding challenges make embedding integrated care within public hospital systems slow, but efforts continue to apply CFEH’s lessons to new models.
The UNSW Optometry Clinic, located alongside CFEH, is well placed to take on many GMC patients, ensuring continuity of care and providing valuable training for students. Other integrated care models exist across Australia but remain fragmented and locally driven. Despite advocacy to the NSW Government, a unified, state-supported framework remains absent.
A CALL FOR SYSTEMIC CHANGE
Public hospital outpatient ophthalmology services are under enormous strain, with wait times exceeding a year in some NSW districts. These delays risk patients experiencing preventable vision loss.
As Optometry NSW/ACT Professional Services and Advocacy Manager Paula Katalinic points out, “Evidence shows that collaborative care pathways involving optometrists and ophthalmologists are patient-centred, cost-efficient, and an effective use of healthcare resources”.1
“We urge the NSW Government to evaluate CFEH models that can be replicated at relatively low cost and with immense benefit to patients: from those with suspected disease to those requiring ongoing chronic management. The closure of CFEH, in particular its western Sydney clinic, will be sorely missed by optometrists, patients, and students alike.”

2025 Cameron Centre team: Helene Ly, Tania Lu, Cinzia Giufre, Carol Chu, Nicola Lee, Jessica Sheaves, and Rubanni Nijjar. Absent: Judy Nam, Henrietta Wang.
The major barrier is funding. Medicare rebates do not adequately cover advanced imaging and diagnostic services, private charging risks excluding the most vulnerable, and internal hospital collaborative models that are emerging in other states struggle to find both funding and space. CFEH’s message is that well-targeted, state-level investment is essential to establish and sustain these pathways.
CLOSING THOUGHTS
As one of Australia’s most significant collaborative eye care initiatives closes its doors, a legacy of innovation and impact is left behind. CFEH reduced waitlists, improved patient outcomes, advanced understanding of ocular disease, trained a generation of optometrists, and reshaped professional education.
Its legacy is not only in the patients cared for, or the students trained, but in the roadmap it has provided for the future of Australian eye care. The challenge now is to embed sustainable, government-supported collaborative care models that build on CFEH’s lessons for decades to come.
This article was written by Sarah Holland with significant contributions from Michael Yapp and Michele Clewett. The author would like to acknowledge valuable input and review by Professor Lisa Keay, Professor Michael Kalloniatis, Paula Katalinic, and Skye Cappuccio.
Sarah Holland is the General Manager of Centre for Eye Health. Ms Holland has a background in developing strategy; reviewing and redesigning patient pathways; developing and delivering financial targets; and a strong HR focus. She is originally from the United Kingdom, where she completed her tertiary studies, including a MSc in Health, Leadership and Management. Ms Holland spent 15 years working in the National Health Service with a focus in oncology prior to moving to Sydney several years ago where she initially worked within the private sector.
Reference
1. Tahhan N, Ford BK, Angell B, et al. Evaluating the cost and wait-times of a task-sharing model of care for diabetic eye care: a case study from Australia. BMJ Open 2020;10:e036842. doi: 10.1136/bmjopen-2020-036842.