mieducation
Evidence-Based Contact Lens Practice: Part One A Review from BCLA CLEAR
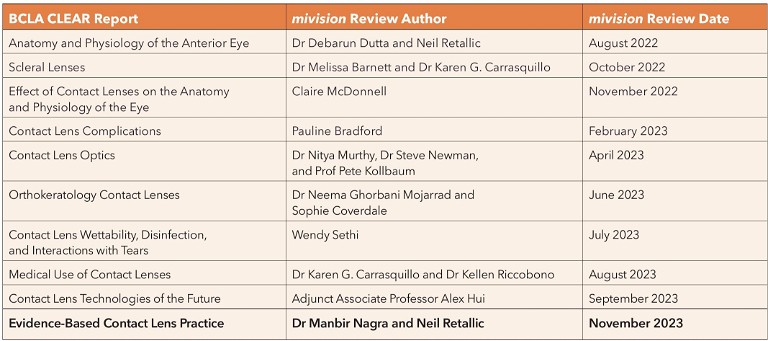
In the tenth of a series of articles summarising the key findings of the BCLA CLEAR publication, a major review of the published evidence relating to all aspects of contact lens practice, Dr Manbir Nagra and Neil Retallic offer an overview of the section on evidence-based contact lens fitting. This article comprises two parts, with part two to follow in a later issue of mivision.
WRITERS Dr Manbir Nagra and Neil Retallic
LEARNING OBJECTIVES
On completion of this CPD activity, participants should be able to:
1. Realise the need to integrate best research evidence with clinical expertise and patient values,
2. Understand how a patient’s history and symptoms contribute to successful contact lens prescribing,
3. Realise the role of lens material, design, and modality in achieving comfort and compliance, and
4. Be aware of the need to continuously review and update contact lens practices.
In December 1986, the LA Timespublished an article highlighting an outbreak of acanthamoeba keratitis.1 The number of cases had been growing for some time and both professional bodies and the media were taking note.
So, what led to this unfortunate episode? Well, in part, us! To combat ocular irritation induced by preservative treated lens solutions, well-intentioned eye care practitioners (ECPs) had been advising patients to make their own saline at home instead. This episode illustrates how the approaches we adopt, and may consider acceptable practice at the time, can look a lot less favourable in the face of evidence. As the old adage goes, hindsight is always 20/20.
So, which of our current practices are destined for the history books? And how can we, as ECPs, ensure our current practices are evidence based?

Figure 1. Fundamental elements of evidence-based practice (based on Wolffsohn et al., 2021).2
We often hear the phrase ‘evidence-based practice’ (EBP) and may assume it involves considering scientific evidence alone, but the BCLA CLEAR report on EBP describes how scientific evidence should be integrated with clinical expertise, practice context, and individual patient values (Figure 1).2 The report highlights how scientific evidence itself is often stratified into a hierarchy, ranging from robust randomised clinical trials through to clinical case reports, but ultimately each approach comes with its own merits and limitations (Figure 2). In short, not all science is the same.
Figure 2. Hierarchy of clinical scientific evidence (Wolffsohn et al., 2021).2
The report also provides an opportunity to address inconsistencies in terminologies and favoured descriptors used by the Federative Committee on Anatomical Terminology (FCAT), such as renaming Bowman’s and Descemet’s membranes as the anterior and posterior limiting lamina respectively. The term rigid corneal lenses (RCL) was preferred to support differentiation from scleral lenses and ‘planned’ or ‘sporadic’ ‘overnight wear’ were deemed more appropriate representations for clinical use.
In this issue of mivision, we discuss some of the highlights from the BCLA CLEAR EBP report with respect to contact lens fitting, and we consider areas of clinical practice that may warrant an update. In a later issue of mivision we will delve further into the BCLA CLEAR EBP report to focus on subsequent contact lens reviews and aspects that influence retention.
What is Evidence-Based Practice?
The integration of best research evidence with clinical expertise and patient values to inform decision making by practitioners to provide better tailored patient care.
HISTORY AND SYMPTOMS
To begin, history and symptom taking can be used to elicit reasons for a patient’s visit, identify any key concerns, and inform management decisions and lens choice. The main motivations for contact lens wear typically stem from a desire to improve cosmesis, for use when playing sports, or to improve optics.
Information gathering can also be conducted by remote virtual methods or using questionnaires ahead of the consultation.
ANTERIOR EYE EXAM
Slit Lamp Biomicroscopy
Although easy to overlook its importance, a comprehensive slit lamp examination provides essential baseline data that can be useful when monitoring ongoing anterior eye changes. While video slit lamps have been around for Figure 3. A broad list of areas to cover during history and symptom taking. decades, smartphone camera mounting systems have more recently become available and there seems to be a growing possibility that diagnosis systems powered by artificial intelligence (AI) will eventually reach our exam rooms.
Less commonly, other imaging equipment can be used to assess anterior eye health and/ or contact lens fitting (Figure 4).
Anterior Eye Grading Scales
Most ECPs (>80%) use some form of anterior eye grading scale or photography to facilitate recordkeeping and communicate findings with patients. A grade change of more than one unit is typically considered clinically significant. While ECPs have previously been encouraged to grade in increments of 0.1, more recent evidence supports grading to the nearest 0.5 as being as accurate, and better, than just one-unit intervals. Grading scales are not without their shortcomings. In practice it is worth remembering that scales are not interchangeable, thus the name of the grading scale used ought to be recorded.
Ophthalmic Dyes
Sodium Fluorescein
Since excess fluorescein can impede the amount of fluorescence, the recommended approach is to use a drop of saline on the paper strip and then remove the excess liquid by shaking. Ideally, assessment ought to be undertaken one to three minutes after instilling the dye. Fluorescence can be observed using a blue light, with a peak of around 495nm, and enhanced using a yellow filter, with a sharp cut-off at 500nm.
Lissamine Green
Lissamine green has largely superseded the use of Rose bengal. For Lissamine green ophthalmic strips, it is recommended that the saline drop be left on the strip for a minimum of five seconds. Assessment may begin one to four minutes following instillation. The ocular surface can be assessed under white light, and visualisation of the dye enhanced using a red-free filter.
OCULAR SURFACE MEASUREMENTS AND LENS SELECTION
A range of ocular surface measurements are typically taken prior to lens fitting. While most measurements can be reasoned as essential for determining first choice lens parameters, their value may be called into question if the eventual lens is mass produced and thus most lens parameters are fixed; e.g., back optic zone diameters (BOZD) for a typical soft lens. Nevertheless, baseline measures can facilitate the future monitoring of ocular surface changes.
The main measurements for lens parameter selection are listed below. Additional considerations relating to lens modality, lens material, and lens type will also influence eventual lens selection.
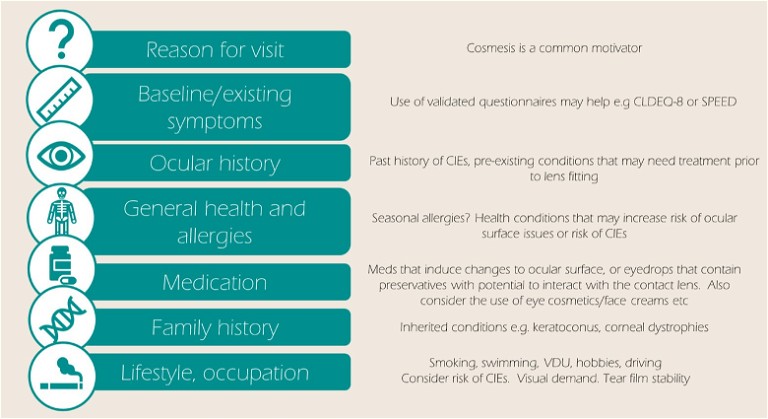
Figure 3 lists some of the major areas covered when history and symptom taking.
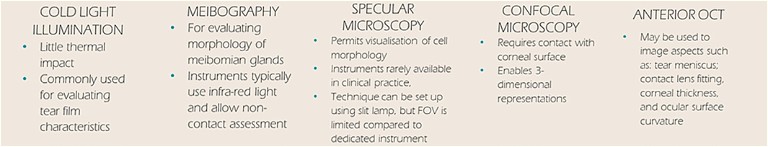
Figure 4. Anterior eye imaging techniques other than slit lamp biomicroscopy.
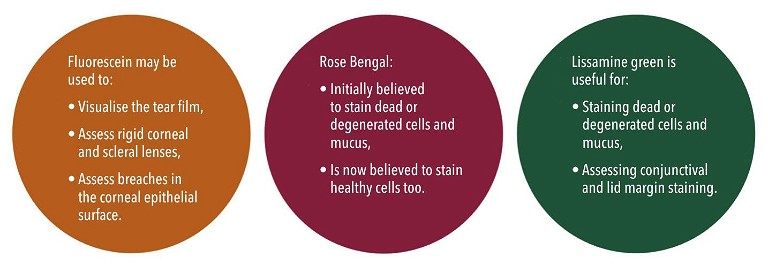
Figure 5. Applications of diagnostic dyes.
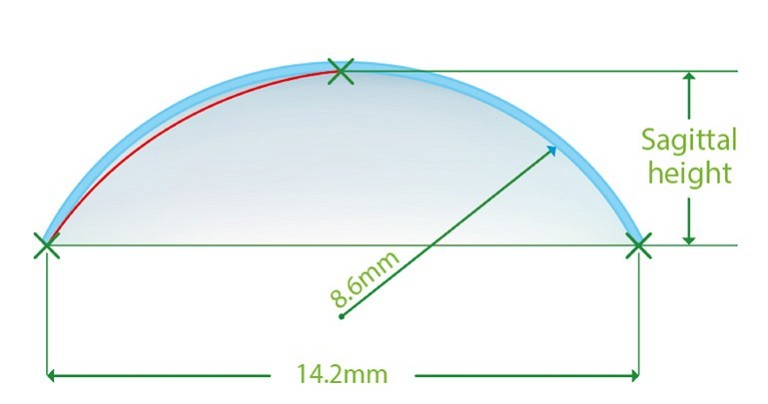
Figure 6. Illustration of sagittal height.
Horizonal Visible Iris Diameter
Horizonal visible iris diameter (HVID) refers to the horizontal distance between nasal and temporal limbi. Conventionally measured using a ruler or slit lamp graticule, ECPs with access to equipment such as biometers and corneal topographers will have noticed that many of these machines allow objective measures of HVID. It should be noted however, that HVID values can differ significantly depending on the method of measurement.
Typical adult values range between 10– 14mm, with an average of 11.8±0.5mm.
What the science says: The BCLA CLEAR EBP report acknowledges that there is little published evidence to inform soft lens diameter choice. It is commonly accepted that interactions between the lens edge and limbal area must be avoided.
For rigid corneal lens neophytes, changing the lens diameter is not found to confer any benefits during the initial adaption process.
Vertical Palpebral Aperture
Defined as the vertical fissure between superior and inferior lid margins with the eyes in primary gaze, vertical palpebral aperture (VPA) typically measures 9.7±1.2 mm with a range of 9.1–10.8 mm.
What the science says: A surprising finding of the BCLA CLEAR EBP report was the lack of published evidence describing the relevance of VPA to lens fitting.
Pupil Size
Pupil size is typically measured under room and mesopic lighting conditions, often with a ruler, although pupillometers and other objective approaches are available. Average values in adults range from 2.0–7.0mm in bright light to 4.0–8.5mm in dark. Numerous factors can influence pupil size including luminance, accommodation, convergence, age, and refractive status.
What the science says: Pupil size may be important for bifocal and multifocal lens performance, yet some studies have shown that patient performance and preference for different multifocal lenses were unaffected by pupil size.
Corneal Shape
The sagittal height of the cornea and lens inform lens fitting, but in the absence of these measurements, we have widely relied on corneal curvature to estimate lens base curve. While traditional manual topographers typically only measure the central 3mm, modern topographers and computer software programs can now model the full eye shape profile.
Sagittal height refers to the distance that the contact lens ‘stands off ’ the eye, such as the perpendicular space between the lens back surface and the cornea (Figure 6). The larger the sagittal depth, the tighter the lens. Altering the lens diameter and/or base curve can influence this and make the contact lens looser or tighter.
Characterising corneal shape at baseline can help monitor changes over time and, although of less relevance to soft lenses, can identify the presence of corneal astigmatism.
What the science says: The limited number of base curves available for mass produced soft contact lenses can be used successfully for approximately 75–90% of eyes; the remainder may require a custom designed lens.
For rigid corneal lens fitting, corneal topography is typically used for back optic zone radius (BOZR) selection and can be used to show the effects of a decentred lens. The eccentricity values produced from video keratography are a better predictor of base curve to corneal relationship than central keratometry readings alone.
Lens Power
The BCLA CLEAR report reminds us that trial frame/phoropter mounted prescriptions require conversion to the corneal plane equivalent. For prescriptions under 4D the difference in power is likely small and so spectacle power may be used as a starting point. Mean spherical power can be used for spherical lenses, but where required, toric corrections can provide improvements in visual quality.
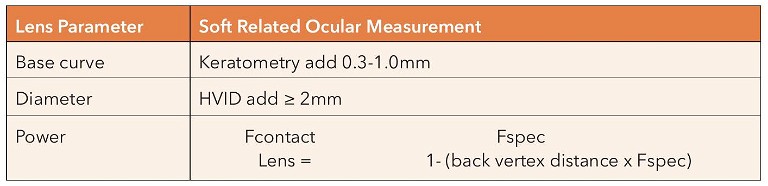
Table 1. Estimating soft lens parameters.
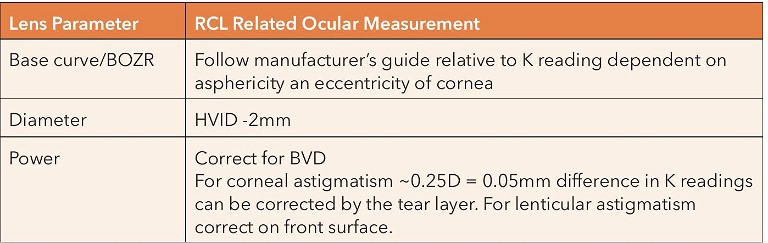
Table 2. Rigid corneal lenses.
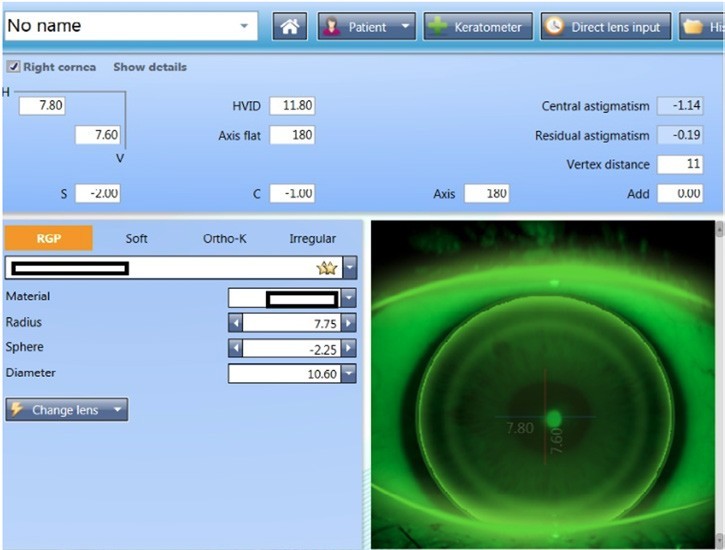
Figure 7. Lens selection and predicted fitting pattern using computerised software.

Figure 8. Predicted fitting pattern appearances on the same eye with 0.3 adjustments to the radius, showing a flat and steep fit respectively.
Computerised software can support lens selection, making the process simple. It can also be used to generate expected fitting pattern profiles and predict the lens fitting behaviours (Figures 7 and 8).
LENS MATERIAL, DESIGN, AND MODALITY
Most new lens fits are soft lenses, which is possibly reflective of short adaptation and fitting processes, wide availability, and the strong performance they can offer. In 1998, it was predicted that by 2010 we would see the demise of rigid lenses. 3,4
Rigid corneal lenses are still very much available and in use as they can be more effective for those with ocular pathology and high corneal astigmatism; are associated with lower levels of some contact lens complications; are used for orthokeratology; and show better tolerance in patients with dry eye and papillary conjunctivitis compared to soft lenses.
There has also been a recent surge in scleral /mini scleral prescribing, especially for medical / therapeutic use, those with poor acceptance to other lens types, and dry eye sufferers. More details on these were covered earlier in mivision’s BCLA CLEAR series.
Contact lens wear with good compliance carries a low risk of serious complications.5 Soft daily disposable contact lenses may be the preferred choice for individuals with higher risk of corneal infiltrative events or those who favour convenience.
The influence of soft lens material is unclear except for when high oxygen transmissibility is the goal (for overnight wear, or for those considered to have a high swelling response to hypoxic conditions, high prescriptions, or potentially for therapeutic use).
EVALUATING FITTING AND ASSESSING VISUAL PERFORMANCE
Soft Lens Fit
Assess the contact lens fit approximately 10 minutes after application following guidance in Figure 9.
• Observe contact lens surface, wettability, and quality,
• Use a fitting cross to denote any decentration relative to the corneal centre,
• Assess post-blink movement in up-gaze: ideal values are 0.25 to 0.50mm,
• Assess horizontal lag: the change in overlap of lens onto limbus should ideally be 0.5–1.0mm,
• Assess push up recovery speed: ideally this should be 2−4mm/s or non-sluggish, visible recovery,
• Ask for a comfort score from 0 (poor comfort) to 10 (can’t feel),
• For toric lenses, assess the position of orientation markings, compensating for any rotation using the CAAS rule (Clockwise Add, Anticlockwise Subtract) or LARS rule (Left Add, Right Subtract). Assessments of the marker in both the primary position and during different directions of gaze is useful. Physically rotating the lens can also help ascertain rotational stability to judge the recovery of the toric marker back to the starting position.
Visual Performance
• Even a cyl of 0.75D can impact visual performance, thus the difference between a toric and mean spherical equivalent ought to be demonstrated to the patient.
• For multifocals, assessing sensory dominance (determined by which eye is most adversely affected by a +1.50D add during binocular distance viewing) is recommended.
• For complex optical lens designs, real world tasks may provide a better assessment of visual experience than clinical objective measures.
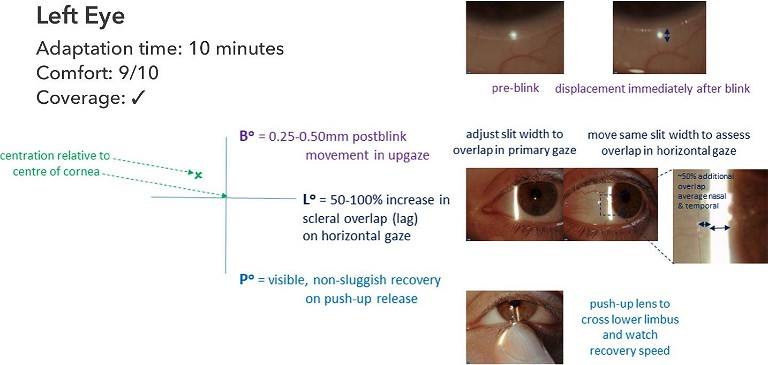
Figure 9. Recording of a soft lens fit.
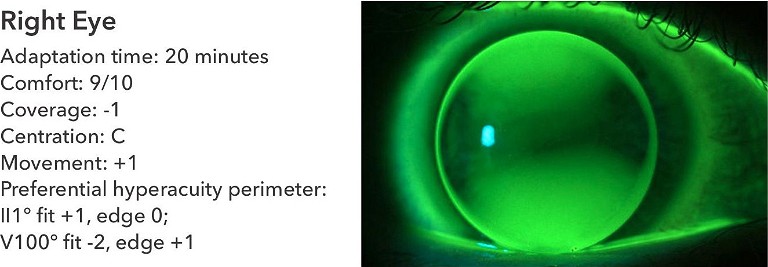
Figure 10. Representation of the recording systems.
Rigid Corneal Lens Fit
Rigid corneal lenses should be fitted to create an alignment in at least one meridian, distributing the weight of the lens over a larger area of the cornea and forming a tear fluid layer of 10–25μm between the back surface of the lens and the anterior surface of the cornea.
Compared with soft lenses, the fit is dynamic with greater lens movement and tear exchange across the ocular surface. The refractive properties of the post lens tear film typically become part of the optical correction and the post lens tear layer profile is easily visualised with fluorescein. Any dark areas indicate contact or close alignment with the cornea, corresponding to a tear layer <20μm. In contrast, as the tear layer volume increases, fluorescence will be brighter and broader.
For rigid corneal lenses, assess the fit around 20 minutes after lens application to allow for adaption and for reflex tearing to subside. The following summarises the recording scheme advised in the BCLA CLEAR report (Figure 10):
• Observe the contact lens surface, wettability, and quality.
• Gain a comfort score rating (0–10).
• Assess the positioning and coverage: how much smaller when compared to the HVID (+2 to -2). Is the lens lid attached?
• Assess the dynamic centration. Ideally this stays within the limbus (C), rather than crossing the limbus (L) or the edge encroaching on the pupil in dim light (P).
• Record the movement on inter-blink, scales relate to millimetres. 0.5–2.0mm could be acceptable.
• Following white light assessment, the fluorescein pattern underneath the lens should be observed within 30 seconds to three minutes of instillation. When the lens is centred in the primary position, assess the centre, mid-periphery, and edge regions.
Five Clinical Pearls for Contact Lens Fitting
1. Obtain information from the patient that will inform lens choice, including lifestyle, environmental, and visual demands.
2. Assess the eye, ocular surface, and consider the impact of general health conditions and medications.
3. Gather clinical data to inform lens selection and for baseline comparisons (use grading scales).
4. Fit the best visual solution, sphere, toric (0.75D and above) or multifocal.
5. Ensure that lens recommendations (modality, design, and material) match with patient preferences, clinical findings, and needs.
ADVANCED CONTACT LENSES
Previous articles have reviewed lens fitting principles that fall beyond the scope of this article. These include:
Scleral/Mini Scleral Lenses
Fitted to vault over the entire cornea, including the limbus, scleral and mini scleral lenses land on the conjunctiva overlying the sclera. Broad indications fall across the entire corneal disease spectrum, i.e., irregular corneas and ocular surface diseases as well as refractive correction in healthy eyes.6
Orthokeratology
Fitted to temporarily redistribute the corneal tissue, orthokeratology lenses use reverse geometry rigid corneal lenses when worn overnight, enabling the wearer to be free of any refractive correction during the daytime. 7
Medical Contact Lenses
Medical contact lenses are fitted for the primary purpose of treating an underlying state or complicated refractive status. 8 For keratoconus, an even distribution is desired when using rigid lenses, otherwise known as the three-point touch approach.
CONCLUSION
The BCLA CLEAR EBP report highlights several areas where clinical conventions deviate from the science, suggesting a possible need to review and update current practices. It is also important to consider other factors, such as patient values and preferences, alongside the science.
The BCLA CLEAR EBP report serves as a reminder to all practitioners of our obligation to keep abreast of changes in the field. Our summary of clinical pearls for contact lenses (left) makes one thing ‘clear’: The clinical norms in force at the start of an ECP’s career are unlikely to resemble those by the end!
Look out for part two of the BCLA CLEAR EBP summary, which will build on aspects of the contact lens journey following the fitting.
To earn your CPD hours from this article visit mieducation.com/evidence-based-contactlens-practice.
The full report and supplementary information can be accessed at contactlensjournal.com/article/S1367-0484(21)00022-9/fulltext.
The BCLA CLEAR Summary report is a short bite-size evidenced-based practical guide for clinicians, bringing together the key findings from the report. Accessed via CLEAR (bcla. org.uk).
The Podcast of BCLA CLEAR Evidence-based contact lens practice can be found by scanning the QR code, or visit: anchor.fm/bcla/episodes/BCLA-CLEAR-Podcast-1---Evidencebased-practice-e179tp5.
Acknowledgement and recognition to James Wolffsohn, Kathy Dumbleton, Byki Huntjens, Himal Kandel, Shizuka Koh, Carolina Kunnen, Manbir Nagra, Heiko Pult, Anna Sulley, Marta Vianya-Estopa, Karen Walsh, Stephanie Wond, and Fiona Stapleton who were the paper’s authors and the educational grants from Alcon and CooperVision.
Original paper: Wolffsohn, J.S., Dumbleton, K., Huntjens, B., Kandel, H., Koh, S., Kunnen, C.M.E., Nagra, M., Pult, H., Sulley, A.L., Vianya-Estopa, M., et al., CLEAR -Evidence-based contact lens practice. Contact Lens & Anterior Eye: The Journal of the British Contact Lens Association 2021, 44, 368–397, doi:10.1016/j.clae.2021.02.008.
The editors for this series are Neil Retallic and Dr Debarun Dutta.
References available at mieducation.com

Dr Manbir Nagra is an optometrist, educator, and researcher based in the United Kingdom. She works as an independent consultant within the optical sector.

Neil Retallic is an optometrist with experience working in practice, education, industry, and head office roles. He currently works for the College of Optometrists in the United Kingdom and Specsavers and is the Immediate Past President of the British Contact Lens Association.