mitechnology
Manual Marking in a Digital Era: The Torix System
As demand for toric intraocular lenses (IOLs) continues to grow, surgeons worldwide are grappling with the challenge of achieving consistent, accurate alignment while maintaining efficient surgical workflows. Although digital marking systems have garnered significant attention, experienced surgeons recognise that manual marking systems remain a vital component of modern cataract surgery.
Dr Peter Macken, a comprehensive eye surgeon based in Bowral in the NSW Southern Highlands, has been at the forefront of this conversation. With a professional focus on cataract surgery, he identified early challenges with toric IOL marking that led him to develop the Torix single-use toric IOL marking and alignment system. His sterile, disposable system represents a thoughtful approach to addressing real-world surgical challenges.
mivision spoke with Dr Macken about his development of the Torix system, its clinical applications, and the continuing relevance of manual marking in an increasingly digital surgical environment.

Figure 1. The Torix preoperative marking tool.
Q. What specific challenges in toric IOL marking led you to develop the Torix system?
When I started implanting toric IOLs in 2009, there were limited options available for marking the eye preoperatively and aligning the IOL intraoperatively. I found that the reusable instruments were expensive to purchase, prone to breakage, varied in functional design, and were not always available to be used when needed. This was especially true when I had multiple cataract cases requiring toric IOLs on a surgical list.
I clearly remember situations where instruments weren’t ready, surgical cases were delayed, and lists were rearranged while reusable instruments were sterilised. It was a frustrating time. I could see the promise and potential of toric IOLs for patients, but the instrumentation was a limitation. I like consistency and simplicity, and having the same system for every case makes it much easier for patient flow.
To address these problems, I decided that a low-cost, sterile, single-use tool was needed for accurate marking, alignment, and maintaining surgical efficiencies. I wanted it to be designed and manufactured in Australia. I am pleased that the Torix system was designed by Outerspace Design and manufactured by Medical Manufacturers Pty Ltd, both in Melbourne.
Q. How do the two components of the Torix system work together to achieve accurate toric IOL positioning?
The Torix system comprises two components; the preoperative marking tool (Figure 1) labelled 1 on the package, and the intraoperative alignment guide (Figure 2) labelled 2 on the package. Both are separately packaged and sterile. This means the tools are always ready to be used. The marking tool is used (sterile) preoperatively. It has a proprietary edge to assist with ink transfer to make the reference marks on the patient’s surgical eye. When I am marking, I use illuminated spectacles or surgical loupes to assist the marking process, with the patient sitting up and looking straight ahead. An assistant holds up the superior eyelid, during the marking (which takes a few seconds). The alignment guide is opened in theatre, and placed on the operating instrument table, when needed, for the eye that was marked previously. I usually mark the steep corneal meridian with an inked instrument (at both points 180° apart, at the start of the case) and proceed then with phacoemulsification in the usual way. This alignment marking step takes less than a minute.
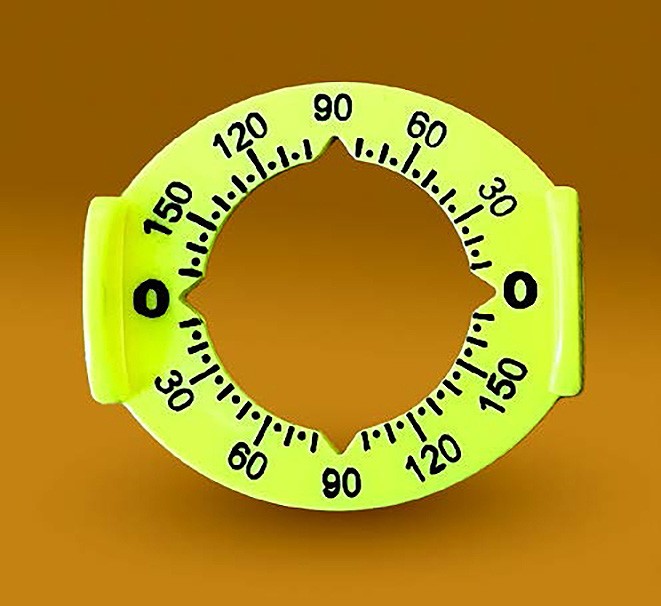
Figure 2. The Torix interoperative alignment device.
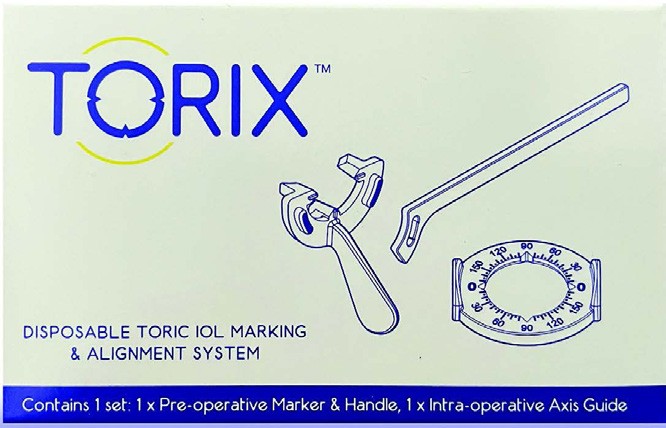
Figure 3. The Torix system.
Having accurate preoperative measurements, validated calculations that consider posterior corneal astigmatism and surgically induced astigmatism (SIA), and accurate alignment at surgery, are all important for patient outcomes when using toric IOLs.1 The accuracy of manual marking requires good patient cooperation and precise technique.2 The Torix system is no different, relatively intuitive, and proficiency can be attained quickly. The cataract surgeon may choose to delegate the preoperative marking to an anaesthetist after appropriate training. One of my regular anaesthetists is highly skilled in manual marking and does this for me. This is most efficient, with zero loss of time.
Q. In what clinical situations do you find manual marking with Torix provides advantages over digital technologies?
There is a misconception that digital marking is more accurate than manual marking. Numerous recent studies of cataract surgery with toric IOLs and surgery for phakic toric IOLs, have found that accurate manual and digital systems, when compared, have similar clinical outcomes.3 Some studies have reported that manual marking (compared to digital systems) may have better uncorrected distance visual acuity (UDVA), higher percentages of IOLs within 0–2° of target alignment, and reduced aberrations, such as trefoil.2,3
That said, if manual marking is done poorly, then of course this will affect results. However, digital marking does not guarantee success, either.4
From personal experience, I know digital marking systems can sometimes fail. This can be for a variety of technical reasons, such as failure to obtain an appropriate preoperative, qualified anterior segment image or intraoperative matching errors. If I cannot be confident that a system will be accurate or available every time, I will not use it. I would much prefer to be very close manually, than digitally inaccurate.
Q. How does the single-use, pre-sterilised nature of Torix address healthcare system challenges?
Not all hospitals / surgical facilities have access to digital marking systems or on-site slit lamps. This may be more common in smaller, rural and regional centres.2 This digital capability is expensive, and often beyond the budgets of chronically stressed resources. Also, some hospitals have rationalised sterilisation processes to a remote site. As a result, instruments are processed ahead of time. This may lead to instruments not being available when needed, which may affect surgical list flow / efficiencies. Patients should still be able to benefit from toric IOLs if a hospital / surgical facility does not have a digital marking system, on-site slit lamp, or use off-site sterilisation of instruments. It is still possible to do cataract surgery with toric IOLs using the Torix system. Toric IOLs are one of the best options to assist patients in seeing better, reducing spectacle dependence.1
Q. How has Torix proven valuable for training young surgeons in toric IOL implantation?
In my view, it is important for emerging cataract surgeons to learn various techniques. Learning how to mark accurately manually, with a simple and reliable method, is a good foundation. If a surgeon prefers digital marking, but it fails for whatever reason, accurate surgery can still proceed with manual marking, so long as the correct technique is used.
Q. How does Torix provide a reliable backup solution when digital systems might fail?
I operate in public and private facilities, and work with several excellent anaesthetists. I always do cataract surgery with intravenous sedation and some form of local anaesthesia. The local anaesthesia and sedation may vary depending on which anaesthetist is involved. When I operate on patients after sub-tenon’s local anaesthesia, conjunctival haemorrhage or swelling is common, making accurate digital image matching of blood vessels impossible. Despite this, I can still use the Torix system, every time. Viscoelastic on the cornea and pterygia, and eye rotation, can all affect digital image matching too.
Q. What feedback have you received about clinical outcomes with Torix?
The Torix system is functionally equivalent to reusable manual marking systems, with the advantage of a proprietary edge on the preoperative marking tool, similar functionality for right and left eyes, and 5° increments on the alignment tool. At the start of each calendar year, I audit my first 30 consecutive real-world cataract cases. In these audits, all cases had monofocal IOLs, and emmetropia was the refractive target. I included cases with ocular comorbidities. I used recent European Registry of Quality Outcomes for Cataract and Refractive Surgery (EUREQUO) data as the benchmark and presented the findings to colleagues in our local area health network. In the audit of 2023 (50% toric IOL cases) and 2024 (59% toric IOL cases), I had identical findings. Mean uncorrected distance visual acuities (UCDVA) were superior in patients with monofocal toric IOLs (mean UCDVA = 6/6.9), compared to patients with monofocal non-toric IOLs (mean UCDVA = 6/7.7). I recently reviewed my last 100 cataract cases, and currently, I insert just over 50% toric IOLs and am approaching 20% EDOF (extended depth of focus) IOL insertion.5
We conduct routine patient satisfaction surveys on all cataract cases at our practice.6 Preparing for this interview, I looked at completed surveys over the past month. There were 52 completed surveys; 98% of patients were satisfied, moderately satisfied, or extremely satisfied with their postoperative vision. Sixty-three per cent were extremely satisfied. These patients are de-identified, with various IOLs (monofocal and EDOF) and independent of postoperative visual acuity, but it appears postoperative vision is meeting or exceeding expectations. It is reassuring to find high satisfaction rates with postoperative vision; it validates our preoperative, operative, and postoperative processes. It also compares favourably with a recent publication of satisfaction rates with EDOF IOLs.7
I have had positive feedback from a number of colleagues who use the Torix system, which has been commercially available in Australia for over 10 years. Each year we continue to sell more products than the previous year.
Q. What role do you see for manual marking systems like Torix as digital technologies continue to advance?
Cataract surgery demand continues to increase, and so too does the demand for simultaneous astigmatism correction. There is no question that we are in the EDOF IOL era. With the increase in popularity of EDOF IOLs, comes the responsibility and expectation of delivering good uncorrected vision to our patients.
It is vitally important that astigmatism is minimised.1,7 The market is large enough for manual marking systems to continue to play an important role in addressing astigmatism correction at the time of cataract surgery, phakic toric IOL surgery, or toric IOL re-alignment.8
The major source of error in astigmatism management at cataract surgery is preoperative corneal measurement, followed by intraoperative alignment and then IOL tilt.9 Preoperative measurements, with three separate devices and optimisation of the corneal surface, to determine the magnitude and meridian of astigmatism, is ideal. Despite this, astigmatic outcomes can still deviate from preoperative predictions.4
It is possible to achieve <0.5D of refractive astigmatism in about 80% of patients, and <1.0D of refractive astigmatism in 100% of patients.4 In future, it is hoped we can achieve more than 90% of our patients with <0.5D of refractive astigmatism. We need to continue to optimise our preoperative measurements, our calculations of astigmatic magnitude and meridian, which consider the effect of (SIA), posterior corneal astigmatism, and accurate toric IOL alignment at surgery. Efforts in all these areas will continue to improve the visual outcomes for our patients. We are very fortunate to work in Australia, where toric IOLs play an important role in our cataract patients. There are excellent online calculators and nomograms to improve our outcomes in our toric IOL patients.10-13 It certainly is an exciting time for astigmatism management with cataract surgery.
“There is no question that we are in the EDOF IOL era”
This article is sponsored by SurgiVision, distributor of the Torix system in Australia and New Zealand.
References available at mivision.com.au.