mieducation
Ocular Imaging on OCT:
A Technical Masterclass
Centre for Eye Health (CFEH) has been operating, in part, as an imaging centre since 2009. Each year, approximately 70 final year optometry students from the University of New South Wales undertake a clinical rotation at CFEH, working alongside the team of optometrists to capture images and scans, mostly on elderly patients.
This article takes learnings from these many years of imaging and teaching to provide advice and generalised troubleshooting tips and tricks for acquiring optical coherence tomography (OCT) scans in more challenging circumstances. The ultimate goal is to reduce operator and patient-dependant errors, and obtain images and scans that clearly define present pathology for the sake of diagnosis, monitoring and management.
WRITER Rubanni Nijjar
LEARNING OBJECTIVES
On completion of this CPD activity, participants should:
1. Understand the importance of good signal strength and high scan quality to facilitate accurate image interpretation,
2. Understand when and why disabling ‘eye tracking’ can be beneficial to image capture in some patient cohorts, and how to achieve good scans,
3. Identify the most appropriate scan for imaging particular disease conditions, retinal locations, and for specific patient cohorts, and
4. Know how to troubleshoot and overcome imaging artefacts.
The growing prevalence of OCT in optometric practice has brought with it enormous advantages in terms of diagnosis and management of eye disease, ensuring better health outcomes for patients.1 Utility of this technology and accuracy of data obtained from it is, however, highly dependent on the acquisition of high-quality scans. This often comes down to the skill, experience, and knowledge of the operator.
Evidence shows that low signal strength and low scan quality can cause under reporting of tissue thickness,2,3 with a higher chance of artefacts.4 This leads to misinterpretation and misdiagnosis, highlighting the importance of quality scans.
As we know, no two patients are the same, and despite careful preparation and forethought, individual patient challenges will always arise. Understanding how your device works, patient cooperation, having good attention to detail, and knowledge about the anatomy of the eye assists in achieving quality scans. While scan modules may vary between manufacturers,2 this article provides general advice applicable to all OCT models with the aim of upskilling ophthalmologists, optometrists, orthoptists, technicians and students in the art of OCT imaging. Please note, to view all the images associated with this article, refer to the online version.*
EQUIPMENT PREPARATION
It is important that your device is regularly serviced, calibrated, and cleaned – especially the lens – to be able to achieve consistency in quality. (Refer to manufacturer advice for cleaning instructions).
A smudged lens, typically from patient noses, is common but can have a similar appearance in the scan to a media opacity (cataracts, floaters, corneal pathology) and so is commonly ignored (Figure 1, online*). To differentiate between a media opacity and a smudged lens, pay close attention to the ‘movement’ of the shadow:
• If the shadow does not move with the patient’s eye, clean the lens and retry.
• If it moves with the patient’s eye and in the direction of gaze, it is most likely due to media opacity.
TRACKING
All later generation OCT devices have the option of ‘eye tracking’ and an option to ‘track to prior scan’. Using this latter function can greatly assist with recalling settings from previous scans, saving time and ensuring follow-up scans are accurately positioned.
While eye tracking reduces acquisition errors, blink artefacts5 and subsequent loss of transient data, it may not completely avoid motion artefacts due to a longer scan duration. Eye tracking may be turned off for faster acquisition and higher quality scans in more complex presentations (hazy media, peripheral locations, elderly or young patients with concentration limitations, etc). When keeping tracking off, you must ensure the patient’s fixation is steady for the duration of the scan (Figures 2–4, online*).
PATIENT SETUP VARIATIONS
While a standard patient setup with clear instructions will typically enable acquisition of quality scans in an efficient manner, there are situations when variations may be used to enhance the outcome.
For example, dropping the chin rest entirely (not used) in cases of hunched backs, broad upper bodies and body tremors.
For non-English speaking background communities:
• Explain what they will see and where to look with minimal words and clear hand cues,
• Show a picture of the target on a paper to give them an idea of where they need to fixate, and
• Consider keeping a copy of instructions in multiple languages for patients to read or use translation applications on a device for when an interpreter is not present.
When working with elderly people or testing fatigue:
• If a patient is dilated, keep room light on to reduce ‘sleepiness’.
• If a patient’s eyelids are droopy (such as in cases of ptosis and dermatochalasis) and obstructing the scan area, gently lift the upper eyelid using a cotton tip or your finger to get a clear view of the posterior pole. If required, use a second assistant to hold the patient in place and lift the eyelid (Figures 5 and 6, online*).
• Give the patient regular breaks and blinks as required and consider using lubricating eye drops (refer to dry eyes section).
When working with a younger patient who may be curious, hyperactive or have a low attention span:
• Keep the patient occupied with the ‘red light, green light’ method. Instruct them to look at the green light. Tell them if they stay still long enough, the light will turn red, OR you can tell them ‘not to move’ when the red lights appear.
SCAN ALIGNMENT
Following correct patient setup, optimised alignment of the scan frame over the area of interest is necessary to avoid de-centration or motion and vignette artefacts, which cause inaccurate analysis and result output by the device.2,5
To ensure your scan is aligned correctly:
• Aim to position the area of interest along the ‘centre line’. For example, if it is a macular scan, the fovea must be aligned with the centre line.
• Ensure the B-scan is clear and enhanced for maximised contrast.
• Keep ‘tracking to prior scan’ on to mirror and assess changes in macular pathologies.1 Ensure the patient is looking directly at the fixation target to obtain accurate comparisons between visits.
SCAN SELECTION (POSTERIOR POLE)
Knowing when and how to use the different scan patterns through a specific area of interest can help reduce artefacts and enhance diagnostic outcomes. To select the ideal scan type, it is important to know the different modifications available. Knowledge of the anatomy of the eye is also required so that you can best instruct the patient’s gaze and be able to place the scan grid over the area of interest.
While the standard macula and disc cubes are useful in most cases, alternate modified scans, used appropriately, can illicit additional or higher quality information in some ocular conditions, such as:
Raster-line scans: Quick and high-resolution B-scans through the area of interest.
Radial: Presence of macular pathology such as macular oedema, epi-retinal membranes, lamellar macular holes, and for optic disc anomalies and swelling (Figure 7A, right, and Figures 8 and 11, online*).
Angiography: Presentations of age-related macular degeneration, diabetic retinopathy, vascular pathologies, optic neuropathies, glaucoma, and retinal nerve fibre layer (RNFL) defects (Figure 7C, right).
Additionally, further modifications to standard scans can be made to better image targeted and specific pathologies:
Density/volume and length: Adjust based on the width or depth of pathology in the area of interest (Figure 10, right).
Single vs multiple line raster: Acquisition time differs. A single raster is better to acquire peripheral scans, for example.
Direction: Direct through changing pathology. For example, use a vertical line scan through the macula for high myopes (Figures 9 and 22, online*).
Enhanced depth imaging (EDI): Enhanced visualisation of the choroid and choroid-scleral interface,5 such as for imaging choroidal naevi and pachychoroid diseases (Figure 10, below, and 11, online*).
PERIPHERAL OCT
While central scans are relatively straightforward, peripheral scans often suffer from lower resolution on OCT. However, several techniques can help optimise scan quality.
Patient fixation: Begin by asking the patient to look at the central fixation target, then move the target towards the area of interest (as far as it goes). At this point, turn on the external fixation light and position it in the desired direction.
Finally, ask the patient to look at the external fixation light and acquire a scan with eye tracking off if necessary.
• Choose a narrow raster in a single direction over larger volume blocks.
• Reduce the patient’s head movement while following the fixation target in most situations, noting that it may help to turn their head when scans are required in the far periphery, as this allows more control and minimises end-point nystagmus.
• Allow frequent blinks and breaks, as required, to minimise fatigue.
• Allow gradual movement of fixation to the periphery for smoother following by the patient.
• Turn eye tracking off for quicker image acquisition, making sure the gaze is steady and there is no blinking.
• Change the direction of the scan. This will enable you to capture as much as possible in one scan to determine the nature of pathology (Figures 12 and 13, online*).
• Knowledge of the disease process and presentation will guide you in what to look for and capture (e.g., knowing the difference in presentation between retinoschisis and retinal detachment will enable you to identify an appropriate scan pattern, direction and location to collect information that best supports clinical diagnosis) (Figure 14, top right).
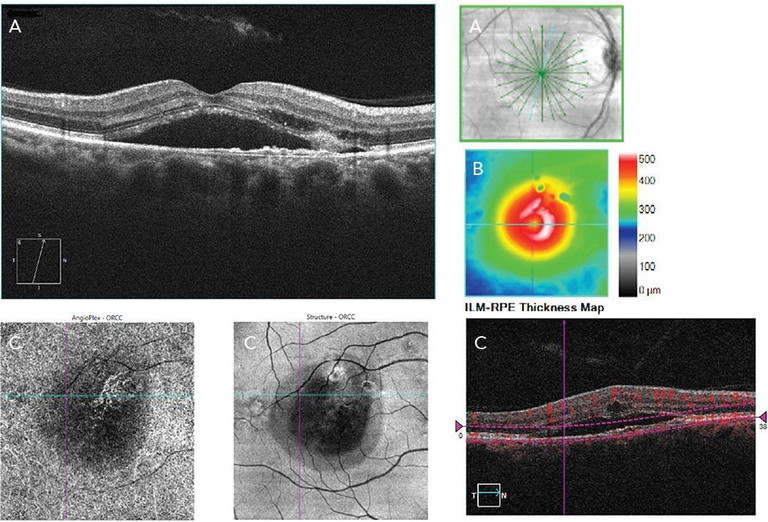
Figure 7. Multimodal use of OCT investigating exudative pachychoroid neovasculopathy. A) radial scan through macula, B) inner limiting membrane retinal pigment epithelium thickness map from macular cube scan, and C) angiography 6x6 analysis of the outer retina to choriocapillaris layer.
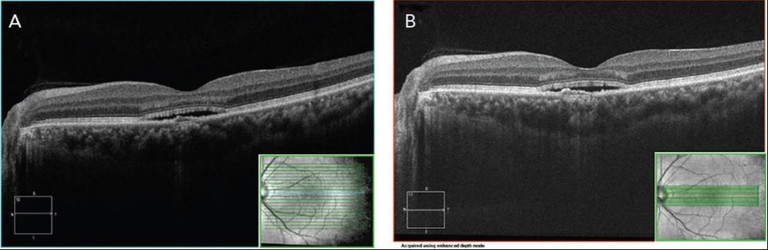
Figure 10. A) Standard B-scan raster through the macula, B) EDI on a dense volume raster through the macula to investigate possible pachychoroid neovasculopathy.
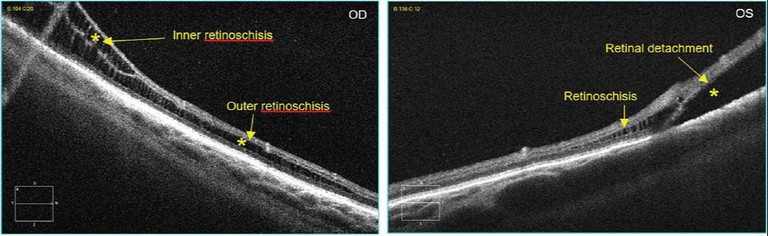
Figure 14. Scan location can assist with acquiring information needed to make a clinical diagnosis.
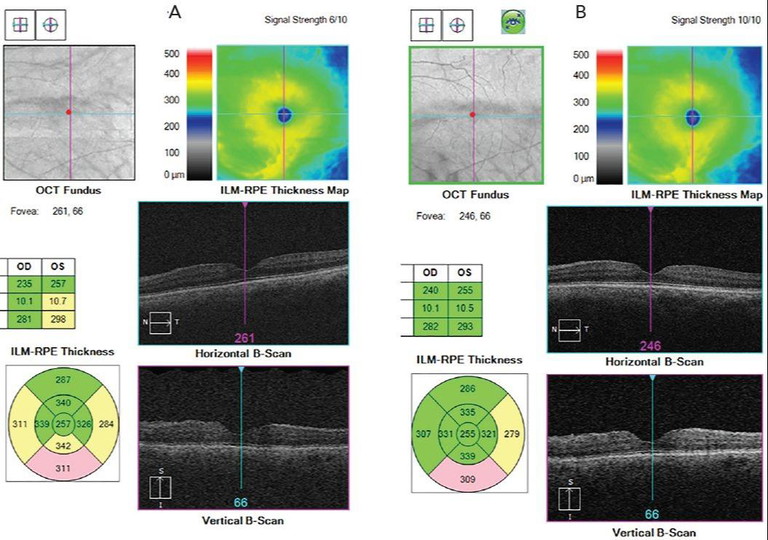
Figure 20. Macular cube scan. A) Scan results before lubricating eye drops were instilled with a signal strength 6/10, B) scan results taken after Systane Ultra preservative-free lubricant drops instilled, with improvement in signal strength to 10/10 and higher contrast. ILM-RPE thickness raw data is also impacted.
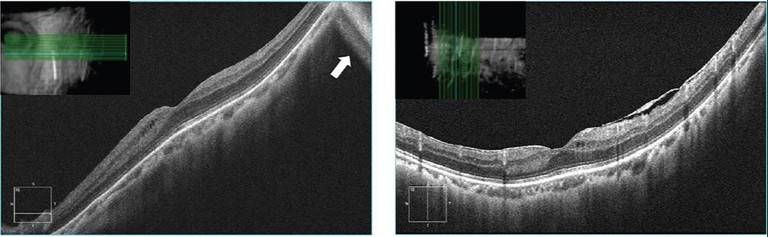
Figure 23. Volume B-scan repeated by adjusting scan direction by 90°, reducing mirror artefacts and achieving higher contrast.
SMALL PUPILS AND NO DILATION
Quality OCT scans are still often possible in patients with small pupils, or without using dilating drops.3 The most common artefacts from small pupils are vignetting and truncation due to pupillary reactions (Figures 15 and 16, online*).
Some methods you can apply to acquire high-quality scans with small pupils include:
• Minimise external sources of light entering the eye by covering light sources in the room,
• Close/occlude the fellow eye to allow further dilation of the eye undergoing scans,
• Position the scan frame in the centre of the pupil, where it is least affected by pupillary reactions, which can cause shadowing due to loss of signal by the iris blocking light, and
• Consider acquiring scans in different locations (with the artefacts present). This can assist with manual interpretation of areas that are not clear, or areas that are too difficult to image without the presence of artefacts.
OPACITIES
Media opacities include cataracts, floaters, corneal pathologies and tear film instability. Below are some tips to work around these opacities when acquiring scans.
Cataracts and corneal pathologies: Allow maximal dilation and ‘fish around’ to find an area within the pupil with the most enhanced and high contrast view of the B-scan, rather than only the ‘clarity/brightness’ of the fundus. Additionally, consider turning eye tracking off, while reminding the patient to be as steady as possible (Figure 17, online*).
Vitreous floaters: Focus on the area of interest and, if a floater is obstructing the scan frame, instruct the patient to look in different directions (one at a time) then look back at the target (Figure 18, online*). Assess which gaze direction moves the floater out of the frame for the duration of the scan to limit interference. Capture the scan by instructing the patient to look in that direction of gaze, then back at the target.
For optic nerve head scans, manipulate the floater to move it outside the temporal-superior-nasal-inferior-temporal curve. This will ensure the best possible RNFL data analysis.
DRY EYES
Dry eyes are a very common issue, causing low-quality imaging, affecting the signal strength and focus, and causing banding artefacts (Figure 19, online*). If you pay attention to the patient’s tear film when focussing on the pupil, you may see signs of dryness, or you may also notice the B-scan contrast change with each blink – this is usually a sign of dry eyes or quick tear film breakdown. Given the high prevalence of dry eyes in adult and elderly populations, the use of artificial tears or lubricating eye drops may help with acquiring quality scans.
Tips to keep in mind with dry eyes are:
• Consider doing OCTs prior to other imaging, or instil lubricating eye drops after performing contact procedures (gonioscopy and tonometry) and prior to OCT imaging,
• Use liquid eye drops, which create minimal visual disturbance as they are thin and watery, rather than gel drops or ointments (the thick consistency may affect OCT signal strength or create temporary visual disturbance) (Figure 20, middle left), and
• Allow patients to keep their eyes closed between scans and ask them to blink once before you capture the scan.
HIGH MYOPES
Staphylomas are common in high myopes, and may cause mirror, segmentation and band artefacts (Figures 21 and 22, online*).
After appropriate patient setup and scan alignment, it helps to:
• Allow maximal dilation of the pupil,
• Manually adjust focus on the OCT to match the subjective refraction,
• Reduce the scan length or change the scan direction (vertical, 90°) to enable ‘flattening’ of the scan by running along, rather than across retinal maximum curvature (Figure 13, online* and 23, bottom left),
• In the case of very high myopia that exceeds the device focus range, use contact lenses for OCT, and
• Turn tracking off if necessary.
EXISTING PATHOLOGY
Existing or changing pathology can influence scan acquisition and quantitative results, especially for low-quality scans. This will affect the diagnosis and management of diseases.3,6
To track changes in pathology over subsequent follow-ups, it is ideal to keep the ‘tracking to prior scan’ function on, allowing you to assess changes in the same location. A word of caution however: often when capturing scans through a previous location, the device may not place the scan accurately due to patient-dependent factors (e.g., difficulties with fixation) or due to a significant change in the pathology causing the structures to appear different. While turning ‘tracking to prior scan’ off may give better quality scans, this must be balanced with the need for accurate change analysis.
It is critical to assess the fundus images to ensure the scan area is in the same location as previous when analysing change (Figure 24, online*).
OTHER HURDLES
Patients with low vision or nystagmus may present OCT image acquisition challenges. Those with low vision may not be able to see the target and those with nystagmus may not be able to fixate on the target, leading to image truncation. Some handy hacks to minimise artefacts for these patients are:
Nystagmus:
• Turn the patient’s head to find the null fixation point where possible. This will reduce or stabilise the saccades.
• If turning the head to find the null point does not work, try patching the fellow eye.
• Manually position the scan frame at the area of interest and turn tracking off for quicker acquisition. This tip is useful provided steady fixation is possible for the duration of the scan.
• Consider reducing the scan density to take quicker scans.
Low vision:
• Use an external light source or visible object for them to fixate with the better eye.
• If using an object, such as a hand for the patient to follow, keep room lights on for easier visibility.
• If necessary, ask them to look straight ahead and manually adjust the scan frame.
• Turn tracking off for quicker acquisition, but only if the patient can hold a steady gaze.
CONCLUSION
Given the importance of OCT in clinical diagnosis and management, we hope this article serves as a valuable resource for achieving high-quality scans. The flowchart (Figure 25, below) outlines the general steps you would follow to acquire OCT scans in practice. It also encapsulates the hurdles and troubleshooting tips discussed in this article.
* To view all figures and earn your CPD hours from this article, visit: mieducation.com/ocular-imaging-on-oct-atechnical-masterclass.
References
1. Hunter L. Optimizing your OCT. Review of Ophthalmology, 10 Oct 2022. Available at: reviewofophthalmology.com/article/optimizing-your-oct [accessed Sept 2025].
2. Reimold J, Wroten C. OCT interpretation for glaucoma: Don’t get fooled. Review of Optometry, 15 Jul 2021. Available from: reviewofoptometry.com/article/oct-interpretation-for-glaucoma-dont-get-fooled [accessed Sept 2025].
3. Hardin JS, Taibbi G, Vizzeri G, et al. Factors affecting cirrus-HD OCT optic disc scan quality: A review with case examples. J Ophthalmol. 2015;2015:746150. doi: 10.1155/2015/746150.
4. Anvari P, Ashrafkhorasani M, Falavarjani KG, et al. Artifacts in optical coherence tomography angiography. J Ophthalmic Vis Res. 2021 Apr 29;16(2):271-286. doi: 10.18502/jovr.v16i2.9091.
5. Feldman BH, Kozak A, Tripathy K, et al. Optical coherence tomography, American Academy of Ophthalmology, July 2025. Available at: eyewiki.org/Optical_Coherence_Tomography [accessed Sept 2025].
6. Chhablani J, Krishnan T, Sethi V, Kozak I. Artifacts in optical coherence tomography. Saudi J Ophthalmol. 2014 Apr;28(2):81-7. doi: 10.1016/j.sjopt.2014.02.010.
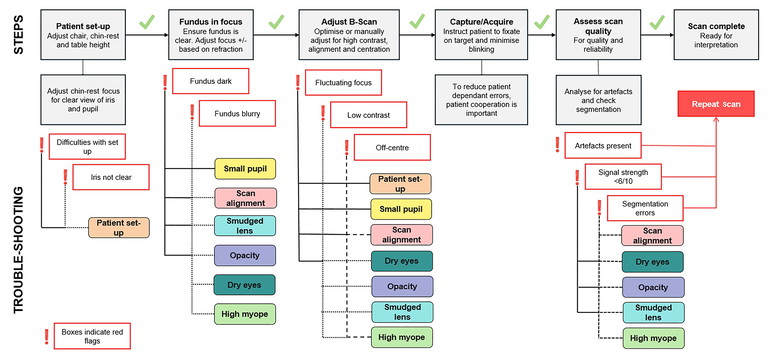
Figure 20. Macular cube scan. A) Scan results before lubricating eye drops were instilled with a signal strength 6/10, B) scan results taken after Systane Ultra preservative-free lubricant drops instilled, with improvement in signal strength to 10/10 and higher contrast. ILM-RPE thickness raw data is also impacted.

Rubanni Nijjar BVisSc MPH graduated from the University of New South Wales in 2019 with a Bachelor of Vision Science and obtained a Master of Public Health degree while working at the Centre for Eye Health. She has a strong interest in ocular imaging as well as promoting eye health awareness and patient education for all, but particularly for vulnerable populations, Indigenous communities and those from non-English speaking backgrounds.