mitechnology
A Longer Reach for Axial Length
WRITERS Professor David A Mackey AO, Dr Samantha Lee, and Dr Gareth Lingham
A study presented by the Lions Eye Institute at the Association for Research in Vision and Ophthalmology (ARVO) meeting in May highlighted the increasing importance of measuring axial length when looking at change in myopia rates over time.
HISTORY OF AXIAL LENGTH MEASUREMENT
While the relevance of axial length in the focus of the eye has been long known, with Alvar Gullstrand winning the 1911 Nobel Prize in Physiology or Medicine for his work on the dioptrics of the eye,1 it was not possible to measure axial length in vivo until the development of A-scan ultrasounds by Mundt and Hughes in 1956.2 And it wasn’t until the 1980s that ultrasound became widely used to measure axial length.
While axial length is most used for calculating intraocular lens power, this measurement is now being leveraged for managing paediatric myopia. Although ophthalmologists have had access to optical biometry for many years, with the IOLMaster 300 released by Carl Zeiss Meditec in 1999,3 not many optometrists have access to axial length-measuring devices.
Almost all treatment trials in paediatric myopia management use axial length as an outcome measure, along with cycloplegic autorefraction. Despite this, population data on axial length is limited, particularly in children and young adults. We previously published axial length and spherical equivalent refraction data for 5,938 individuals aged five to 89 years from eight Australian studies.4 Participants were classified as emmetropes, myopes, or hyperopes. Two regression model parameterisations (piecewise and restricted cubic splines) were applied to the cross-sectional data to analyse the association between age and axial length. These results were compared with longitudinal data from the Raine Study, in which participants’ axial length was measured at age 20 years and 28 years.
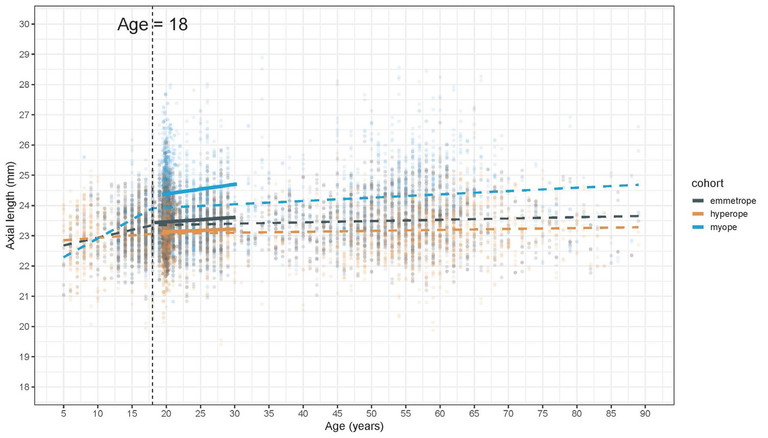
Figure 1. Cross-sectional axial length measurements from eight studies with best fit for myopic, emmetropic, and hyperopic eyes (dashed lines). Solid lines represent the two time points at age 20 years and age 28 years of the Raine Study.
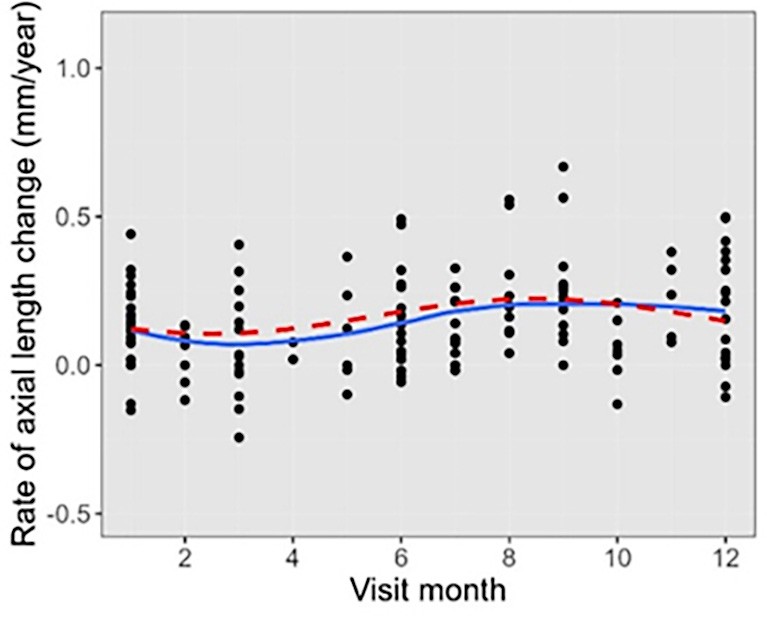
Figure 2. Axial length and month of examination from the control arm of the Western Australia Atropine for the Treatment of Myopia (WA-ATOM) Study, with lowest growth around February and greatest growth around August.
Looking at the cross-sectional data, a piecewise regression model (with one knot) showed that myopes had a greater increase in axial length before 18 years by 0.119 mm/year (P < 0.001) and after 18 years by 0.011 mm/ year (P < 0.001), compared to emmetropes and hyperopes (Figure 1). Similar results were shown with the restricted cubic splines model (with three knots). The longitudinal data from the Raine Study revealed that, when compared to emmetropes, only myopes showed a significant change in the axial length in young adulthood (by 0.016 mm/year, P < 0.001).
These data indicate that in emmetropic and hyperopic individuals, axial length stabilises around the age of 18 years but can continue to increase over this age in myopic individuals. Thus, while axial eye growth is normal in childhood and in teenage years, axial length can also be used as a measure of myopic progression in children and young adults.
RESEARCH ON AXIAL LENGTH IN CHILDREN
Data on axial length in children is limited and mainly available for children with myopia enrolled in clinical trials. Data from the WA-ATOM study5 showed that there was greater axial elongation over the winter months compared with the summer months (Figure 2). This is important to consider when evaluating the effectiveness of any treatment where there will be minimal progression over summer, with children spending less time in school and more time outdoors, both of which are well known environmental contributors to myopia.
With primary school-aged children from generation three in the Raine Study and from the ORIGINS study – both resident in Perth, Western Australia – we have commenced six-monthly examinations to determine actual axial length trajectories for children. With 250 children enrolled already, we hope to continue to expand the Raine and ORIGINS studies and continue this biometric assessment over the next four years to determine axial length trajectory as a predictor of myopia. As axial length is shorter in females than males (children and adults), we need to create both male and female axial length trajectories as is done for children’s height and weight. Indeed, height is correlated with axial length, and we are measuring children’s height in our studies to examine the relationship between height and weight.
RESEARCH ON AXIAL LENGTH IN ADULTS
Data on axial length is widely available on many patients seen in clinics around the world. These data can be used to determine if there is a population increase in axial length over time. When comparing myopia rates in adults in the Blue Mountains Eye Study and Melbourne Visual Impairment Project in the 1990s with those in the 2010s, the Busselton Healthy Aging Study and the Raine Study generation one were confounded by the changing rates of cataract surgery.6 Increased outdoor time increases the likelihood of cataracts but decreases the likelihood of myopia. However, myopia also increases the likelihood of cataracts. Early cataract can result in a lenticular myopia. Post-cataract surgery, most patients are emmetropic and thus the true refractive error may not be available. Thus, excluding people who have had cataract surgery may skew the data in either direction. In contrast, axial length is known and relatively constant after cataract surgery.
In a study presented at ARVO in May this year, we reviewed de-identified axial length measurements (IOLMaster700, ZEISS, USA) from 9,793 individuals taken between 2017–2024 at the Lions Eye Institute in Perth, Western Australia. We included patients born between 1930–1975. A height adjustment was applied by multiplying the average increase in axial length per cm of height by the relative change in the mean height of Australian adults since 1930. We report results for the 25th, 50th, and 75th percentiles.
For patients born 1945 or earlier vs 1946 or later, median height-adjusted axial length was 23.19 mm vs 23.35 mm for females (p<0.001) and 23.78 mm vs 23.95 mm for males (p<0.001).
In this cross-sectional clinic-based sample of Australian adults, median axial length increased over time while the distribution became increasingly positively skewed. For the bottom quartile, axial length remained relatively stable but, for the top quartile, axial length increased by >1.1 mm for patients born 1930–1975. These results are consistent with our earlier study that myopia rates have increased in Australian adults. While myopic adults are likely over-represented in this clinic-based sample relative to the whole population, we found remarkably similar results when restricting to patients aged 60 years or older, who were more likely to be attending for cataract surgery and therefore more representative of the broader population.
This study could be replicated in any large eye clinic with access to axial length measurements.
We predict that as normal values for axial length are established, individual axial length data will become incorporated into myopia treatment decisions for children, in an effort to improve vision and prevent further increases in population levels of myopia.
Professor David Mackey AO MBBS MD FRANZCO FRACS FAHMS FARVO is an internationally renowned clinician, scientist, and academic. He is Professor of Ophthalmology at University of Western Australia and was the Lions Eye Institute’s Managing Director from 2009 until 2018.
Dr Samantha Lee completed her PhD in 2017 at the Queensland University of Technology. She is a Senior Research Fellow at the Lions Eye Institute and the University of Western Australia. She has published more than 50 peer-reviewed articles, with her current research focussing on the genetics and epidemiology of glaucoma and myopia.
Dr Gareth Lingham MOrth PhD is a Postdoctoral Research Fellow at the Lions Eye Institute, a Clinical Data Analyst with Ocumetra, and holds adjunct positions with Technological University Dublin and the Centre for Eye Research Australia.
References
1. The Nobel Prize organisation, Allvar Gullstrand Facts. Available at nobelprize.org/prizes/medicine/1911/gullstrand/facts [accessed June 2025].
2. Mundt GH Jr, Hughes WF Jr. Ultrasonics in ocular diagnosis. Am J Ophthalmol. 1956 Mar;41(3):488-98. doi: 10.1016/0002-9394(56)91262-4.
3. Scholtz SK, Langenbucher A, Stachs O. Celebrating 25 years of optical biometry: A milestone in ophthalmology. Klin Monbl Augenheilkd. 2024 Dec;241(12):1298-1301. English. doi: 10.1055/a-2428-8007.
4. Nilagiri VK, Lee SS, Mackey DA, et al. Distribution of axial length in Australians of different age groups, ethnicities, and refractive errors. Transl Vis Sci Technol. 2023 Aug 1;12(8):14. doi: 10.1167/tvst.12.8.14.
5. Lee SS, Nilagiri VK, Mackey DA, et al. Myopia progression following 0.01% atropine cessation in Australian children: Findings from the Western Australia - Atropine for the Treatment of Myopia (WA-ATOM) study. Clin Exp Ophthalmol. 2024 Jul;52(5):507-515. doi: 10.1111/ceo.14368.
6. Mackey DA, Lingham G, Yazar S, et al. Change in the prevalence of myopia in Australian middle-aged adults across 20 years. Clin Exp Ophthalmol. 2021 Dec;49(9):1039-1047. doi: 10.1111/ceo.13980.