mieyecare

Myopia Management
Data Revealing Observations
Analysis of data from 287,958 Specsavers appointments for myopic children since 2016 has revealed significant trends, insights, and lessons in disease management, writes Dr Joseph Paul, Head of Professional Services at Specsavers ANZ.
WRITER Dr Joseph Paul
Myopia, often known as near sightedness, is one of the most common eye conditions in young children. According to the International Myopia Institute, myopia is defined as a spherical equivalent refraction of -0.50D or less in one or both eyes, with high myopia being -6.00D or less. This condition can significantly impact a person’s quality of life, making distant objects appear blurry while close objects remain clear. It also makes one more susceptible to eye conditions later in life including retinal detachment, glaucoma, and cataracts.
Myopia prevalence is increasing around the world, with reported rates of myopia seen among children and young adults increasing over time, particularly in South East Asian countries.1-3It is often reported that by 2050, 50% of the world’s population will be myopic and 10% highly myopic.4 This is a concerning potential future, albeit one that may be avoided if the eye care profession continues to advance myopia management as the standard of care for young myopes.
In Australia and New Zealand, the situation is similar, and so much of a growing concern that Specsavers has been monitoring and sharing its insights on myopia and myopia treatment for a number of years. As we learn more about these trends in myopia and myopia management, we will continue to share them with the industry, with the ambition being to drive improved care for patients across the sector.
FINDINGS
Recently, we reviewed data from 287,958 Specsavers appointments for myopic children since 2016 to further understand trends in myopia and myopia management in Australia.
Overall, we were not surprised to find that the increasing prevalence of myopia is compounded by the increased severity with which children are first presenting to optometrists.
By examining trends in patient data, we observed that the average spherical equivalent (SE) refraction for first-time myopic patients under the age of 15 nearly doubled, increasing from -0.91D in 2016 to -1.79D in 2024. SE measures the overall refractive power of the eye and is crucial for assessing vision quality. These findings indicated that children are presenting with higher degrees of myopia at an earlier age.
When looking at the most myopic eyes of these children, the same trend is seen, increasing from -1.03D to -1.99D. As every dioptre of myopia significantly increases the lifetime risk of visual impairment,5 this increase in myopia at first presentation is a potentially concerning development.
These results are displayed in Figure 1, where the dark green line indicates the most myopic eye, and the light green line indicates the average SE refraction. This data highlights the urgent need for effective myopia management strategies to prevent long-term vision impairment.
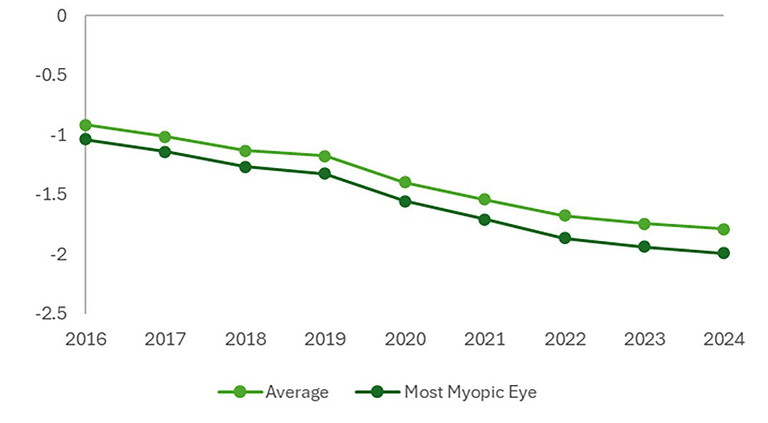
Figure 1. Myopic spherical equivalent refraction at first presentation.
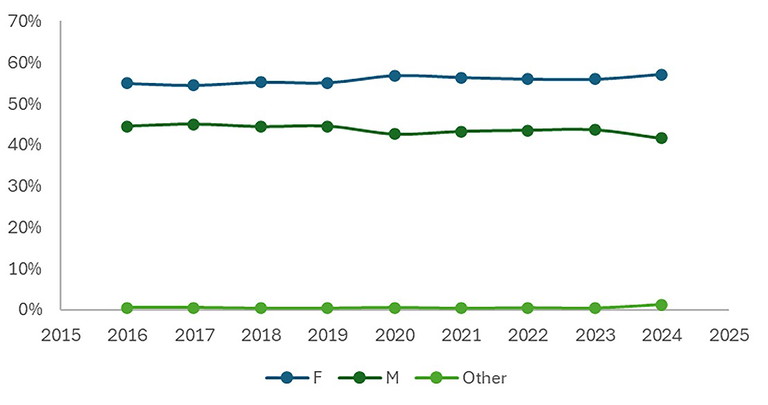
Figure 2. Gender of first-time myopic patients.
DEMOGRAPHICS
Examining demographic factors, we found that first-time myopic patients presenting to our Specsavers practices were more likely to be female than male. Since 2016, this gender disparity has increased slightly, with a further increase in the proportion of female first-time myopic patients: in 2016, 54.9% of first-time myopic patients were female, and by 2024, this figure had risen slightly to 57.1% (Figure 2).
Although further research is needed, as prior studies have shown varying correlations between gender and myopia,6,7 these findings suggest a trend towards a higher prevalence of myopia among females.
MYOPIA MANAGEMENT
While myopia management is seen as the gold standard of care,8 and Australian practitioners are considered among the most proficient and willing providers of myopia management,9 accurate data on the uptake of myopia management modalities among myopic children at the population level has historically been difficult to obtain.
At Specsavers, we have only recently been able to observe population-level trends as myopia management has become more commonplace and as our data analysis capabilities have evolved.
In 2023, when we first were able to capture the information, 18.21% of myopic children were engaged in active myopia management prescribed by their optometrist. Of these, 45.2% were using spectacle lenses, 29.6% were using contact lenses, and 25.2% were prescribed atropine drops.
Since then, Specsavers has invested significant time and resource into optometrist and dispenser education, supplier procurement, and myopia awareness campaigns. The results are evident in Figure 3.
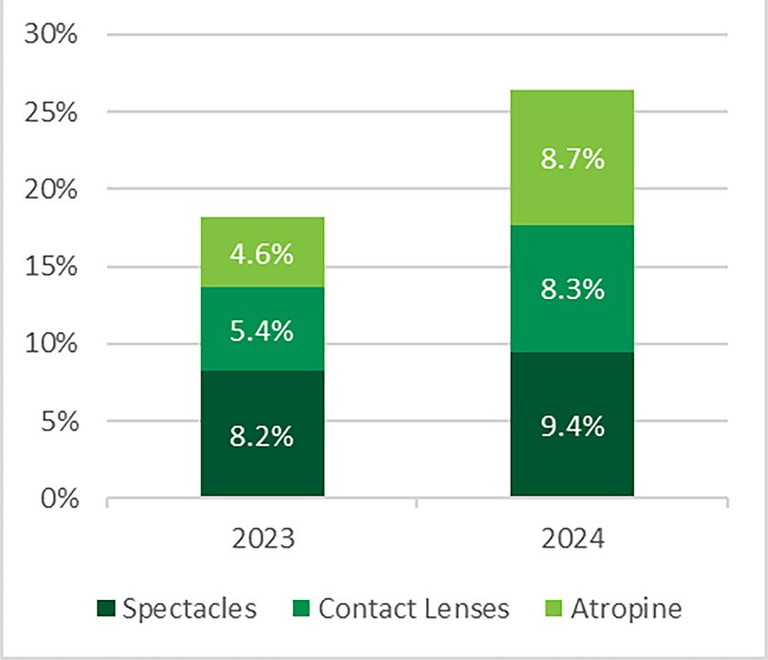
Figure 3. Myopic children in treatment.
An increase of just over 8% in the uptake of myopia management to 26.4% of children was seen among all treatment modalities, although interestingly, the largest increase was seen in atropine use. This resulted in a more even split between the three treatment modalities, with contact lenses being worn by 31.7% of patients in active management, atropine used by 33.0%, and spectacle lenses by 35.7%.
Several factors could contribute to this increase in atropine usage, including additional research showing its efficacy at various doses across multiple populations, and the widespread availability of commercial atropine preparations.
It is important to highlight that this work does not include orthokeratology (OK) as a form of active management of myopia. OK is a nonsurgical procedure where a specific type of rigid gas-permeable contact lens is worn at night to gently and temporarily reshape the cornea. This has not been included due to a significantly lower availability of highquality data on the use of OK as a modality of myopia in clinical practice. It also does not include other forms of myopia management that are being used by optometrists, such as single vision, bifocal or multifocal lenses as a form of myopia management, as these have shown to have a lesser effect on the progression of myopia than myopiamanagement specific lenses such as defocus incorporated multiple segments (DIMS) or highly aspherical lenslet target (HALT) lenses, and contact lenses such as MiSight.10-12
NEXT STEPS
While myopia is increasing in children in Australia, we can see that the use of myopia management is too, with at least one in four myopic children seen in 2024 at Specsavers actively engaged in myopia management. This is encouraging but also highlights the need to continue work in this field to reduce the impact of myopia, ensuring we protect the sight of future generations.
As a part of our purpose to change lives through better sight and hearing, Specsavers will continue to educate parents and carers of children on the importance of eye tests in early years, and help to improve awareness of myopia among this audience.
Additionally, to lower the risks of young myopes developing more serious vision-impacting diseases in the future, Specsavers will continue to focus on educating optometrists, dispensers, patients, and their families about the various myopia management techniques.
“An increase of just over 8% in the uptake of myopia management… was seen among all treatment modalities, although interestingly, the largest increase was seen in atropine use”
Dr Joseph Paul BOptom PhD studied optometry at the University of Melbourne, graduating in 2011. He then completed a PhD in retinal structure and function at the University of Melbourne and a post-doctoral position in optic nerve bioenergetics at the Centre for Eye Research Australia. Alongside this work, Dr Paul has practised in a wide range of public, private and corporate optometry practices across Victoria over the past decade. He is currently Head of Professional Services at Specsavers Australia and New Zealand.
References
1. Rudnicka AR, Kapetanakis VV, Owen CG. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016 Jul;100(7):882-890. doi: 10.1136/bjophthalmol-2015-307724.
2. Dong L, Kang YK, Jonas JB, et al. Prevalence and time trends of myopia in children and adolescents in China: A systemic review and meta-analysis. Retina. 2020 Mar;40(3):399-411. doi: 10.1097/IAE.0000000000002590.
3. Grzybowski A, Kanclerz P, Saw SM, et al. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020 Jan 14;20(1):27. doi: 10.1186/s12886-019-1220-0.
4. Holden BA, Fricke TR, Resnikoff S, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016 May;123(5):1036-42. doi: 10.1016/j.ophtha.2016.01.006.
5. Bullimore MA, Ritchey ER, Flitcroft DI, et al. The risks and benefits of myopia control. Ophthalmology. 2021 Nov;128(11):1561-1579. doi: 10.1016/j.ophtha.2021.04.032.
6. Alvarez-Peregrina C, Martinez-Perez C, Sánchez-Tena MÁ, et al. on behalf of Grupo de Investigación Alain Afflelou. The prevalence of myopia in children in Spain: An updated study in 2020. Int J Environ Res Public Health. 2021 Nov 25;18(23):12375. doi: 10.3390/ijerph182312375.
7. Matsumura S, Dannoue K, Hori Y, et al. Prevalence of myopia and its associated factors among Japanese preschool children. Front Public Health. 2022 Jun 22;10:901480. doi: 10.3389/fpubh.2022.901480.
8. Dahlmann-Noor AH, Ghorbani-Mojarrad N, Young AL, et al. 2024 UK and Ireland modified Delphi consensus on myopia management in children and young people. Ophthalmic Physiol Opt. 2024 Nov;44(7):1368-1391. doi: 10.1111/opo.13381.
9. Wolffsohn JS, Whayeb Y, Logan NS, Weng R; International Myopia Institute Ambassador Group. IMI-global trends in myopia management attitudes and strategies in clinical practice-2022 update. Invest Ophthalmol Vis Sci. 2023 May 1;64(6):6. doi: 10.1167/iovs.64.6.6. Erratum in: Invest Ophthalmol Vis Sci. 2023 May 1;64(5):12. doi: 10.1167/iovs.64.5.12.
10. Lam CS, Tang WC, To CH, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363-368. doi: 10.1136/bjophthalmol-2018-313739.
11. Bao J, Huang Y, Chen H, et al. Spectacle lenses with aspherical lenslets for myopia control vs single-vision spectacle lenses: A randomized clinical trial. JAMA Ophthalmol. 2022 May 1;140(5):472-478. doi: 10.1001/jamaophthalmol.2022.0401.
12. Chamberlain P, Peixoto-de-Matos SC, Young G, et al. A 3-year randomized clinical trial of MiSight lenses for myopia control. Optom Vis Sci. 2019 Aug;96(8):556-567. doi: 10.1097/OPX.0000000000001410.