mitechnology
Managing Glaucoma:
Quest for Efficient Visual Field Analysis
Visual field tests with increased diagnostic accuracy and shorter durations can improve the quality of care in glaucoma. The Henson 9000 perimeter utilises unique testing strategies to optimise visual field analysis.
WRITER Dr Catharine Chisholm
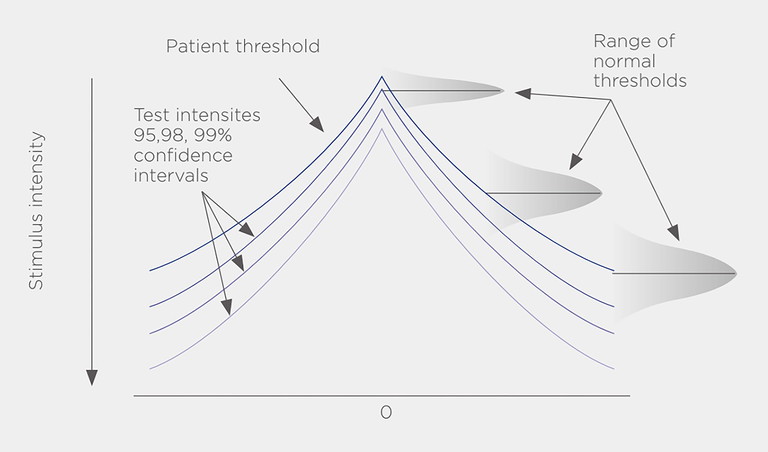
Figure 1. Stimulus intensities of the Smart Supra test based on 95, 98, and 99% probability of being seen by an age-matched eye with no visual field loss.
BARRIERS TO EFFECTIVE GLAUCOMA DETECTION
Globally, glaucoma is the second leading cause of blindness and the leading cause of irreversible blindness in patients aged 50 years and older.1 Standard automated perimetry (SAP) is recommended for monitoring of glaucomatous visual field damage;2 however, the intrinsic test-retest variability of SAP3 and the variable rates of glaucoma progression among patients4,5 necessitate repeated visual field testing to accurately detect progression and to identify rapid progressors in a timely manner.6,7
The European Glaucoma Society (EGS) recommends thrice yearly visual field tests for the first two years after diagnosis.8 However, the frequency of testing reported in clinical practice often falls short of the recommended guidelines.9,10
This can be attributed to patients finding frequent visual field testing tiresome, as the prolonged mental effort required is viewed unfavourably by patients.11 Evidently, visual field tests need to be shorter and more convenient for patients to effectively monitor progression. A better patient experience during perimetry can increase measurement reliability and improve adherence to the recommended frequency of testing. The time-consuming nature of visual field testing also hinders efficient case finding. A substantial proportion of glaucoma cases worldwide remain undiagnosed, as patients typically do not present to the clinic until relatively late in the disease course.12,13 If the current rate of diagnosis remains unchanged, it is projected that around 67 million people will have undetected glaucoma by 2040.13 To tackle the vast burden of undiagnosed glaucoma in the community, testing needs to be proactive. This requires visual field tests that are quick enough to perform on a large proportion of patients, while still maintaining good sensitivity and specificity to avoid false positive diagnoses.
Therefore, innovations in perimetry are focussed on reducing the duration of visual field examination without compromising diagnostic accuracy.14
Although several testing algorithms in various perimeters have been introduced to decrease test times, the currently available visual field tests have three main limitations:
1. High variability at moderate to severely damaged test locations.
Visual field locations with low sensitivities have limited informational value, as the response variability at individual test locations increases with decreasing sensitivity, making it difficult to discern true progression from a random change in sensitivity due to chance.15,16 This reduces the reliability of the measurements obtained. In locations with sensitivity worse than 10 dB, the response probability does not increase with increasing stimulus intensity, and perimetric sensitivities beyond this cutoff have little correlation with true functional status.16 Repeated testing of such locations to determine accurate sensitivity estimates prolongs test durations without adding to the diagnostic power of the test.17
2. Poor sensitivity to small central defects when testing with the 24-2 visual field test.
The 24-2 test pattern is the most frequently used perimetric testing pattern, covering an area within 24° from the point of fixation, with a regular 6° grid consisting of 54 test locations. However, only four of these test locations lie within 8° of fixation (the macular region).18 Due to inadequate sampling of the macula, 24-2 tests may miss early glaucomatous macular damage when compared to the 10-2 test, which has a 2° grid with greater sampling density in the central 8°.19 In a prospective multicentre study, 61% of eyes with early glaucoma had central field defects on 10-2 tests that were missed on 24-2tests.20 In another study, 52% of eyes with macular damage were missed by 24-2 test metrics.18 Since initial glaucomatous damage can involve the macular region,19 patients with significant glaucomatous damage, due to isolated central visual field loss, can be misdiagnosed as pre-perimetric glaucoma if relying on 24-2 testing alone.
3. Long test times are further prolonged with the inclusion of more test locations.
The sensitivity and specificity of visual field tests can be increased by the inclusion of additional testing locations.21–23
The diagnostic precision of perimetry increases exponentially with the number of locations tested.22 However, testing more locations also extends test durations,23 which can introduce perimetric fatigue effects. Sensitivity estimates have been observed to decline with increasing test duration due to loss of vigilance in patients;24,25 this can lead to increased measurement variability with prolonged testing.
OPTIMISED PERIMETRY WITH THE HENSON 9000
The Henson 9000 is the newest iteration of the long-standing Henson perimeter that aims to address the aforementioned limitations of existing visual field tests. Its testing algorithms are uniquely designed to improve operator efficiency and patient comfort during perimetry, both for monitoring progression and for case detection through population screening.
THE SMART SUPRA TEST
SAP can be classified as threshold or suprathreshold perimetry. In threshold perimetry, a limited number of locations are tested repeatedly with light stimuli, in an adaptive staircase sequence, imparting greater resolution of sensitivity information and providing threshold values that can be tracked over time. In suprathreshold perimetry, a greater number of locations are tested with a light stimulus of a suprathreshold intensity. If stimulus is seen, it is assumed that no significant defect exists, and testing is discontinued at that location. A reduced number of presentations at more locations shortens test durations and provides high-resolution spatial information about visual field defects.26
The Henson 9000 features the Smart Supra test, which performs suprathreshold perimetry at 30 carefully selected locations to screen for glaucomatous damage. Effective screening can be performed with only 30 test locations due to the use of an intelligent test pattern, based on a detailed analysis of the locations most likely to be affected in the early stages of glaucoma.27
If a defect is detected, however small, the Smart Supra auto-extends to a total of 64 test locations (equivalent to the 24-2 with 10 additional central points) and can be manually extended to include an additional 22 locations in the central 10°, for a total of 86 locations.
The additional sampling of 22 locations in the central 10° provides greater sensitivity to small, central defects, as compared to the 24-2visual field test that samples only 12 locations in the same region.
The 30-point test can be completed in under a minute while the 86-point extension where required, can be completed in around 3.5 minutes. Rapid testing is achieved, even with the increased number of test locations, as the tests can be extended in the event of a screening failure without having to start a separate test. The initially acquired information is built upon without re-examining already tested locations.
This keeps test durations short for patients at low risk of glaucoma and enhances clinic workflow.
Smart Supra also maximises diagnostic precision by setting stimulus intensity increments according to the normal variability observed at each test location.
An in-built age-normative database is used to derive probability-based increments which have a 95, 98, and 99% probability of being seen (Figure 1), improving reliability as a result. Possible false positive results are minimised by automatically repeating any missed stimulus, marking it as missed only if missed twice in the same test. The operator can manually retest locations and test additional locations clustered around a missed point, further reducing false positives to improve the specificity of the screening test, and increasing confidence that any defect detected is genuine.
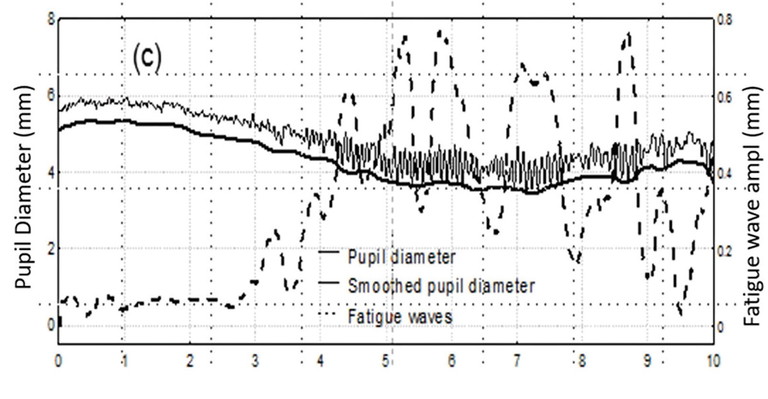
Figure 2. Pupillary fatigue waves (dotted line) and pupillary diameter (solid lines) plotted against duration of perimetric test in minutes, showing increase in amplitude of fatigue waves with longer test duration. Reproduced with permission from Invest Ophthalmol Vis Sci. 2010 Jul;51(7):3540-3.
THE ZATA THRESHOLD TEST
The Zippy Adaptive Threshold Algorithm (ZATA) of the Henson 9000 is a threshold testing algorithm that uses Bayesian methods similar to the Swedish Interactive Thresholding Algorithm (SITA) of the Humphrey Field Analyser. ZATA uses the same stimulus, background luminance, testing locations (24-2 or 30-2 test patterns), and decibel scale as that of Humphrey perimetry. However, the ZATA test features a few additional optimisations to reduce test times:
Use of prior test data: If patients have been tested previously, ZATA can utilise prior threshold values to set starting stimulus intensities closer to patients’ actual thresholds, as compared to supraliminal starting stimuli or age-normative threshold values used in other perimeters.
This reduces test times and attenuates patients’ anxiety by reducing the number of unseen presentations early in the test. The ZATA 24-2 test can be completed in about three minutes per eye for an eye with limited visual field loss, thus avoiding fatigue due to loss of attention that is observed to occur after approximately three minutes of perimetric testing (Figure 2).28
Variable terminating criteria: ZATA utilises stricter terminating criteria at damaged and neighbouring locations, while terminating criteria are looser for severely damaged locations (<10 dB), where high response variability yields limited useful data. Focussing stimulus presentations on less damaged locations can obtain reliable sensitivity information while reducing test times for patients with advanced glaucomatous damage. Stimulus presentations are conserved for use at all but the most damaged locations, thereby obtaining more accurate thresholds and increasing reliability.
“The Henson 9000 generates data in a globally recognised format for easy comparison with other perimeters”
Elimination of testing at highly damaged locations also reduces the number of unseen presentations, which minimises anxiety and improves the testing experience for patients.
In an initial clinical study, perimetry with ZATA Standard reduced test durations by up to 30% compared to the SITA standard test. Testing duration was also shortened in eyes with severe visual field damage.29 Test-retest variability of mean deviation values with ZATA was similar to that of SITA tests, and the differences between both tests appeared to be similar to random differences due to test-retest variability. Visual field defects were represented similarly, and the reports generated were closely comparable.
‘Extend’ facility enabling both 24-2 and 30-2test patterns in a single test: If required, the ZATA 24-2 test can be extended to a 30-2 test pattern, either during or at the end of each test, without needing a retest of the already examined 24-2 locations.
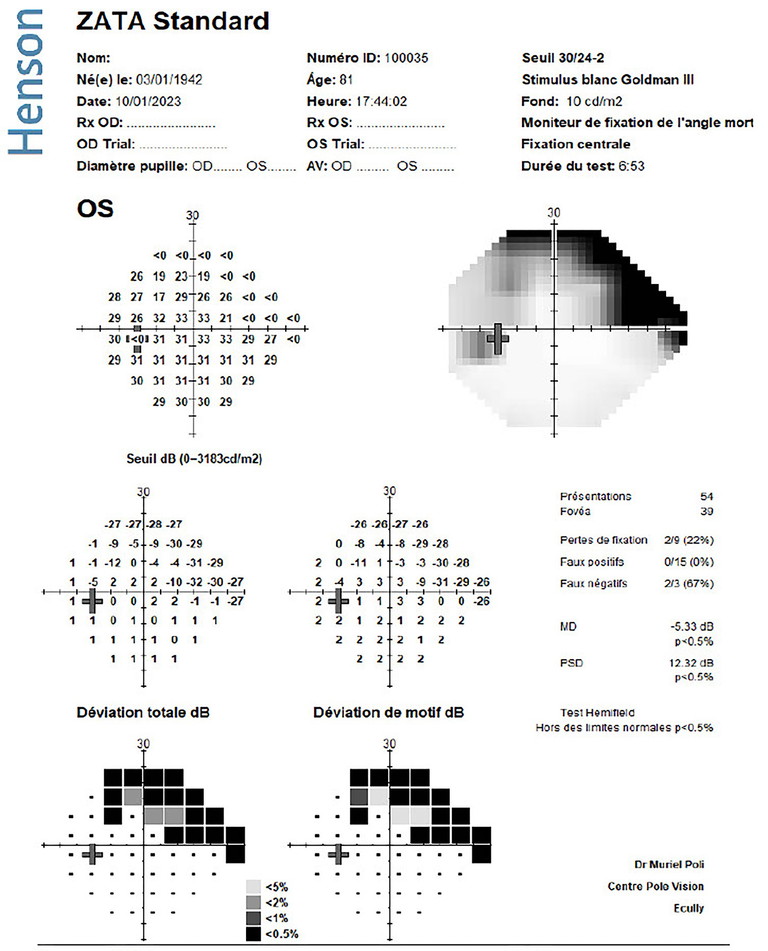
Figure 3. ZATA Standard printout showing threshold, grayscale, total deviation, and pattern deviation plots, with universally recognised reliability indices (fixation losses, false positives, false negatives) and global indices (mean deviation, pattern standard deviation, and the Glaucoma Hemifield Test). Image provided by Dr Muriel Poli MD PhD.

Figure 4. The Henson 9000 perimeter.
INTEGRATION INTO CLINICAL PRACTICE
The Henson 9000 generates data in a globally recognised format for easy comparison with other perimeters. Smart Supra printouts include pattern and total deviation probability maps, similar to those of threshold tests, and ZATA reports feature all globally accepted indices (mean deviation, pattern standard deviation and hemifield) in addition to threshold and grayscale, total deviation and pattern deviation values (Figure 3). The Henson 9000 is also equipped with a full suite of analytical tools, including progression analysis.
The Henson 9000 has a compact and ergonomic design with a small footprint (Figure 4) that allows flexible positioning of the perimetrist with respect to the device, even in clinics with space constraints. It has an intuitive, multilingual user interface that minimises staff training time, and a Windows-based database that provides networking capabilities without the need to purchase additional software.
Files can be stored on a network drive and shared between devices. The Henson software can also be linked to practice management systems for transfer of prior patient data to the Henson tests. Online operator training materials are also available.
APPLICATIONS IN GLAUCOMA DIAGNOSIS
The Henson 9000 improves testing experience during perimetry by reducing patient anxiety and fatigue, with strategies designed to prevent unnecessary prolongation of test durations. Increased sampling of the macula and elimination of testing at severely damaged locations ensure high diagnostic sensitivity, specificity, and reliability, even with faster testing speeds.
Rapid multiple-point testing with Smart Supra can facilitate routine screening of glaucoma without disrupting clinic workflow, enabling asymptomatic patients to be diagnosed early.
Shorter test times with ZATA will allow more frequent testing for detection and monitoring of glaucoma, which will guide clinicians in providing appropriate therapy. Initial clinical studies have shown the potential of the Henson 9000 perimeter as a promising solution to the challenges faced in the diagnosis of glaucoma.
This article is sponsored by Topcon Health.
Dr Catharine Chisholm PhD MCOptom FBCLA earned a degree in optometry at the University of Manchester and completed her PhD at City University, London. She held various lectureships in the United Kingdom before being appointed as the Director of Global Training, leading Topcon Healthcare University. This initiative supports eye care practitioners to optimise their use and understanding of cutting-edge ophthalmic technology through the provision of education and training.
References available at mivision.com.au.