Surgical Preferences Revealed: AUSCRS
Delegates at the Australasian Society of Cataract and Refractive Surgeons (AUSCRS) conference in Darwin have contributed to a short survey, offering an illuminating snapshot of how refractive surgery is evolving across Australia and New Zealand.
The 2025 Refractive Surgery Trends Survey captured the preferences, practices, and opinions of delegates who attended the conference in Darwin. The cohort consisted predominantly of Australian ophthalmologists, however, did include a few international guests. Approximately 50% of attending surgeons responded to the survey. Survey results are not the opinion of the AUSCRS committee, but rather a snapshot of the surgical preferences of the group. The results reveal a field that is both adopting new technologies and maintaining trusted approaches, with some intriguing shifts in clinical behaviour.
CATARACT SURGERY: PRECISION MEETS PRAGMATISM
Cataract surgery remains a central part of practice for most surgeons. Annual case volumes ranged from under 200 for 23% of respondents, to between 500 and 1,000 for 32%, with 11% being “high volume cataract surgeons” performing over 1,000 procedures a year.
WRITER Dr Anton van Heerden
Femtosecond laser-assisted cataract surgery (FLACS) remains contentious:
• 57% acknowledge some clinical benefit but feel cost outweighs advantages,
• 30% see it purely as a marketing tool, and
• Only 13% believe it is safer and more accurate.
When it comes to intraocular lens (IOL) choices, 36% use toric lenses in over 75% of cases, while uptake for trifocals remains modest, with 66% only using them in fewer than 25% of cases. Extended depth of focus IOL adoption is more evenly spread, but 40% use them in fewer than 25% of cases.
Notably, 87% of surgeons routinely use intracameral antibiotics.
LASER VISION CORRECTION: MATCHING PROCEDURE TO PRESCRIPTION
The survey revealed 55% of the cohort offer laser vision correction services. The preferred surgical options vary quite considerably in the group:
• Patients with moderate myopia: 50% prefer keratorefractive lenticule extraction (Klex) including small incision lenticule extraction (SMILE), corneal lenticule extraction for advanced refractive correction (CLEAR), SmartSight, and smooth incision lenticule keratomileusis (SILK), while 46% favour laser-assisted in situ keratomileusis (LASIK).
• Patients with low myopia: LASIK leads at 48%, with photorefractive keratectomy (PRK) and Klex tied at 25%.
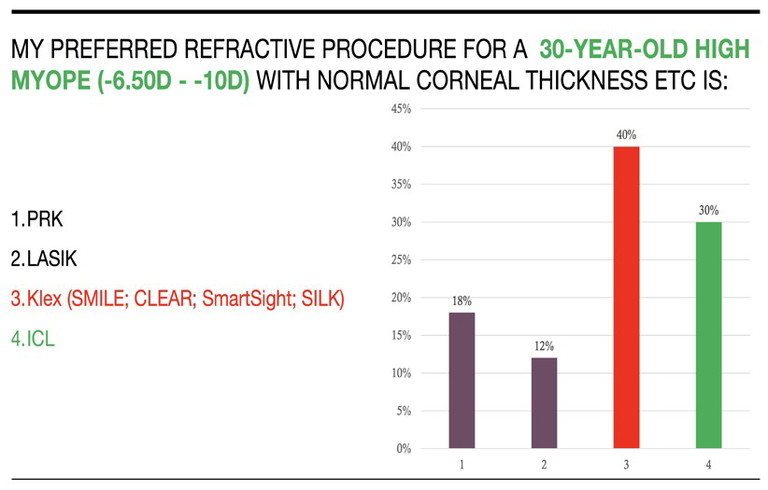
• Patients with high myopia: 40% choose Klex, 30% opt for implantable collamer lenses (ICLs).
• Patients with hyperopia: LASIK dominates at 60%, with smaller shares for ICL, Klex, and refractive lens exchange (RLE)/clear lens exchange (CLE).
PRESBYOPIA: DIVIDED PREFERENCES
In hyperopic presbyopes, preferences were almost evenly split:
• 35% choose RLE with EDOF IOLs,
• 33% favour PresbyLASIK, and
• 32% prefer RLE with trifocals.
In myopic presbyopes, the corneal approach dominates: 66% opt for PresbyLASIK, with just 10% selecting RLE with EDOF lenses.
ICLS: EXPANDING ROLE, PERSISTENT BARRIERS
ICLs are viewed positively by most surgeons:
• 82% consider them a good option for patients unsuitable for laser vision correction (LVC), and
• 14% go further, regarding them as safer than LVC.
For 74% of respondents, cost to patients remains the primary barrier to ICLs, followed by technical support (15%), and perceived surgical risk (9%).
In terms of surgical practice, 47% always perform bilateral same-day ICL implantation, while 44% prefer separate days. Sizing is split between white-to-white measurements (51%) and anterior segment optical coherence tomography (47%).
IMPLICATIONS FOR OPTOMETRY
For optometrists, these findings underline the need to remain up to date with surgical innovations and preferences. Whether comanaging cataract patients considering EDOF IOLs, or advising a young high myope on refractive options, understanding current surgeon trends enables better patient guidance and expectation management.
BOTTOM LINE
The AUSCRS 2025 Refractive Surgery Trends Survey shows a profession in transition – balancing innovation with pragmatism, embracing new technologies where they add value, and refining patient selection. For patients, it means more personalised solutions than ever. For optometry, it’s a call to maintain an active dialogue with surgical colleagues as the refractive landscape continues to evolve.
The intention is to do this study on an annual basis to assess the changes in cataract and refractive surgery practices.
Dr Anton van Heerden MBChB FRANZCO WCRS is a cataract and refractive surgeon based in Melbourne. He is a Director of Eye Laser Specialists, Armadale Eye Clinic and Mornington Peninsula Eye Clinic.